Abstract
In males, androgens are essential in maintaining the integrity of the prostate. Androgen-ablation induces apoptosis of the prostatic epithelium. In females, ovariectomy induces apoptosis in uterine epithelium while progesterone inhibits this process. The objective of this study was to determine whether androgen and progesterone inhibit apoptosis, respectively, in mouse prostatic and uterine epithelia via steroid receptors in the epithelium or in the stroma. To address this question, prostatic tissue recombinants were prepared with rat urogenital sinus mesenchyme plus bladder epithelium from wild-type or testicular feminization mutant (Tfm) mice. Thus, prostatic tissue was generated having androgen receptor (AR) in both epithelium and stroma or in the stroma only. Castration of hosts induced apoptosis in the AR-negative Tfm prostatic epithelium with an epithelial apoptotic index virtually identical to prostatic tissue recombinants containing wild-type epithelium. Moreover, this castration-induced prostatic epithelial apoptosis was blocked by testosterone and dihydrotestosterone in both wild-type and Tfm prostatic tissue recombinants. Likewise, uterine tissue recombinants were prepared in which epithelium and/or stroma was devoid of progesterone receptor (PR) by using uterine epithelium and stroma of wild-type and PR knockout mice. Progesterone inhibited uterine epithelial apoptosis only in tissue recombinants prepared with PR-positive stroma. The PR status of the epithelium did not affect epithelial apoptotic index. Therefore, the apoptosis in prostatic and uterine epithelia is regulated by androgen and progesterone via stromal AR and PR, respectively. In both cases, epithelial AR or PR is not required for hormonal regulation of epithelial apoptosis in prostatic and uterine epithelium.
Similar content being viewed by others
Introduction
Both male and female reproductive tissues show dramatic growth and regression during reproductive cycles. Steroid hormones, androgen in males and 17-β estradiol (E2) and progesterone (P4) in females, are key regulators of these growth/regression cycles. Studies of epithelial apoptosis in male1 and female,2,3 reproductive tracts have demonstrated that epithelial apoptosis in steroid target organs is under the control of steroid hormones. In the male, the prostate is dependent on androgens for growth, function and maintenance of tissue architecture.4 Androgen deprivation elicited by physiological or chemical castration induces apoptosis in prostatic epithelium of rats and mice. In the rodent ventral prostate, epithelial apoptosis reaches its maximum 3 days after castration.4,5 In females, apoptosis plays an important role in regulating functions in the reproductive tract, and is regulated by two ovarian steroid hormones, E2 and P4. E2 is mitogenic for uterine epithelium, while P4 inhibits proliferation and apoptosis of uterine epithelium.6,7 Increased systemic levels of E2 at the proestrus/estrus-phases induces growth of uterine tissue. The integrity of the uterus is maintained in part by P4, which prevents cell death. If pregnancy is not established, the level of P4 drops, and uterine epithelial tissue regresses via apoptosis.8 This prolifertive/apoptotic cycle in uterine epithelium can be mimicked in ovariectomized mice by a hormone treatment protocol with P4 and E2.6,7
Steroid hormone action is mediated via nuclear receptor proteins, which function as ligand modulated transcription factors.9 Androgen and P4 signals are mediated through the androgen receptor (AR) and progesterone receptor (PR), respectively. Many genes are regulated by steroid hormones, and it has been tacitly assumed that hormonal effects on a cell are mediated through receptors in the responding cell. However, hormone target organs such as the prostate and uterus express steroid receptors in both epithelial and stromal cells.10,11 The importance of paracrine mechanisms in steroid hormone action in male and female reproductive tracts has been well established. For example, proliferation of normal epithelial cells induced by steroids in male and female reproductive tracts appears to be regulated via paracrine mediators produced by stromal cells. The idea that epithelial proliferation is regulated in vivo by paracrine mechanisms is based upon several lines of evidence: (a) E2 and testosterone (T) are not mitogenic when applied to primary cultures of normal target epithelial cells.12,13 (b) Mitogenicity of E2 for uterine and vaginal epithelia is reconstituted when cultured epithelial cells are recombined with stroma, and the tissue recombinants are grafted in vivo.14 (c) Androgen stimulates proliferation of Tfm prostatic epithelium, which is devoid of functional AR, in prostatic tissue recombinants made with Tfm epithelium plus wild-type stroma.15 (d) Uterine and vaginal tissue recombinants composed of ERα-negative epithelium derived from ERα knockout mice and ERα-positive wild-type stroma demonstrate conclusively that mitogenicity of estrogen in normal uterine and vaginal epithelia is dependent upon ERα in the stroma in vivo.16,17 Epithelial ERα is neither necessary or sufficient for the mitogenicity of estrogen in normal target epithelial cells in vivo. Similar evidence has been demonstrated for anti-mitogenic effect of P4 for uterine epithelium.18 P4 inhibits E2-induced uterine epithelial DNA-synthesis in PR-negative epithelium from PRKO mice when the epithelial cells are combined with PR-positive uterine stroma from wild-type mice. In contrast, P4 does not block E2-induced DNA-synthesis in PR-positive uterine epithelium combined with PR-negative uterine stroma.18 Thus, in all cases epithelial steroid receptors are not required for the regulation of proliferation of normal epithelial cells in vivo. Paracrine mechanisms are also involved in the regulation of lactoferrin expression by E219 and P420 in uterine epithelium, and regulation of uterine epithelial PR by E221 and P4.20 These facts raise the possibility that the apoptosis of epithelial cells in male and female reproductive tracts may also be regulated by steroid hormones through paracrine mechanisms.
In this study we report a paracrine mechanism for regulation of apoptosis in prostatic and uterine epithelia. To study the respective roles of epithelial versus stromal steroid receptors in the anti-apoptotic action of androgen on prostatic epithelium and P4 on uterine epithelium, tissue recombination techniques were utilized. Since stromal AR is essential for the development of prostate,22 we could not make prostatic tissue recombinants with AR-negative stroma. To demonstrate whether epithelial AR is required for the regulation of prostatic epithelial apoptosis, bladder epithelium (BLE) was combined with urogenital sinus mesenchyme (UGM) which result in prostatic induction.23 If the BLE is derived from wild-type mice, the resultant induced prostatic epithelium expresses many markers indicative normal prostatic epithelium including prostatic specific secretory proteins,24 Nkx3.125 and AR.23 If Tfm bladder is combined with wild-type UGM prostatic ducts also form and the induced Tfm prostatic epithelium expresses Nkx3.125 and proliferates in response to androgen even though the Tfm prostatic epithelium does not express prostatic secretory proteins due to lack of epithelial AR.15,24 To determine the role of stromal versus epithelial AR in prostatic epithelial apoptosis, prostatic tissue recombinants were prepared with BLE of Tfm and wt mice combined with rat UGM. The induced prostatic tissue expressed AR in both its epithelium (E) and stroma (S) in wt-S+wt-E tissue recombinants, or only in stroma but not the epithelium in wt-S+Tfm-E tissue recombinants. Likewise, to determine whether P4 inhibits uterine epithelial apoptosis via epithelial versus stromal PR, 4 types of tissue recombinants were prepared with uterine stroma (S) and epithelium (E) from wild-type (wt) and PR knockout (PRKO) mice: wt-S+wt-E, wt-S+PRKO-E, PRKO-S+wt-E and PRKO-S+PRKO-E.
Results
Prostatic epithelial apoptosis induced by androgen-withdrawal in androgen receptor null prostatic epithelium
In intact male mice, very few apoptotic cells were observed in the epithelium of the ventral (Figure 1c) and dorsolateral lobes of prostate, and the apoptotic index (derived from terminal deoxynucleotidyltransferase dUTP nick end labeling [TUNEL] stained specimens) was low in the ventral prostate (VP) and dorsolateral prostate (DLP) (Table 1). Castration induced apoptosis of prostatic epithelium in both VP (Figure 1a,b,d) and DLP (not shown). At 3 days after castration, the epithelial apoptotic index significantly increased from that of intact mice in both VP and DLP with epithelial apoptotic index being significantly higher in VP than in DLP (Table 1). Rat VP is widely used as a model system for studying mechanisms of epithelial apoptosis. Epithelial apoptotic index in rat and mouse VP and DLP was also compared by counting positive cells for TUNEL staining. In both rat and mouse, epithelial apoptotic index was exceedingly low in intact animals, increased at 3 days after castration, and was significantly higher in VP than DLP following castration. In both VP and DLP, epithelial apoptotic index at 3 days after castration was significantly higher in rat than mouse (Table 1).
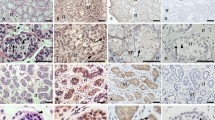
Prostatic tissue recombinants were prepared with rat urogenital sinus mesenchyme (rUGM) plus mouse bladder epithelium (mBLE) from wild-type (wt) or Tfm mice. The rUGM+mBLE tissue recombinants were grown under the kidney capsule of male athymic nude mice for 1 month (see Figure 6A for treatment protocol). After 1 month, both types of prostatic tissue recombinants developed normally and showed comparable prostatic histology as reported previously23 (Figure 2a,b). AR was detected in the wild-type rat stroma whether wt-mBLE or Tfm-mBLE was used to prepare the tissue recombinants (Figure 2a,b, arrows). AR was detected in the epithelium of rUGM+wt-mBLE tissue recombinants (Figure 2a) but not in the epithelium of rUGM+Tfm-mBLE tissue recombinants (Figure 2b). In intact hosts, epithelial apoptotic indices of both rUGM+wt-mBLE and rUGM+Tfm-mBLE prostatic tissue recombinants were equally low; there was no significant difference in epithelial apoptotic index in rUGM+wt-mBLE and rUGM+Tfm-mBLE tissue recombinants (Figure 4A,a). Three days after castration, many epithelial cells positive for TUNEL staining were detected in epithelium of both wt-mBLE and Tfm-mBLE prostatic tissue recombinants (Figure 3a,b). In castrated hosts the epithelial apoptotic indices of both rUGM+wt-mBLE and rUGM+Tfm-mBLE prostatic tissue recombinants (Figure 4A,b) increased significantly relative to tissue recombinants in intact hosts (Figure 4a). In castrated hosts, the difference in epithelial apoptotic index between rUGM+wt-mBLE and rUGM+Tfm-mBLE prostatic tissue recombinants was not significant. In addition to the androgen, orchiectomy could change levels of other hormones, such as estrogen. To confirm that the castration induced epithelial apoptosis in the prostatic tissue recombinants was due to a decrease in the androgen level, the host nude mice were given an androgen pellet (20 mg of T or DHT), and then castrated on 3 days after the pellet implantation. Both T and DHT blocked castration-induced epithelial apoptosis in both rUGM+wt-mBLE and rUGM+Tfm-mBLE prostatic tissue recombinants (Figure 3 and 4). Thus, differences in apoptotic indices were not statistically different in T-pellet/castration, DHT-pellet/castration and intact groups in both rUGM+wt-mBLE and rUGM+Tfm-mBLE tissue recombinants (Figure 4a). These results clearly showed that androgen maintains integrity of prostatic epithelial tissue via stromal AR. Epithelial AR is not involved in this process. Since DHT cannot be aromatized to estrogenic compounds, a role of estrogens in this process can be excluded.
Time lines for experiment protocol. (A) Protocol for induction of prostatic epithelial apoptosis. Prostatic tissue recombinants were grafted under the renal capsule of adult male athymic nude mice. After 1 month, some hosts were sacrificed to collect tissue recombinants at time zero as a control group, while others were castrated. Three days prior to the castration, 20 mg T or DHT pellets were subcutaneously implanted into some hosts. Three days after castration tissue samples were collected. (B) Protocol for progesterone treatment for female mice. Uterine tissue recombinants were grafted under the renal capsule of adult female athymic nude mice. All hosts were ovariectomized at approximately 1 month after grafting, and 2 weeks after the ovariectomy, all hosts were given 1 μg E2 daily for 3 days (days 1–3). After three injections of E2, hosts were treated with 2 mg/day of progesterone (P4) or oil for 3 days (days 4–6), and 24 h after the last hormone injection, tissue recombinants and host reproductive tracts were collected
Immunohistochemistry for AR and PR in uterine and prostatic tissue recombinants. ep, epithelium; st, stroma. AR-immunohistochemistry in prostatic tissue recombinants (a,b). Tissue recombinants were prepared with rat urogenital sinus mesenchyme (rUGM) and bladder epithelium (BLE) of wild-type (wt) or Tfm mice (m). In rUGM+wt-mBLE recombinants (a), AR-positive cells were detected in both epithelium and stroma (arrows). In contrast, AR-positive cells were detected only in stroma (arrows) of rUGM+Tfm-mBLE tissue recombinants (b). PR-immunohistochemistry in uterine tissue recombinants prepared with wild-type and PRKO tissues (c–f). Tissue recombinants were prepared with uterine epithelium (E) and stroma (S) from wild-type (wt) and PR knockout (ko) mice. In wt-S+wt-E tissue recombinants (c), positive nuclear staining for PR was detected in both epithelium and stroma. In contrast, both epithelium and stroma were negative for PR in ko-S+ko-E tissue recombinants (f). In wt-S+ko-E (d) and ko-S+wt-E (e) tissue recombinants, only wt-S or wt-E is positive for PR, respectively
Detection of apoptotic cells by in situ DNA fragmentation in prostatic and uterine tissue recombinants. rUGM+wt-mBLE (wt-E) (a,c) and rUGM+Tfm-mBLE (Tfm-E) (b,d) prostatic tissue recombinants in hosts 3 days post castration with (c,d) and without (a,b) 20 mg T-pellet (see Figure 6A for treatment protocol). Uterine tissue recombinants prepared with wild-type (wt) and PRKO (ko) tissues growing in P4-treated hosts. Wt-S+wt-E (e), wt-S+ko-E (f), ko-S+wt-E (g) and ko-S+ko-E (h). All hosts were received 2 mg of P4 injection daily following E2 treatment (see Figure 6B for treatment protocol)
Inhibition of apoptosis by P4 in PR null uterine luminal epithelial apoptosis
Uterine tissue recombinants (wt-S+wt-E, wt-S+PRKO-E, PRKO-S+wt-E and PRKO-S+PRKO-E) were grafted under the renal capsule of adult female athymic nude mice, and then all hosts received hormone treatments on the schedule shown in Figure 6B. To establish a baseline, we first examined uterine epithelial apoptosis in the host's uteri. Twenty-four hours after the last injection, many apoptotic cells were detected in uterine luminal epithelium of oil-treated hosts as judged by both apoptotic bodies observed in H&E stained slides (Figure 1e,f) and by TUNEL staining for in situ DNA fragmentation (Figure 1h). In contrast, very few apoptotic bodies and TUNEL stained epithelial cells were detected in uterine luminal epithelium of P4-treated hosts (Figure 1g). P4-treatment significantly reduced the apoptotic index in uterine luminal epithelium of host mice from 15.91±0.572% to 4.46±0.951% (P<0.001). Thus, for the uteri of host nude mice, P4 was anti-apoptotic as described previously.26
In all uterine tissue recombinants, the tissue types (PR-positive (wild-type) or PR-negative (PRKO)) were confirmed with PR-immunohistochemistry. Only tissues of wild-type mouse origin stained for PR. This is particularly evident in heterotypic tissue recombinants (wt-S+PRKO-E and PRKO-S+wt-E) (stroma in Figure 2d and epithelium in Figure 2e). In all four types of uterine tissue recombinants, apoptotic index of oil-treated (−P4) group was high (14–18%) and similar to that of the host's uterine epithelium (Figure 4B). P4-treatment inhibited uterine epithelial apoptosis only in tissue recombinants prepared with wt-S (wt-S+wt-E and wt-S+PRKO-E, Figure 3e,f, respectively). Thus, in wt-S+wt-E and wt-S+PRKO-E tissue recombinants, epithelial apoptotic index was significantly lower in the P4-treated group (+P4) than that of the oil-treated group (−P4) (Figure 4B,c). The presence or absence of PR in the epithelium did not affect its response to P4. In contrast, P4-treatment did not inhibit apoptosis in tissue recombinants lacking PR in the stroma (PRKO-S+wt-E and PRKO-S+PRKO-E, Figure 3g,h, respectively). Thus, in response to P4 epithelial apoptotic index in PRKO-S+wt-E and PRKO-S+PRKO-E tissue recombinants was significantly higher (Figure 4B,d) than that of wt-S+wt-E and wt-S+PRKO-E uterine tissue recombinants in the P4-treated host (Figure 4B,c).
Discussion
This study clearly demonstrated that steroid hormones regulate survival of epithelial cells via stromal steroid receptors in both prostatic and uterine tissue. Thus, androgen and progesterone regulate apoptosis in prostatic and uterine epithelia through paracrine mechanisms mediated by hormone receptors in the stroma. Paracrine regulation of epithelial cell death has been proposed in various models of development. For example, regression of embryonic mammary epithelial cells in male mice is induced by androgen through a paracrine mechanism mediated via AR in mammary mesenchyme.27 Likewise, apoptosis of Müllerian epithelium is induced by Müllerian inhibitory substance presumably via receptors in surrounding mesenchyme.28 In the case of mammary gland and Müllerian duct, the epithelial receptors for the hormones triggering epithelial apoptosis were not detected. In contrast, in prostate and uterus both the epithelium and stroma express receptors for the steroid hormones regulating epithelial apoptosis. Nevertheless, this study has clearly shown that epithelial steroid receptors are not involved in regulation of prostatic or uterine epithelial apoptosis induced by the withdrawal or the absence of androgen and progesterone, respectively. Hence, epithelial AR and PR are not required to directly regulate transcription of intracellular effectors for apoptosis in the mouse prostatic and uterine epithelial cells. This implies that some form of communication between the stroma and epithelium is required to elicit apoptosis in the epithelium.
There are two possible mechanisms by which stromal cells may control apoptosis of epithelial cells (Figure 5). In presence of steroid hormone, stroma may produce survival factors for epithelium (Figure 5A). Withdrawal of steroid hormones would down-regulate production of the survival factors and thus trigger apoptosis of epithelial cells (Figure 5A′). In some cells, cell death can be induced by withdrawal of peptide survival factors, such as epidermal growth factor (EGF).29 In prostate, androgens modify expression levels of members of EGF family ligand and receptors.30,31,32 In uterus, E2 and P4 regulate expression of peptide growth factors, such as members of EGF family,33,34 insulin-like growth factors (IGFs)35,36,37 and fibroblast growth factors (FGFs).38,39 Such peptide growth factors are good candidates for the survival factors for prostatic and uterine epithelium.
Models of paracrine mechanisms of uterine and prostatic epithelial apoptosis. (A) In presence of steroid hormones, steroid hormone binds to stromal steroid receptor, and the ligand occupied receptor activates signaling pathway to maintain epithelial cells. Even though epithelial steroid receptors are expressed, they are not involved in this signaling pathway. (A′) As the tissue steroid level is depleted, stromal production of the epithelial survival signal decreases, and epithelial cells undergo apoptosis (B) In response to a reduced steroid hormone level, stroma generates death signals which induce epithelial apoptosis
Alternatively, in response to decreased steroid levels stroma may produce death signals, which induce epithelial apoptosis (Figure 5B). In the prostate castration induces expression of several secreted molecules such as IGF binding proteins (IGFBPs).40 In the uterus, levels of IGFBPs are modulated by E2.41 IGF signaling plays a role in growth and survival of prostatic42 and uterine43 epithelia, and IGFBPs antagonize IGF signaling.44 Thus, IGFBPs are possible mediators of stromal-epithelial interactions in prostatic and uterine epithelial apoptosis. In prostate, castration increases mRNA levels of transforming growth factor (TGF)-βs.45 TGF-βs are known to be produced by prostatic stromal cells, and their receptors are expressed in prostatic epithelium.46,47 Transcripts for TGF-β-1,-2,-3 and their type-II receptors are upregulated in the mouse uterus after E2 withdrawal, and administration of P4 inhibits this up-regulation of mRNA for TGF-βs.48 TGF-βs are known to induce cell death in many different cell types including prostatic and uterine epithelia.49,50 Therefore, TGF-βs are also candidates as paracrine mediators of apoptotic (death) signaling. Epithelial apoptosis in uterus and prostate may be regulated by a balance of these two possible mechanisms (Figure 5A,B). A subtle change in the balance of survival/death signaling may determine the fate of epithelial cells.
Prostatic and uterine stromal tissue consists of many different cell types. The stromal cell types that are the direct target of androgen and progesterone in the regulation of epithelial apoptosis is not clear. Castration of mature male rats results in a rapid reduction of blood flow in VP coinciding with the appearance of TUNEL-positive vascular endothelial and stromal cells.51 This reduction in the blood flow precedes prostatic epithelial apoptosis in VP.51 P4 also regulates proliferation of the spiral arteries in endometrial stroma of primates.39 These studies suggest that action of androgen and P4 on the prostate and uterus, respectively, may involve blood vessel integrity and thus, regulation of blood flow. Vascular endothelial growth factor (VEGF) may be a mediator of androgen action on prostate blood flow. Exogenous androgen given to long-term castrated rats increases the level of vascular endothelial growth factor (VEGF) in VP.52
It has been tacitly assumed that activation of the molecular machinery of apoptosis elicited by androgen deprivation is due to failure to maintain ligand occupancy of the AR within the epithelial cells themselves. By this reasoning it is presumed that the occupancy status of the epithelial AR plays a key role in regulating the molecular machinery required for epithelial apoptosis. Our results demonstrate definitely that this is not the case. Epithelial AR is not required to elicit prostatic epithelial apoptosis triggered by androgen deprivation. One of the intracellular regulators of apoptosis is the bcl-2/bax ratio, which changes after castration in epithelium of rat ventral prostate.53 Castration of mature male rats also induces expression of transglutaminase54 and c-fos55 in the epithelium of rat ventral prostate. In the prostate these intracellular regulators and effectors for epithelial apoptosis must be regulated by androgen via stromal AR through a paracrine mechanism.
We observed that the epithelial apoptotic index of ventral and dorsolateral prostates in the rat is significantly higher than that of the mouse at 3 days after castration. The epithelium in rUGM+wt-mBLE prostatic tissue recombinants mostly shows a dorsolateral prostatic phenotype as assessed by expression of secretory protein specific for DLP.24 The prostatic tissue recombinants analyzed in this study were heterospecific (epithelium=mouse, mesenchyme=rat). Epithelial apoptotic index in rUGM+mBLE prostatic tissue recombinants was lower than that of rat DLP and higher than that of mouse DLP. Thus, the level of prostatic epithelial apoptosis may be determined by the origin and phenotype of both stromal and epithelial tissues, even though the kinetic pattern of apoptosis is similar in both species.
Our tissue recombination studies with steroid receptor null mutants have revealed the importance of paracrine mechanisms in steroid actions that regulate growth and differentiation in reproductive organs.56,57,58 This study emphasizes the importance of paracrine mechanisms in steroid hormone regulation of epithelial apoptosis in male and female reproductive tracts. In both male and female reproductive tracts (different systems) androgen and progesterone (different steroid hormones) elicit their anti-apoptotic effect via stromal receptors. These data, therefore, strongly suggest general mechanism, that for steroid target organs, hormones regulate epithelial apoptosis via paracrine mechanisms involving stromal-epithelial tissue interactions. Future studies on regulation of the machinery of apoptosis must take into account these paracrine mechanisms.
Materials and Methods
Animals
All animals were maintained in accordance with the NIH Guide for Care and Use of Laboratory Animals, and all procedures described here were approved by the UCSF. Mice were maintained under controlled temperature and lighting conditions during the experiment, and were given food and water ad libitum. Adult athymic nude mice, adult male and time-pregnant female Sprague-Dawley rats were purchased from Charles River (Wilmington, MA, USA). AR null male mice (Tfm male) were bred in our laboratory in a colony from breeding pairs (purchased from Jackson Laboratory).24 The affected Tfm males were identified by the presence of testis and female external genitalia. PRKO mice were produced by breeding heterozygous males and females, and genotypes of pups were determined by PCR as described before.59
Tissue separation, recombination and grafting
Details of prostatic24 and uterine18 tissue recombination have been described, previously. For prostatic tissue recombination, bladder epithelium from neonatal or adult wild-type and Tfm male mice was combined with urogenital sinus mesenchyme from gestation 18 day-old embryonic rats. For uterine tissue recombination, uteri from neonatal PRKO and wild-type litter-mate mice (days 3–10) were used. Female athymic mice were used as hosts for uterine tissue recombinants, and male athymic mice were used as hosts for prostatic tissue recombinant (Charles River, Wilmington, MA, USA).
Hormone treatment and castration
The experimental design to study prostatic epithelial apoptosis is illustrated in Figure 6A. Prostatic tissue recombinants were grown under the kidney capsule of male athymic nude mice for a month. After 1 month, some hosts were sacrificed to collect tissue recombinants at time zero as a control group, while others were castrated. Three days prior to the castration, 20 mg of T or DHT pellet were subcutaniously implanted into some of the hosts. Three days after castration tissue samples were collected. Pellets were made in our laboratory from T (Sigma) and DHT (Sigma) powder with a pellet press (Parr Instrument Co., Moline, IL, USA).
To study uterine epithelial apoptosis, a hormone treatment protocol described by Terada et al7 was utilized with modifications. The experimental design is illustrated in Figure 6B. Approximately 4 weeks after grafting, all hosts were ovariectomized and kept for another 2 weeks to allow establishment of a hormone deprived state. Two weeks after ovariectomy, daily dosages of 1 μg E2 (Sigma, St. Louis, MO, USA) was given to all hosts subcutaneously in 0.1 ml of vehicle for 3 days to stimulate uterine epithelial proliferation thus mimicking the E2 surge at the proestrus/estrus. E2 was dissolved in 0.9% NaCl, 0.4% Polysorbate 80 (Sigma), 0.5% carboxymethylecellose 80 (Sigma), and 0.9% benzyl alcohol 80 (Sigma) as described.6,7 From days 4 to 6, 2 mg progesterone (P4) (Steroids Inc., Wilton, NH, USA) in 0.1 ml peanut oil (Sigma), or 0.1 ml oil alone were given intraperitoneally. Twenty-four hours after the last hormone injection, host animals were sacrificed to harvest tissue samples.
Immunohistochemistry and apoptosis detection
Anti-human PR rabbit polyclonal antibody was purchased from DAKO (Carpenteria, CA). Anti-human AR was purchased from Affinity Bio Reagents (Golden, CO, USA). Tissues were fixed with 4% paraformaldehyde and processed into paraffin, and then sectioned at 6 μm. Slides were deparaffinized, re-hydrated and heated in 10 mM citrate buffer (pH 6.0) by microwave. Sections were incubated with primary antibody overnight. Immunoreactivity was developed by Vectorstain Elite ABC kit (Vector Laboratories Inc., Burlingame, CA, USA). ApoTag kit (Oncor Co., Gaithersburg, MD, USA) was used to detect 3′-hydroxyl termini of DNA in situ (TUNEL assay).
Apoptotic index
For prostate and prostatic tissue recombinants, since counting apoptotic bodies in H&E stained sections was technically difficult due to small number of apoptotic cells, positive and negative cells for TUNEL staining were counted to determine epithelial apoptotic index. For the apoptotic index of prostatic epithelium, propidiumiodide-counter stained epithelial cells were counted under a fluorescent microscope in randomly selected fields. Cells positive for TUNEL staining were counted in the same field. At least 10 fields from five to 33 prostate or tissue recombinants from at least 3 independent experiments were analyzed (minimum 2000 cells/group). For uterus and uterine tissue recombinants, epithelial apoptotic index was determined by counting apoptotic bodies on images of H&E slides captured with a DC330 camera (Dage-MTI Inc., Michigan City, IN, USA), interfaced with a PowerBase 200 computer (Power Computing, Round Rock, TX, USA). At least 2000 epithelial cells in 4–33 uterine tissue recombinants from 3 to 5 independent experiments were counted for each group, and in total 351 images from 24 nude mouse hosts and 85 tissue recombinants were analyzed. The result is analyzed by the factorial-ANOVA and Fisher's protected least significant difference (PLSD) tests.
Abbreviations
- AR:
-
androgen receptor
- DHT:
-
dihydrotestosterone
- E2:
-
17-β estradiol
- PR:
-
progesterone receptor
- PRKO:
-
progesterone receptor knockout
- P4:
-
progesterone
- T:
-
testosterone
- Tfm:
-
testicular feminization mutant
- wt:
-
wild-type
References
Kerr JF and Searle J . 1973 Deletion of cells by apoptosis during castration-induced involution of the rat prostate. Virchows Arch. B. Cell Pathol. 13: 87–102
Sandow BA, West NB, Norman RL and Brenner RM . 1979 Hormonal control of apoptosis in hamster uterine luminal epithelium. Am. J. Anat. 156: 15–35
Hopwood D and Levison DA . 1976 Atrophy and apoptosis in the cyclical human endometrium. J. Pathol. 119: 159–166
Isaacs JT, Furuya Y and Berges R . 1994 The role of androgen in the regulation of programmed cell death/apoptosis in normal and malignant prostatic tissue. Semin. Cancer Biol. 5: 391–400
Colombel M, Radvanyi F, Blanche M, Abbou C, Buttyan R, Donehower LA, Chopin D and Thiery JP . 1995 Androgen suppressed apoptosis is modified in p53 deficient mice. Oncogene 10: 1269–1274
Martin L, Finn CA and Carter J . 1970 Effects of progesterone and oestradiol-17 beta on the luminal epithelium of the mouse uterus. J. Reprod. Fertil. 21: 461–469
Terada N, Yamamoto R, Takada T, Miyake T, Terakawa N, Wakimoto H, Taniguchi H, Li W, Kitamura Y and Matsumoto K . 1989 Inhibitory effect of progesterone on cell death of mouse uterine epithelium. J. Steroid Biochem. 33: 1091–1096
Sato T, Fukazawa Y, Kojima H, Enari M, Iguchi T and Ohta Y . 1997 Apoptotic cell death during the estrous cycle in the rat uterus and vagina. Anat. Rec. 248: 76–83
Evans RM . 1988 The steroid and thyroid hormone receptor superfamily. Science 240: 889–895
Prins GS, Birch L and Greene GL . 1991 Androgen receptor localization in different cell types of the adult rat prostate. Endocrinology 129: 3187–3199
Tibbetts TA, Mendoza-Meneses M, O'Malley BW and Conneely OM . 1998 Mutual and intercompartmental regulation of estrogen receptor and progesterone receptor expression in the mouse uterus. Biol. Reprod. 59: 1143–1152
Uchima F-DA, Edery M, Iguchi T, Larson L and Bern HA . 1987 Growth of mouse vaginal epithelial cells in culture: Functional integrity of the estrogen receptor system and failure of estrogen to induce proliferation. Cancer Lett. 35: 227–235
McKeehan WL, Adams PS and Rosser MP . 1984 Direct mitogenic effects of insulin, epidermal growth factor, glucocorticoid, cholera toxin, unknown pituitary factors and possibly prolactin, but not androgen, on normal rat prostate epithelial cells in serum-free, primary cell culture. Cancer Res. 44: 1998–2010
Cooke PS, Uchima F-DA, Fujii DK, Bern HA and Cunha GR . 1986 Restoration of normal morphology and estrogen responsiveness in cultured vaginal and uterine epithelia transplanted with stroma. Proc. Natl. Acad. Sci. USA 83: 2109–2113
Sugimura Y, Cunha GR and Bigsby RM . 1986 Androgenic induction of deoxyribonucleic acid synthesis in prostatic glands induced in the urothelium of testicular feminized (Tfm/y) mice. Prostate 9: 217–225
Cooke P, Buchanan D, Young P, Setiawan T, Brody J, Korach K, Taylor J, Lubahn D and Cunha G . 1997 Stromal estrogen receptors (ER) mediate mitogenic effects of estradiol on uterine epithelium. Proc. Nat'l. Acad. Sci. USA 94: 6535–6540
Buchanan DL, Kurita T, Taylor JA, Lubahn DB, Cunha GR and Cooke PS . 1998 Role of stromal and epithelial estrogen receptors in vaginal epithelial proliferation, stratification, and cornification. Endocrinology 139: 4345–4352
Kurita T, Young P, Brody JR, Lydon JP, O'Malley BW and Cunha GR . 1998 Stromal progesterone receptors mediate the inhibitory effects of progesterone on estrogen-induced uterine epithelial cell deoxyribonucleic acid synthesis. Endocrinology 139: 4708–4713
Buchanan DL, Setiawan T, Lubahn DB, Taylor JA, Kurita T, Cunha GR and Cooke PS . 1999 Tissue compartment-specific estrogen receptor participation in the mouse uterine epithelial secretory response. Endocrinology 140: 484–491
Kurita T, Lee K, Cooke PS, Lydon JP and Cunha GR . 2000 Paracrine regulation of epithelial progesterone receptor and lactoferrin by progesterone in the mouse uterus. Biol. Reprod. 62: 831–838
Kurita T, Lee K, Cooke PS, Taylor JA, Lubahn DB and Cunha GR . 2000 Paracrine regulation of epithelial progesterone receptor by estradiol in the mouse female reproductive tract. Biol. Reprod. 62: 821–830
Cunha GR and Chung LWK . 1981 Stromal-epithelial interactions: I. Induction of prostatic phenotype in urothelium of testicular feminized (Tfm/y) mice. J. Steroid Biochem. 14: 1317–1321
Cunha GR, Reese BA and Sekkingstad M . 1980 Induction of nuclear androgen-binding sites in epithelium of the embryonic urinary bladder by mesenchyme of the urogenital sinus of embryonic mice. Endocrinology 107: 1767–1770
Donjacour AA and Cunha GR . 1993 Assessment of prostatic protein secretion in tissue recombinants made of urogenital sinus mesenchyme and urothelium from normal or androgen-insensitive mice. Endocrinology 131: 2342–2350
Bhatia-Gaur R, Donjacour AA, Sciavolino PJ, Kim M, Desai N, Young P, Norton CR, Gridley T, Cardiff RD, Cunha GR, Abate-Shen C and Shen MM . 1999 Roles for Nkx3.1 in prostate development and cancer. Genes Dev. 13: 966–977
Jo T, Terada N, Saji F and Tanizawa O . 1993 Inhibitory effects of estrogen, progesterone, androgen and glucocorticoid on death of neonatal mouse uterine epithelial cells induced to proliferate by estrogen. J. Steroid Biochem. Mol. Biol. 46: 25–32
Dürnberger H and Kratochwil K . 1980 Specificity of tissue interaction and origin of mesenchymal cells in the androgen response of the embryonic mammary gland. Cell 19: 465–471
Roberts LM, Hirokawa Y, Nachtigal MW and Ingraham HA . 1999 Paracrine-mediated apoptosis in reproductive tract development. Dev. Biol. 208: 110–122
Rawson CL, Loo DT, Duimstra JR, Hedstrom OR, Schmidt EE and Barnes DW . 1991 Death of serum-free mouse embryo cells caused by epidermal growth factor deprivation. J. Cell Biol. 113: 671–680
Taylor TB and Ramsdell JS . 1993 Transforming growth factor-alpha and its receptor are expressed in the epithelium of the rat prostate gland. Endocrinology 133: 1306–1311
Hiramatsu M, Kashimata M, Minami N, Sato A and Murayama M . 1988 Androgenic regulation of epidermal growth factor in the mouse ventral prostate. Biochem. Int. 17: 311–317
St-Arnaud R, Poyet P, Walker P and Labrie F . 1988 Androgens modulate epidermal growth factor receptor levels in the rat ventral prostate. Mol. Cell Endocrinol. 56: 21–27
Huet-Hudson YM, Chakraborty C, De SK, Suzuki Y, Andrews GK and Dey SK . 1990 Estrogen regulates the synthesis of epidermal growth factor in mouse uterine epithelial cells. Mol. Endocrinol. 4: 510–523
Zhang Z, Funk C, Glasser SR and Mulholland J . 1994 Progesterone regulation of heparin-binding epidermal growth factor-like growth factor gene expression during sensitization and decidualization in the rat uterus: effects of the antiprogestin, ZK 98.299. Endocrinology 135: 1256–1263
Ghahary A, Chakrabarti S and Murphy LJ . 1990 Localization of the sites of synthesis and action of insulin-like growth factor-I in the rat uterus. Mol Endocrinol. 4: 191–195
Westley BR and May FE . 1994 Role of insulin-like growth factors in steroid modulated proliferation. J. Steroid Biochem. Mol. Biol. 51: 1–9
Richards RG, DiAugustine RP, Petrusz P, Clark GC and Sebastian J . 1996 Estradiol stimulates tyrosine phosphorylation of the insulin-like growth factor-1 receptor and insulin receptor substrate-1 in the uterus. Proc. Natl. Acad. Sci. USA 93: 12002–12007
Rider V and Psychoyos A . 1994 Inhibition of progesterone receptor function results in loss of basic fibroblast growth factor expression and stromal cell proliferation during uterine remodelling in the pregnant rat. J. Endocrinol. 140: 239–249
Koji T, Chedid M, Rubin JS, Slayden OD, Csaky KG, Aaronson SA and Brenner RM . 1994 Progesterone-dependent expression of keratinocyte growth factor mRNA in stromal cells of the primate endometrium: keratinocyte growth factor as a progestomedin. J. Cell Biol. 125: 393–401
Nickerson T, Pollak M and Huynh H . 1998 Castration-induced apoptosis in the rat ventral prostate is associated with increased expression of genes encoding insulin-like growth factor binding proteins 2,3,4 and 5. Endocrinology 139: 807–810
Molnar P and Murphy LJ . 1994 Effects of oestrogen on rat uterine expression of insulin-like growth factor-binding proteins. J. Mol. Endocrinol. 13: 59–67
Cohen P, Peehl DM, Lamson G and Rosenfeld RG . 1991 Insulin-like growth factors (IGFs), IGF receptors, and IGF-binding proteins in primary cultures of prostate epithelial cells. J. Clin. Endocrinol. Metab. 73: 401–407
Shiraga M, Takahashi S, Miyake T, Takeuchi S and Fukamachi H . 1997 Insulin-like growth factor-I stimulates proliferation of mouse uterine epithelial cells in primary culture. Proc. Soc. Exp. Biol. Med. 215: 412–417
Lee PD, Giudice LC, Conover CA and Powell DR . 1997 Insulin-like growth factor binding protein-1: recent findings and new directions. Proc. Soc. Exp. Biol. Med. 216: 319–357
Kyprianou N and Isaacs JT . 1989 Expression of transforming growth factor-beta in the rat ventral prostate during castration-induced programmed cell death. Mol. Endocrinol. 3: 1515–1522
Kyprianou N and Isaacs JT . 1988 Identification of a cellular receptor for transforming growth factor-beta in rat ventral prostate and its negative regulation by androgens. Endocrinology 123: 2124–2131
Timme TL, Truong LD, Merz VW, Krebs T, Kadmon D, Flanders KC, Park SH and Thompson TC . 1994 Mesenchymal-epithelial interactions and transforming growth factor-beta expression during mouse prostate morphogenesis. Endocrinology 134: 1039–1045
Wada K, Nomura S, Morii E, Kitamura Y, Nishizawa Y, Miyake A and Terada N . 1996 Changes in levels of mRNAs of transforming growth factor (TGF)-beta1, -beta2, -beta3, TGF-beta type II receptor and sulfated glycoprotein-2 during apoptosis of mouse uterine epithelium. J. Steroid Biochem. Mol. Biol. 59: 367–375
Martikainen P, Kyprianou N and Isaacs JT . 1990 Effect of transforming growth factor-beta 1 on proliferation and death of rat prostatic cells. Endocrinology 127: 2963–2968
Rotello RJ, Lieberman RC, Purchio AF and Gerschenson LE . 1991 Coordinated regulation of apoptosis and cell proliferation by transforming growth factor beta 1 in cultured uterine epithelial cells. Proc. Natl. Acad. Sci. USA 88: 3412–3415
Shabsigh A, Chang DT, Heitjan DF, Kiss A, Olsson CA, Puchner PJ and Buttyan R . 1998 Rapid reduction in blood flow to the rat ventral prostate gland after castration: preliminary evidence that androgens influence prostate size by regulating blood flow to the prostate gland and prostatic endothelial cell survival. Prostate 36: 201–206
Joseph IB, Nelson JB, Denmeade SR and Isaacs JT . 1997 Androgens regulate vascular endothelial growth factor content in normal and malignant prostatic tissue. Clin. Cancer Res. 3: 2507–2511
Perlman H, Zhang X, Chen MW, Walsh K and Buttyan R . 1999 An elevated bax/bcl-2 ratio corresponds with the onset of prostate epithelial cell apoptosis. Cell Death Differ. 6: 48–54
Cummings M . 1996 Apoptosis of epithelial cells in vivo involves tissue transglutaminase upregulation. J. Pathol. 179: 288–293
Feng Z, Joos HJ, Vallan C, Muhlbauer R, Altermatt HJ and Jaggi R . 1998 Apoptosis during castration-induced regression of the prostate is Fos dependent. Oncogene 17: 2593–2600
Cunha GR, Hayward SW, Hom YK, Donjacour AA, Kurita T, Cooke PS and Lubahn DB . 1998 Growth factors as mediators of stromal-epithelial interactions in steroid hormone target organs. In Hormones and growth factors in development and neoplasia, Dickson RB and Salomon DS, eds. New York: Wiley-Liss, Inc. pp. 207–228
Cooke PS, Buchanan DL, Kurita T, Lubahn DB and Cunha GR . 1998 Stromal-epithelial cell communication in the female reproductive tract. In Contemporary Endocrinology, 9. Endocrinology of pregnancy, Bazer FW, eds Totowa, New Jersey, USA: Humana Press Inc. pp. 491–506
Cunha GR, Boutin EL, Turner T and Donjacour AA . 1992 Role of mesenchyme in the development of the urogenital tract. In Chemically-Induced Alterations in Sexual and Functional Development: The Wildlife/Human Connection, Colborn T and Clement C, eds. Princeton: Princeton Scientific Publishing Co., Inc. pp. 85–106
Lydon JP, DeMayo FJ, Funk CR, Mani SK, Hughes AR, Montgomery Jr CA, Shyamala G, Conneely OM and O'Malley BW . 1995 Mice lacking progesterone receptor exhibit pleiotropic reproductive abnormalities. Genes Dev. 9: 2266–2278
Acknowledgements
We thank Dr. Simon W Hayward (Department of Urology, University of California San Francisco, USA) for critical reading of the manuscript. This work was supported by NIH Grants AG-13784, AG-15500, AG-16870, CA 89520, DK 52645, DK 47517 and VA REAP.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by F D Miller
Rights and permissions
About this article
Cite this article
Kurita, T., Wang, Y., Donjacour, A. et al. Paracrine regulation of apoptosis by steroid hormones in the male and female reproductive system. Cell Death Differ 8, 192–200 (2001). https://doi.org/10.1038/sj.cdd.4400797
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4400797
Keywords
This article is cited by
-
Immunotherapy in endometrial cancer: rationale, practice and perspectives
Biomarker Research (2021)
-
Role of androgen receptor splice variant-7 (AR-V7) in prostate cancer resistance to 2nd-generation androgen receptor signaling inhibitors
Oncogene (2020)
-
Integrated transcriptomes throughout swine oestrous cycle reveal dynamic changes in reproductive tissues interacting networks
Scientific Reports (2018)
-
Influence of Cancer-Associated Endometrial Stromal Cells on Hormone-Driven Endometrial Tumor Growth
Hormones and Cancer (2015)
-
Desquamation is a novel phenomenon for collective prostate epithelial cell deletion after castration
Histochemistry and Cell Biology (2014)