Abstract
Little is known about genetic alterations of patients who present multiple primary cancers. We hypothesized that microsatellite instability (MSI) is one of the underlying genetic factors in the development of double primary cancers in colorectal cancer patients. We examined for MSI in 41 colorectal cancer patients who presented with extra-colonic primary cancers consisted of 17 gastric and 24 non-gastric cancers. Coincident MSI+ in tumors of two organs were observed in 3 (17.7%) of 17 patients with colon and stomach cancers and 0 of 24 patients with colon and non-gastric cancers (P =.03). In 17 patients with colon and stomach cancers, 6 (31.6%) of 19 colon cancers and 3 (17.7%) of 17 gastric cancers exhibited MSI+. Among four patients with metachronous colon cancers who were identified within the 41 double primary cancer patients, two patients were associated with the MSI+ phenotype. In summary, the prevalent coincidence of MSI suggests that genetic defect of mismatch repair deficiency may be responsible for a small subset of double primary cancers of the colorectum and stomach.
Similar content being viewed by others
INTRODUCTION
The incidence of multiple primary cancers is increasing significantly. Nearly 10% of cancer patients develop another primary cancer within 10 years of their first operation (1). Stomach cancer is the most prevalent extracolonic malignancy in multiple primary cancers with colon cancer in both Koreans (2) and Japanese (3). One of the tumors with significantly elevated risk is colon cancer after the diagnosis of stomach cancer (4).
The development of multiple primary cancers is known to be a feature of hereditary nonpolyposis colorectal cancer (HNPCC), and significantly increasing numbers of cancers of the stomach, small intestine, upper urologic tract (renal pelvis and ureter), and endometrium have been observed in HNPCC (5). Over 90% of the HNPCC tumors are MSI+ (6). However, the MSI+ phenotype has also been observed in approximately 10 to 15% of apparently sporadic colorectal cancers (7), and in about 10% of sporadic gastric cancers (8). Previously, significant associations have been noted between the MSI+ phenotype, and cancer multiplicity, cancers in other organs in the HNPCC patients (9, 10), and sporadic metachronous multiple colorectal carcinomas (11). Patients with multiple primary cancers are likely to be a part of a group with an underlying inherited predisposition.
Individuals who carry germline mutations in hMSH2 or hMLH1 probably have a higher risk of accumulating mutations in cancer-associated genes and of developing multiple primary cancers. There have been a few reports on the contribution of replication error in double cancers of the colorectum and stomach. Genetic instability may play an important role in the development of multiple primary cancers, and testing for MSI in a primary cancer may be an appropriate approach to the detection of patients at high risk for developing multiple primary cancers. Although it would be laborious to examine cancer patients for germline mutations in various mismatch repair genes, the presence or absence of MSI in tumors may constitute a useful marker for screening patients and identifying those at high risk for additional primary cancers. If the MSI+ tumor phenotype is an indicator of increased cancer susceptibility in these multiple primary cancer patients, then MSI detection may constitute a useful screening tool.
To investigate the above possibility, the MSI phenotype and frameshift mutation were analyzed in 17 patients with double primary cancers of the colorectum and stomach and 24 patients with double primary colorectal cancer and non-gastric malignancy. Additional studies for loss of heterozygosity (LOH) of the chromosomal arm 17p, and p53 immunohistochemical staining, were performed.
MATERIALS AND METHODS
Patients
Nineteen colon cancers and 17 gastric cancers from 17 patients with double primary cancers who underwent surgical resection between 1988 and 1997 at Seoul National University Hospital, Seoul, Korea, were analyzed. Double cancers of the colorectum and stomach were found synchronously in 5 patients and metachronously in 12 patients. The majority of the colon cancers were Dukes’ stage B or C (73.7% and 26.3%, respectively). The stomach cancers consisted of six early gastric cancers and 11 advanced gastric cancers. Nine were of the intestinal type and eight were of the diffuse type. The average age of 17 patients was 56.3 years, and the male to female ratio was 7.5:1.
As a control group, twenty-six colorectal cancers and 24 cancers of non-gastric origin from 24 patients of double primary cancers were analyzed for MSI. They were composed of malignant tumors from the prostate in four cases, the breast in three, the kidney in three, the urinary bladder in three, the uterine cervix in three, the liver in two, the skin in two, the small intestine in one, the endometrium in one, the hematopoietic system (multiple myeloma) in one, and sarcoma (malignant fibrous histiocytoma) in one. The average age of 24 patients was 58.6 years, and the male to female ratio was 1.7:1.
Among 41 patients with double cancers analyzed, 4 patients of metachronous colorectal cancers were identified. Two patients were of colon and stomach cancer pairs (cases 23 and 25), and remaining two were of colon and non-gastric origin cancer pairs (renal cell carcinoma and prostatic adenocarcinoma, respectively).
For comparison, 247 single primary colorectal cancers and 152 single primary gastric cancers were analyzed for MSI.
Information concerning cancer in first- and second-degree relatives has been obtained for all patients investigated in the present study. Patients with family history of the Amsterdam criteria for HNPCC were excluded. Family history of cancers in colorectum or stomach were identified in two (11.8%) of 17 patients with double primary cancers of the colorectum and stomach and 18 (7.3%) of 247 patients with single primary colorectal cancer.
DNA Extraction
DNA from 41 patients was obtained from formalin-fixed, paraffin embedded surgical sections. The microdissecion procedure was performed with 26 gauge needle under light microscopy. To reduce the possibility that the genetic abnormalities in the tumor cells would be compromised by the presence of normal cells, the neoplastic areas were microdissected from hematoxylin-eosin stained slides. This microdissection procedure harvests more than 60% of tumor cell populations (12).
Microsatellite Markers
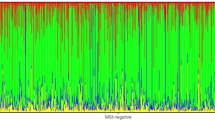
For the evaluation of MSI status in the 17 patients who had double cancers of the colorectum and stomach, five primers (BAT26, D5S346, D17S520, D17S786, and TP53) were purchased from Research Genetics (MapPair, Huntsville, AL). In the 24 patients with pairs of colorectal cancer and non-gastric malignancy, the MSI-H tumor was detected using the sensitive and specific marker, BAT26 (Fig. 1, left; 7, 12, 13, 14). The primers for the mononucleotide repeat microsatellite sequences were as follows: BAT26, located within Intron 5 of the hMSH2 gene; poly(A)10 tract of TGF-β RII; poly(G)8 tract of BAX; poly(G)8 tract of IGFIIR; and poly(A)8 tract of hMSH3. We used the same primers as described in a previously published paper (12).
Left, examples of BAT26 alteration. Carcinoma with size variation in the BAT26 allele is defined as MSI+. C1 and C2, metachronous colorectal cancers. Case 20 and Case 23 were MSI+ in two metachronous colon cancers and stomach cancer. Case 25 was MSI+ in one colon cancer but was MSI− in the other colon cancer and stomach cancer. Right, examples of microsatellite alteration. N, normal mucosa; C, colorectal cancer; S, stomach cancer. At marker D17S786, Case 22 exhibited prominent decrease of upper-band density in DNA of the colon cancer (Lane C) and stomach cancer (Lane S). Case 23 showed MSI in the stomach cancer (Lane S) and two colon cancers (Lanes C1 and C2).
PCR Amplification and Microsatellite Analysis
PCR amplification with MapPair primers was performed with 5 pmol/μL of each primer, 1.5 mm MgCl2, 0.2 mm deoxynecleotide triphosphate, 0.5 unit Taq polymerase, 0.1 μL [α- 32P] dCTP (3,000 Ci mmol-1, NEN, Dupoint, Boston, MA), and 1–2 μL of DNA in a total volume of 10 μl. The PCR conditions were 95°C for 5 minutes, followed by 33 cycles (94°C for 30 s, 45–58°C for 30 s, 72°C for 40 s), and a final elongation step at 72°C for 10 minutes. The PCR products were diluted to a concentration of 1:4 with a loading buffer, heated at 100°C for 5 minutes, and stored on ice until analysis. Then 1.5-μL aliquots of each sample were separated on denatured 6% polyacrylamide gel. The gel was dried on a vacuum slab gel dryer at 80°c for 1–1.5 hours, and exposed to X-ray film at −70°C for 12–72 hours.
MSI of any marker was defined as appearance of additional band in the PCR product in a tumor compared to normal counterpart. MSI+ denoted cases with MSI in two or more markers. MSI- included cases with no instability in any of the markers (MSS) and MSI in one marker (MSI-L; 7). LOH was scored when the band intensity of one allele was less than 50% in the tumor DNA than in normal DNA (Fig. 1, right).
To detect frameshift mutations in the coding regions, the reaction involved 32 cycles at 94°C for 1 minutes, at 53–60°C for 1 minutes, and at 72°C for 1 minutes using 3.7 × 104 Bq of 32P-dCTP in 10 μl of reaction mixture. The subsequent procedures were the same as for the MSI analysis.
p53 Immunostaining
Paraffin-embedded tissue sections of 4 μm thickness were stained using murine monoclonal antibody against p53 (Dakopatts, Copenhagen, Denmark, 1:100) by the avidin-biotin complex (ABC) method. Biotinylated rabbit anti-IgG and avidin-biotin-peroxidase conjugate were used for labeling and 3-diaminobenzidine was used for coloring. More than 10% of nuclear staining was considered to be positive.
Statistical Analysis
Either chi-test or Fisher’s exact test was used to analyze the differences in MSI status between the tumor groups. Statistical significance was defined as P <.05.
RESULTS
Six (31.6%) of 19 colon cancers and 3 (17.7%) of 17 gastric cancers were MSI+ in 17 patients with double cancers of the colorectum and stomach (Table 1). Three (17.7%) of 17 patients were MSI+ in both colon and gastric cancers. Twelve (70.6%) patients were MSI- in both the colorectal and gastric cancers. The remaining two (11.8%) patients were MSI+ in colon cancer, but MSI- in gastric cancer. We summarized the MSI results in Table 2.
Of 24 patients with double primary pairs of colorectal cancer and non-gastric malignancy, MSI+ was found in three (11.5%) of 26 colorectal cancers and one (4.2%) of 24 extra-colonic cancers (breast cancer). In the patient with MSI+ breast cancer, the colon cancer was MSI-. There were three patients with MSI+ both in colon and stomach pairs, compared to none in colon and non-gastric pairs (3 of 17 vs 0 of 24, P =.033, Fisher’s exact test).
Of 4 patients with metachronous colorectal cancers included in this study, one patient was MSI+ in both colon and stomach cancers (cases 23), one patient was MSI+ in colon cancer and MSI- in gastric cancer (case 25), and the remaining two patients with non-gastric cancer were MSI- in all of the detected cancers.
In our experimental study for MSI in single primary cancers, MSI+ rate was 9.7% in colorectal cancers, and 9.2% in stomach cancers. MSI+ rate in stomach cancers of the double cancer patients was not greater than expected one (3 of 17 vs 14 of 152, P =.27), however, it was significantly higher than expected in colorectal cancers (6 of 19 vs 24 of 247, P =.004; Table 2).
Five (83.3%) of 6 MSI+ colon cancers showed a frameshift mutation in the poly(A)10 tract of the TGF-β RII gene. All three MSI+ gastric cancers showed mutation in that gene. In contrast, mutations of hMSH3, IGFIIR or BAX in both cancers were found in less than half of the cases (Table 3).
The MSI+ colorectal cancers showed characteristics of localization in the proximal or right side of the colon, grossly ulcerofungating type, mucinous or poorly differentiation histologically, rare lymph node metastasis, and larger average tumor size (7.1 versus 4.8 cm). Three MSI+ stomach cancers showed exclusively intestinal type, no lymph node metastasis, and smaller average tumor size (2.5 versus 4.3 cm). In the colorectal cancers, 3 of 6 MSI+ cancers and one of thirteen MSI- cancers showed high numbers of intraepithelial lymphocytes (IELs; P =.036). However, no significant association between the degree of IELs and MSI status was found in the stomach cancers (1 of 3 vs 6 of 14, P =.76).
LOH at 17p was noted in 13 (81.3%) of 16 colorectal cancers and nine (64.3%) of 14 gastric cancers. In 10 (76.9%) of 13 MSI- colon cancers and 9 (64.3%) of 14 MSI- gastric cancers, 17p allelic loss was identified. Twelve (63.2%) of 19 colorectal cancers and 6 (35.3%) of 17 stomach cancers were positive in p53 immunostaining. Nine (69.2%) of 13 colorectal cancers and 6 (85.7%) of 7 gastric cancers with p53 overexpression were MSI-. The p53-positive cancers tended to be MSI-. 17p allelic loss was observed in 8 (66.7%) of 12 colorectal cancers and 4 (66.7%) of 6 gastric cancers with p53 overexpression. No correlation was demonstrated between p53 overexpression and 17p allelic loss.
DISCUSSION
In our study, 3 (17.7%) of 17 patients with double primary cancers of the colorectum and stomach showed the MSI+ in both cancers. It is suggested that there is a genetic component in the coincidence of double primary cancers of the colorectum and stomach, and that a defect in the mismatch repair system might be the causative mechanism in a small subset of double primary cancers.
Frequent MSI in multiple primary cancers of the colorectum or stomach have been reported (15, 16). In one series (15), MSI+ rate was reported in 17 (27.4%) of 62 cases of the multiple primary cancers excluding the HNPCC patients compared to 7 (8.1%) of 86 of the single primary colon cancers. These MSI+ rates are similar to our study. However, concordant MSI+ in double primary cancers was not analyzed in their study. In another series (16), 34 (89.5%) of 38 patients with multiple primary cancers were determined as MSI+, however, they had a limitation that MSI-L and MSI-H were not distinguished. To apply the recent consensus about MSI+ (7), they misclassified low frequency MSI (MSI-L) cases that were instable in one of 5 markers as MSI+. The 13 cases that were instable in one marker should be classified as MSI−.
Multiple cancers occurred in 5–10% (17, 18) of ordinary colorectal cancer patients, and in 11.5 (19)-24% (20) of HNPCC patients. In HNPCC, 10-year cumulative incidence of metachromous cancer is 40% if the first cancer is treated with less than a subtotal colectomy (5). Overall MSI+ rate in multiple colorectal cancers including HNPCC and sporadic tumors has been reported to be 28% (9).
In our study, most MSI+ tumors exhibited a TGF-β RII frameshift mutation and half of the MSI+ tumors showed BAX mutation. It is well known that the TGF-β RII gene is the main target of MSI+ sporadic colorectal cancer as well as of HNPCC (21, 22).
We demonstrated that the MSI+ tumors tended to show a lower rate of p53 overexpression as previously reported (10). The observed mismatch repair deficiency of double primary colorectal and gastric cancers suggests that there is an independent pathway involved in their carcinogenesis, which differs from the p53 pathway.
The MSI+ colorectal cancers in our study showed gross features of the fungating type, larger size, microscopically poorly differentiated or mucinous type histology, and rarely metastasized into the regional lymph nodes. It has been assumed that MSI+ colorectal cancers show similar histopathologic findings to HNPCC (23). All three cases of MSI+ gastric cancer in our study were of the intestinal type, and the size of the tumors was smaller than in MSI- stomach cancer. In addition, MSI+ stomach cancer seldom spread to the lymph nodes. The histological features of MSI+ colorectal cancer showed a large size and poor differentiation. In contrast, MSI+ stomach cancer showed a smaller size and good differentiation. The reason for the above discrepancy between these two different types of cancers should be investigated in future studies.
Considering the strong association of MSI+ with double primary colorectal-gastric cancers, we suggest that the carcinogenic background is related to genetic factors. The cancer susceptibility of non-HNPCC MSI+ colorectal-gastric primary cancer patients in this study is more likely to be the result of unrecognized genetic predisposition to mismatch repair defect.
References
Tsukuma H, Fujimoto I, Hanai A, Hiyama T, Kitagawa T, Kinoshita N . Incidence of second primary cancers in Osaka residents, Japan, with special reference to cumulative and relative risks. Jpn J Cancer Res 1994; 85: 339–345.
Kim HC, Kim CN, Jung CS, Yu CS, Kim JC . Multiple primary malignant neoplasm with colorectal cancer. J Korean Cancer Assoc 1998; 30: 668–674.
Akagi Y, Araki Y, Ogata Y, Morodomi T, Shirouzu K, Isomoto H, et al. Clinicopathological studies of multiple cancers in the large bowel and other organs. Kurume Med J 1993; 40: 81–88.
Hiyama T, Hanai A, Fujimoto I . Second primary cancer after diagnosis of stomach cancer in Osaka, Japan. Jpn J Cancer Res 1991; 82: 762–770.
Lynch HT, Smyrk T . Hereditary nonpolyposis colorectal cancer (Lynch syndrome). An updated review. Cancer 1996; 78: 1149–1167.
Liu B, Parsons R, Papadopoulos N, Nicolaides NC, Lynch HT, Watson P, et al. Analysis of mismatch repair genes in hereditary non-polyposis colorectal cancer patients. Nat Med 1996; 2: 169–174.
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 1998; 58: 5248–5257.
Kang GH, Yoon GS, Lee HK, Kwon YM, Ro JY . Clinicopathologic characteristics of replication error-positive gastric carcinoma. Mod Pathol 1999; 12: 15–20.
Pedroni M, Tamassia MG, Percesepe A, Roncucci L, Benatti P, Lanza G Jr, et al. Microsatellite instability in multiple colorectal tumors. Int J Cancer 1999; 81: 1–5.
Muta H, Noguchi M, Perucho M, Ushio K, Sugihara K, Ochiai A, et al. Clinical implications of microsatellite instability in colorectal cancers. Cancer 1996; 77: 265–270.
Masubuchi S, Konishi F, Togashi K, Okamoto T, Senba S, Shitoh K, et al. The significance of microsatellite instability in predicting the development of metachronous multiple colorectal carcinomas in patients with nonfamilial colorectal carcinoma. Cancer 1999; 85: 1917–1924.
Kim HS, Woo DK, Bae SI, Kim YI, Kim WH . Microsatellite instability in the adenoma-carcinoma sequence of the stomach. Lab Invest 2000; 80: 57–64.
Hoang J, Cottu PH, Thuille B, Salmon RJ, Thomas G, Hamelin R . BAT-26, an indicator of the replication error phenotype in colorectal cancers and cell lines. Cancer Res 1997; 57: 300–303.
Zhou XP, Hoang JM, Li YJ, Seruca R, Carneiro F, Sobrinho-Simoes M, et al. Determination of the replication error phenotype in human tumors without the requirement for matching normal DNA by analysis of mononucleotide repeat microsatellites. Genes Chromosom Cancer 1998; 21: 101–107.
Brown SR, Finan PJ, Hall NR, Bishop DT . Incidence of DNA replication errors in patients with multiple primary cancers. Dis Colon Rectum 1998; 41: 765–769.
Horii A, Han HJ, Shimada M, Yanagisawa A, Kato Y, Ohta H, et al. Frequent replication errors at microsatellite loci in tumors of patients with multiple primary cancers. Cancer Res 1994; 54: 3373–3375.
Enker WE, Dragacevic S . Multiple carcinomas of the large bowel: a natural experiment in etiology and pathogenesis. Ann Surg 1978; 187: 8–11.
Rennert G, Robinson E, Rennert HS, Neugut AI . Clinical characteristics of metachronous colorectal tumors. Int J Cancer 1995; 60: 743–747.
Fante R, Roncucci L, Di Gregorio C, Tamassia MG, Losi L, Benatti P, et al. Frequency and clinical features of multiple tumors of the large bowel in the general population and in patients with hereditary colorectal carcinoma. Cancer 1996; 77: 2013–2021.
Lynch HT, Watson P, Kriegler M, Lynch JF, Lanspa SJ, Marcus J, et al. Differential diagnosis of hereditary nonpolyposis colorectal cancer (Lynch syndrome I and Lynch syndrome II). Dis Colon Rectum 1988; 31: 372–377.
Akiyama Y, Iwanaga R, Ishikawa T, Sakamoto K, Nishi N, Nihei Z, et al. Mutations of the transforming growth factor-beta type II receptor gene are strongly related to sporadic proximal colon carcinomas with microsatellite instability. Cancer 1996; 78: 2478–2484.
Lu SL, Zhang WC, Akiyama Y, Nomizu T, Yuasa Y . Genomic structure of the transforming growth factor beta type II receptor gene and its mutations in hereditary nonpolyposis colorectal cancers. Cancer Res 1996; 56: 4595–4598.
Rodriguez-Bigas MA, Boland CR, Hamilton SR, Henson DE, Jass JR, Khan PM, et al. A National Cancer Institute Workshop on Hereditary Nonpolyposis Colorectal Cancer Syndrome: meeting highlights and Bethesda guidelines. J Natl Cancer Inst 1997; 89: 1758–1762.
Acknowledgements
This work was supported by Grant 03-2000-080 from the Seoul National University Hospital Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H., Cho, N., Yoo, J. et al. Microsatellite Instability in Double Primary Cancers of the Colorectum and Stomach. Mod Pathol 14, 543–548 (2001). https://doi.org/10.1038/modpathol.3880347
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880347
Keywords
This article is cited by
-
Multiple primary malignancies involving colorectal cancer—clinical characteristics and prognosis with reference to surveillance
Langenbeck's Archives of Surgery (2010)
-
Double primary malignancy in colorectal cancer patients—MSI is the useful marker for predicting double primary tumors
International Journal of Colorectal Disease (2009)
-
Geno- and pheno-typic characterization in ten patients with double-primary gastric and colorectal adenocarcinomas
International Journal of Colorectal Disease (2004)