Abstract
It is unclear whether synchronous multiple tumors arise from multicentric or monoclonal origins. To verify the multicentric origin of synchronous colorectal carcinomas at a genetic level, immunohistochemical and molecular techniques were used to determine the p53 alterations in individual lesions of synchronous colorectal carcinomas. This study was based on a total of 32 colorectal tumors from 16 patients. Twenty-one of the 32 (66%) advanced tumors examined had positive staining for p53. Single-strand conformation polymorphism and polymerase chain reaction direct sequencing were carried out for exons 5 to 8 of p53. All cases had p53 mutations in one or more tumors of synchronous lesions. In nine patients in this series, individual lesions were found to carry a different mutated codon of the p53 gene. In the other seven patients, a p53 mutation was found in one tumor but not in another. These results indicate discordance of the mutation pattern of p53 in individual lesions of multiple colorectal carcinomas and support the idea that most synchronous colorectal carcinomas are genetically distinguishable and are multicentric in origin. We also confirmed the high frequency of p53 mutations in left-sided (71%) and rectal (91%) carcinomas, rather than right-sided (43%; P =.04) carcinomas, suggesting that the molecular mechanism of synchronous colorectal carcinomas might differ between right- and left-sided tumors in the same patient.
Similar content being viewed by others
INTRODUCTION
The incidence of two or more primary colorectal carcinomas has been estimated to be 2 to 11% of all carcinomas in the colon and rectum. In 1957, Moertel and his colleagues (1) proposed histologic criteria for multiple colorectal carcinomas. However, it has been difficult to determine whether individual lesions in synchronous colorectal carcinomas arise from multicentric or monoclonal origins using conventional clinical and morphologic studies, because such lesions frequently show similar morphologic features both macroscopically and microscopically. Molecular biologic techniques have made it possible to evaluate multicentricity (i.e., to exclude metastases) at a genetic level. Greenblatt et al. (2) also reported that the analysis of substitution mutations can provide clues to the cause of these diverse lesions. Many investigators have attempted to determine the cause of multiple tumors in different organs using several molecular techniques. In the upper aerodigestive tract (3, 4), lung (5), stomach (6), and liver (7), multiple carcinomas have been alleged to be multicentric in origin. Conversely, investigators have claimed that multiple tumors in the bladder (8, 9), gynecologic organs (10, 11, 12), and breast (13) have the same clonal origin rather than multicentric. Moreover, some investigators have reported that multiple tumors in the urothelial organs and liver can have either a common or an independent origin (14, 15, 16).
The frequency of synchronous lesion generally is recognized to be much greater in patients who also have ulcerative colitis than in the general population (17). With regard to the synchronous colorectal carcinomas in patients without inflammatory bowel disease, some authors have reported the causative characteristics. On the basis of an analysis of p53 and K-ras mutations, Koness et al. (18) concluded that the great majority of synchronous colonic adenocarcinomas arose as independent neoplasms. In contrast, Schwartz et al. (19), on the basis of an analysis of nuclear DNA content, suggested that such lesions arose as transmural metastases from an initial single lesion.
Mutation of the p53 gene is the most common genetic alteration observed in many kinds of human neoplasms. As a molecular marker, p53 is considered to be helpful for differentiating between synchronous colorectal carcinomas of multicentric and monoclonal origin, because it is believed to be the most prevalent genetic alteration. The purpose of the current study was to classify the characteristics and to verify the possibility of a multicentric origin of synchronous colorectal carcinomas at a genetic level focusing on p53 alterations. We used immunohistochemical and molecular techniques to determine the mutation pattern of p53 in individual lesions of synchronous colorectal carcinomas.
MATERIALS AND METHODS
Samples
The clinicopathologic data are summarized in Table 1. Thirty-two colorectal carcinomas (formalin-fixed, paraffin-embedded tissues) were obtained from 16 patients who had undergone surgical resection and been diagnosed with synchronous colorectal carcinomas at the Department of Anatomic Pathology, Kyushu University, Pathological Sciences, Japan. Three patients (Patients 16, 17, and 20) had early-stage carcinomas in addition to advanced carcinomas, and these additional lesions were excluded from this study. All of the patients in this study initially were operated on at the Kyushu University Hospital or related hospitals. None of the cases received preoperative therapy, such as chemotherapy. The patients included 12 men and 4 women, ranging in age from 55 to 83 years (average, 66 years). Synchronous carcinomas met the criteria established by Moertel et al. (1). None of the patients had inflammatory bowel disease or familial polyposis syndrome. Our cases did not include the patients with hereditary nonpolyposis colorectal cancer, which is qualified by the minimum criteria in Amsterdam in 1990 (20), as far as we investigated. All of the specimens were embedded in paraffin after fixation in 10% formalin. Histologic sections taken for routine pathologic examination were evaluated and classified according to the World Health Organization classification (21), and staging was done according to the Turnbull modification of Dukes' classification (22). The larger tumor in each case was named T1. The data were statistically analyzed using Fisher's exact test.
P53 Immunohistochemistry
In all 32 tumor tissues from the 16 patients, immunohistochemical staining of p53 protein was performed. Four-micron-thick sections were cut, deparaffinized in xylene, and hydrated in descending dilutions of ethanol. After heating in phosphate-buffered saline (pH 7.2) for 10 min for antigen retrieval, endogenous peroxidase activity was blocked by 30 min of incubation with 0.3% hydrogen peroxide. All of the sections were incubated with the primary antibody PAb1801 (dilution 1/100; Oncogene Science, Cambridge, MA) overnight at 4° C. The subsequent development of antibody-bridge labeling was made by the streptavidin-biotin-peroxidase method (Histofine SAB-PO Kit; Nichirei, Tokyo, Japan) with hematoxylin counterstaining. Appropriate positive and negative controls were included. Immunoreactivity for p53 protein was evaluated by the distribution pattern of positive nuclei as follows: 0, negative tumors; 1+, low expression (1 to 10% immunoreactive tumor cells); 2+, moderate expression (10 to 50%); 3+, high expression (50 to 100%).
DNA Preparation
DNA was extracted from the paraffin-embedded tissue samples as described by Goelz et al. (23) with slight modifications. Briefly, sections (approximately 2 cm × 2 cm × 10 μm) dissected with a scalpel were deparaffinized with xylene, hydrated with ethanol, and digested in proteinase K solution (0.1 mg/mL proteinase K, 100 mm NaCl, 10 mm Tris-Cl, 25 mm EDTA, and 0.5% sodium dodecyl sulfate) for 48 to 72 h at 37° C. After phenol/chloroform extraction, DNA was precipitated with ethanol and redissolved in 0.1 × TE buffer (10 mm Tris, 1 mm EDTA). The concentration of the DNA solutions was determined by spectrophotometry and adjusted to 50 ng/μl. In all cases, DNA extracted from normal tissue of the same patients was used as a normal control.
Oligonucleotide Primers
Oligonucleotides for exons 5 and 6 of the p53 gene were obtained commercially (Clonetech, Palo Alto, CA). Their nucleotide sequences were as follows: PU5 (5′-CTCTTCCTGCAGTACTCCCCTGC-3′), PD5 (5′-GCCCAGCTGCTCACCATCGCTA-3′),PU6 (5′-GATTGCTCTTAGGTCTGGCCC-CTC-3′), PD6 (5′-GGCCACTGACAACCACCCTTAACC-3′);primers P71 (5′-GCTTGCCACAGGTCTCCCCAAG-3′) and P72 (5′-GTCAGGAGCCACTTGCCACCCTG-3′). P81 (5′-TGGTAATCTACTGGGACGGA-3′) and P82 (5′-GCTTAGTGCTCCCTGGGGGC-3′) werenoted to amplify exons 7 and 8.
Polymerase Chain Reaction Amplification
Genomic DNA was amplified by the polymerase chain reaction (PCR) in two steps (24). The first reaction mixtures (5 μl) contained 50 ng DNA, 1 pmol of each primer, 50 mm KCl, 10 mm Tris-HCl (pH 8.3), 2 mm MgCl2, dNTPs at 25 mm each, and 0.25 units of AmpliTaq DNA Polymerase (Perkin-Elmer, Branchburg, NJ). Forty cycles of the reaction at 95° C for 1 min, 66° C for 1 min, and 72° C for 2 min were performed in an automatic programmable thermal cycler (Gene Amp PCR System 9600; Perkin-Elmer Cetus, Norwalk, CT). The PCR products were electrophoresed on 2% agarose gel and stained with ethidium bromide. Bands that showed the proper length were cut, and the DNAs were eluted from the gel using a filter cartridge (SUPREC-01; Takara, Kyoto, Japan). The labeling reaction was then carried out using 1 μl of the eluted PCR products with 2 μCi α32-PdCTP for 10 cycles under the same conditions as described above. After Klenow treatment was performed, 40 μl of formamide dye (95% formamide, 20 mm EDTA, 0.05% bromophenol blue, and 0.05% xylene cyanol) was added to the reactions.
Single-Strand Conformation Polymorphism Analysis
Single-strand conformation polymorphism (SSCP) analysis was performed as previously described (25, 26). Electrophoresis was carried out under four different conditions as follows: Samples were denatured at 80° C for 5 min and loaded onto nondenaturing 5% polyacrylamide gel with or without 5% glycerol; electrophoresis was performed at 40W for 90 to 150 min at 15° C and 25° C, using a water-jacketed electrophoretic apparatus; gels were dried and exposed to X-ray films (XAR-5; Kodak, Rochester, NY) for 12 to 24 h at room temperature.
Direct DNA Sequencing
Abnormal bands detected by SSCP analysis were eluted from the gel and reamplified by PCR as described previously (26). The products were sequenced with 5′-and 3′-32P-labeled primers using a Thermo Sequenase cycle sequencing kit (Amersham, LIFE SCIENCE, Cleveland, OH). The primers used in the PCR-SSCP analysis served as sequencing primers. The conditions were according to the instructions of the manufacturer. Samples were loaded onto denaturing 6% urea gel and electrophoresed. Gels were then exposed to X-ray films (RX; Fuji, Kanagawa, Japan) and developed. When a mutation was found, PCR-SSCP analysis was repeated using the original DNA sample to exclude the possibility of PCR-induced DNA sequence changes. Moreover, when mutations at multiple sites on the p53 genome or the results of immunoreactivity and sequence analysis conflicted, new DNA samples were extracted from the sequential sections of the tumor paraffin block. PCR-SSCP analysis was then repeated to eliminate any possibility of identical mutations resulting from DNA contamination from other samples.
RESULTS
Clinicopathologic Findings
Of the 16 patients, 11 had lymph node metastases (Dukes' C) and 4 had no lymph node metastases (Dukes' B). No data were available regarding metastases in the remaining one patient. Twenty-seven of the 32 lesions (84%) were of low grade, including one mucinous carcinoma, and 4 were of high grade. Furthermore, 5 of the 32 lesions were associated with tubular adenomas (Table 1).
The lesions in two patients were histologically similar (Patients 7 and 17). In Patient 7, each tumor was of low histologic grade with abundant mucin, goblet cells, and less-pleomorphic nuclei forming irregular glands (Figs. 1 and 2). Each contained foci of tubular adenoma. In Patient 17, each tumor was of low grade and had well-differentiated glandular structures that had less-pleomorphic nuclei and that were located in the sigmoid colon. Two tumors were distinctly separated by 3.2-cm intervals of normal bowel wall. The lesions in eight patients (50%) were histologically dissimilar (Patients 14, 15, 19, 20, 21, 22, 23, and 25); in the remaining six patients (38%), the multiple lesions were histologically similar in part (Patients 3, 6, 9, 13, 16, and 24).
P53 Gene Alterations in Synchronous Colorectal Carcinomas
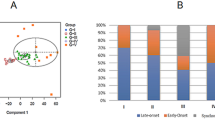
Table 2 shows the characteristics of p53 gene mutations, together with the relevant immunohistochemical data in each case. All cases had p53 mutations in one or more of the multiple tumors. In nine patients with p53 mutations in both tumors, individual lesions carried a different mutated codon of the p53 gene. In the other seven patients, a p53 mutation was found in one tumor but not in another. Hence, all of the cases examined showed heterogeneity in the location or the presence of p53 mutation (representative results of SSCP and the corresponding DNA sequence analysis are shown in Figs. 3 and 4). In Patient 7, who had histologically similar synchronous lesions (Fig. 2), T1 showed a transition mutation at codon 175 (CGC-CAC). T2 did not have any mutation in exons 5 to 8 (Fig. 3). In Patient 17, who had histologically and immunohistochemically similar synchronous lesions, SSCP analysis revealed that T1 and T2 carried an identical mutated exon (exon 7), whereas DNA sequencing showed different locations of the mutations (GGC-TGC at codon 245 in T1 and TCC-TTC at codon 241 in T2) (Fig. 4). Twenty-five of the 32 tumors had one or more p53 mutations. Twenty-four of the 28 mutations (86%) detected by sequencing resulted in missense errors, which led to a change in the amino acid sequence of p53 protein. Two nonsense mutations were due to the deletion of one base and resulted in frameshift mutations and the generation of a stop signal at codon 246. One intronic point mutation was also recognized. Mutations within introns may affect RNA splice sites and produce an abnormal p53 protein (27). Among the base substitutions, there was an extreme predominance of transitions. Twenty-one (88%) missense mutations were transitions, whereas only 3 of 24 (13%) were transversions. Fifteen of 21 transitions (71%) were guanine:cytosine to adenine:thymine changes, of which 6 occurred at cytosine phosphate guanine sites. Codon 175 in exon 6 and codon 248 in exon 7 are known as “hot spots” in p53 mutations in human cancers, and the same mutation, guanine:cytosine to adenine:thymine, was found in five tumors from five patients. To distinguish between genetic alterations in the germline and somatic mutations, we compared our results with those in non-neoplastic tissues. The same exon in which the mutation was found in the tumor was analyzed by PCR-SSCP and sequenced in the non-neoplastic tissue. Because no genetic alterations could be detected in non-neoplastic tissues, all of the mutations found in the tumors must have been of somatic origin. In a comparison of the relative intensity of the mutant and wild-type SSCP bands, five tumors appeared to have a loss of heterozygosity (Table 2). We could not evaluate loss of heterozygosity in other tumor samples because of significant contamination by normal cellular DNA.
Immunohistochemical Analysis: Correlation with P53 Mutation by SSCP
Twenty-one of the 32 tumors (66%) examined had positive staining for p53 (Table 2). Of the 21 carcinomas with positive staining, 19 (90%) showed mutations by SSCP. In contrast, of the 11 carcinomas with negative staining, 6 (55%) showed mutations by SSCP. The concordance between p53 nuclear reactivity and p53 mutations using SSCP was 75% (Table 3). Two tumors that were negative in p53 immunohistochemistry revealed a mobility shift in SSCP and contained a one base-pair deletion resulting in a stop codon (codon 246). In 7 of the 16 patients, the p53 immunohistochemistry in synchronous lesions was concordant (Table 2).
Correlation between P53 Alteration and Clinicopathologic Findings
P53 mutations were found more often in left-sided tumors, including rectal tumors, than in right-sided tumors, with a significant difference between right-sided tumors and rectal tumors (P =.04). The frequency of p53 nuclear reactivity in right-sided tumors was significantly lower than that in left-sided tumors, including rectal tumors (P <.05, Fisher's exact test). The frequency of p53 mutations in high-grade tumors was significantly lower than that in low-grade tumors (P <.05, Fisher's exact test) (Table 4).
DISCUSSION
Multiple tumors at many sites have been studied at a genetic level in many organs by several molecular techniques, including allelic deletions at chromosome-specific loci, viral integration analysis, flow cytometric analysis, and point mutation of specific genes, and the results have indicated that they were either monoclonal or multicentric.
With regard to the colon, however, the results regarding the cause of diverse lesions have not always been in agreement. Koness et al. (18) reported the discordance of p53 and K-ras mutations among individual lesions in the same patient, strongly suggesting that the great majority of synchronous colorectal carcinomas arise as independent neoplasms. In contrast, another study that used flow cytometric analysis noted that 3 of 10 patients with colorectal carcinomas had aneuploid tumors with identical DNA ploidy, suggesting that multiple primary carcinomas may, in some cases, be clonally related (19).
All of the cases examined in this study showed heterogeneity of the location or presence of p53 mutations. Two cases showed a markedly similar histology, along with a similar immunohistochemistry in one case, as well as a discrepancy in p53 mutation. The results of this investigation provide some support for the idea that most synchronous colorectal carcinomas are multicentric rather than monoclonal in origin. However, it is still possible that some of the synchronous colorectal carcinomas have a common origin, but tumor cells might migrate to other sites before the development of p53 mutations, resulting in primary and secondary sites displaying independent p53 mutations.
Delattre et al. (28) speculated that proximal and distal colon carcinomas might differ with regard to the genetic mechanism of their initiation and/or progression, because distal tumors show allelic losses more than twice as often as proximal tumors do. Moreover, Jernvall et al. (29) indicated that mutations in the conserved regions of the p53 gene accumulate in distal but not in proximal tumors. In our limited series of tumors, we confirmed the higher frequency of p53 mutations in left-sided (71%) and rectal (91%) carcinomas than in right-sided (43%) carcinomas (Table 4). Immunohistochemically, six of the seven right-sided tumors had negative staining for p53 protein. In addition, only one (Patient 3, T2) of the seven proximal tumors had a transition mutation in the nonconserved area. Moreover, in three of the five patients with both proximal and distal tumors, the proximal tumors had no mutations whereas the distal tumors had a mutation in the conserved regions of the gene. With regard to tumor location in synchronous colorectal carcinomas, the molecular mechanism of colorectal carcinogenesis may differ between right- and left-sided tumors, and the p53 genetic pathway of individual lesions may be fundamentally the same as that of sporadic colorectal carcinomas.
Point mutations of the p53 tumor suppressor gene have been reported in approximately 50% of colorectal carcinomas (30). Almost all of these mutations have been transitions, resulting in single base-pair changes (31). G:C to A:T transitions compose approximately 60 to 80% of colorectal tumor mutations, and most of them occur at cytosine phosphate guanine dinucleotides, as shown by previous studies (2, 30, 31, 32, 33). Moreover, most of these mutations are localized in four regions of the protein (residues 117–142, 171–181, 234–258, and 270–286), which are highly conserved among several different species (5). There are at least three mutation hot spots, affecting residues 175, 248, and 273 (34). In the current study, p53 mutations were scattered in exons 5 to 7 and were not clustered within hot spots. Only 6 of the 24 missense mutations showed a G:C to A:T transition at cytosine phosphate guanine dinucleotides (25%). These results regarding p53 mutation may reflect the limited number of samples examined in this study. Other reasons for these differences include the possibility of differences in environmental exposure or inherited characteristics among the populations, based on previous reports of different proportions of the p53 mutation spectrum (2, 35, 36, 37).
We also performed p53 immunohistochemical analysis on all of the tumors in this series. The two techniques gave concordant results in 75% of the tumors. Esrig et al. (38) and many other investigators have presented several possible reasons for the discrepancy between p53 gene mutations by SSCP and p53 expression by immunohistochemistry. In this study, two cases were immunohistochemically positive and SSCP negative (6% of the tumors). If the proportion of cells containing the mutation is low or if mutations occur outside the regions examined (exons 5 to 8), this could explain cases in which immunohistochemistry was positive but no mutation was detected (8, 38). Conversely, six cases were immunohistochemically negative and SSCP positive (19%). P53 mutations could be identified by DNA analysis, whereas no p53 is detected immunohistochemically if the mutation produces a stop signal or a large rearrangement or deletion that prevents expression of the protein. The mutation may also produce a protein with a very short half-life that cannot be detected immunohistochemically (27). Exon 5 resides closest to the denaturation-resistant epitope between amino acids 32 and 79 of the p53 protein. Therefore, mutations at exon 5 may alter the conformation of the p53 protein, making it more difficult to detect by immunohistochemistry using the monoclonal antibody PAb1801. Moreover, a p53 protein mutated at exon 6 may be degraded more rapidly, resulting in a low-intensity heterogeneous staining pattern (38).
In conclusion, these results show that synchronous colorectal carcinomas reveal a variety of mutations and have different patterns of genetic changes at separate sites. This suggests the independent development of synchronous colorectal carcinomas that are genetically distinguishable.
References
Moertel CG, Bargen JA, Dockerty MB . Multiple carcinomas of the large intestine: a review of the literature and a study of 261 cases. Gastroenterology 1958; 34: 85–98.
Greenblatt MS, Bennett WP, Hollstein M, Harris CC . Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Cancer Res 1994; 54: 4855–4878.
Chung KY, Mukhopadhyay T, Kim J, Casson A, Ro JY, Goepfert H, et al. Discordant p53 gene mutations in primary head and neck cancers and corresponding second primary cancers of the upper aerodigestive tract. Cancer Res 1993; 53: 1676–1683.
Yang HK, Linnoila RI, Conrad NK, Krasna MJ, Aisner SC, Johnson BE, et al. TP53 and RAS mutations in metachronous tumors from patients with cancer of the upper aerodigestive tract. Int J Cancer 1995; 64: 229–233.
Sozzi G, Miozzo M, Pastorino U, Pilotti S, Donghi R, Giarola M, et al. Genetic evidence for an independent origin of multiple preneoplastic and neoplastic lung lesions. Cancer Res 1995; 55: 135–140.
Kang GH, Kim CJ, Kim WH, Kang YK, Kim HO, Kim YI . Genetic evidence for the multicentric origin of synchronous multiple gastric carcinoma. Lab Invest 1997; 407–417.
Sakamoto M, Hirohashi S, Tsuda H, Shimosato Y, Makuuchi M, Hosoda Y . Multicentric independent development of hepatocellular carcinoma revealed by analysis of hepatitis B virus integration pattern. Am J Surg Pathol 1989; 13: 1064–1067.
Sidransky D, Frost P, Von EA, Oyasu R, Preisinger AC, Vogelstein B . Clonal origin bladder cancer. N Engl J Med 1992; 326: 737–740.
Lunec J, Challen C, Wright C, Mellon K, Neal DE . C-erbB-2 amplification and identical p53 mutations in concomitant transitional carcinomas of renal pelvis and urinary bladder. Lancet 1992; 339: 439–440.
Kupryjanczyk J, Thor AD, Beauchamp R, Poremba C, Scully RE, Yandell DW . Ovarian, peritoneal, and endometrial serous carcinoma: clonal origin of multifocal disease. Mod Pathol 1996; 9: 166–173.
Mok CH, Tsao SW, Knapp RC, Fishbaugh PM, Lau CC . Unifocal origin of advanced human epithelial ovarian cancers. Cancer Res 1992; 52: 5119–5122.
Smit VT, Fleuren GJ, van Houwelingen JC, Zegveld ST, Kuipers-Dijkshoorn NJ, Cornelisse CJ . Flow cytometric DNA-ploidy analysis of synchronously occurring multiple malignant tumors of the female genital tract. Cancer 1990; 66: 1843–1849.
Noguchi S, Aihara T, Koyama H, Motomura K, Inaji H, Imaoka S . Discrimination between multicentric and multifocal carcinomas of the breast through clonal analysis. Cancer 1994; 74: 872–877.
Goto K, Konomoto T, Hayashi K, Kinukawa N, Naito S, Kumazawa J, et al. P53 mutations in multiple urothelial carcinomas: a molecular analysis of the development of multiple carcinomas. Mod Pathol 1997; 10: 428–437.
Oda T, Tsuda H, Scarpa A, Sakamoto M, Hirohashi S . Mutation pattern of the p53 gene as a diagnostic marker for multiple hepatocellular carcinoma. Cancer Res 1992; 52: 3674–3678.
Tsuda H, Oda T, Sakamoto M, Hirohashi S . Different pattern of chromosomal allele loss in multiple hepatocellular carcinomas as evidence of their multifocal origin. Cancer Res 1992; 52: 1504–1509.
Greenstein AJ, Slater G, Heimann TM, Sachar DB, Aufses AH Jr . A comparison of multiple synchronous colorectal cancer in ulcerative colitis, familial polyposis coli, and de novo cancer. Ann Surg 1986; 203: 123–128.
Koness RJ, King TC, Schechter S, McLean SF, Lodowsky C, Wanebo HJ . Synchronous colon carcinomas: molecular-genetic evidence for multicentricity. Ann Surg Oncol 1996; 3: 136–143.
Schwartz D, Banner BF, Roseman DL, Coon JS . Origin of multiple “primary” colon carcinomas: a retrospective flow cytometric study. Cancer 1986; 58: 2082–2088.
Vasen HFA, Mecklin J-P, Khan PM, Lynch HT . The international collaborative group on hereditary non-polyposis colorectal cancer (ICG-HNPCC). Dis Colon Rectum 1991; 34: 424–425.
Large intestine. In: Jass JR, Sobin LH, editors. Histological typing of intestinal tumours. 2nd ed. Berlin: Springer-Verlag; 1989. pp. 29–40.
Turnbull RJ, Kyle K, Watson FR, Spratt J . Cancer of the colon: the influence of the no-touch isolation technic on survival rates. Ann Surg 1967; 166: 420–427.
Goelz SE, Hamilton SR, Vogelstein B . Purification of DNA from formaldehyde fixed and paraffin embedded human tissue. Biochem Biophys Res Commun 1985; 130: 118–126.
Hayashi K, Kukita Y, Inazuka M, Tahira T . Single-strand conformation polymorphism analysis. In: Cotton RGH, Edkins E, Forrest S, editors. Mutation detection. Oxford: Oxford University Press; 1997. pp. 7–17.
Orita M, Suzuki Y, Sekiya T, Hayashi K . Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics 1989; 5: 874–879.
Suzuki Y, Sekiya T, Hayashi K . Allele-specific polymerase chain reaction: a method for amplification and sequence determination of a single component among a mixture of sequence variants. Anal Biochem 1991; 192: 82–84.
Dunn JM, Hastrich DJ, Newcomb P, Webb JC, Maitland NJ, Farndon JR . Correlation between p53 mutations and antibody staining in breast carcinoma. Br J Surg 1993; 80: 1410–1412.
Delattre O, Olschwang S, Law DJ, Melot T, Remvikos Y, Salmon RJ, et al. Multiple genetic alterations in distal and proximal colorectal cancer. Lancet 1989; 2: 353–356.
Jernvall P, Makinen M, Karttunen T, Makela J, Vihko P . Conserved region mutations of the p53 gene are concentrated in distal colorectal cancers. Int J Cancer 1997; 74: 97–101.
Hollstein M, Sidransky D, Vogelstein B, Harris CC . P53 mutations in human cancers. Science 1991; 253: 49–53.
Baker SJ, Preisinger AC, Jessup JM, Paraskeva C, Markowitz S, Willson JK, et al. P53 gene mutations occur in combination with 17p allelic deletions as late events in colorectal tumorigenesis. Cancer Res 1990; 50: 7717–7722.
Nigro JM, Baker SJ, Preisinger AC, Jessup JM, Hostetter R, Cleary K, et al. Mutations in the p53 gene occur in diverse human tumour types. Nature 1989; 342: 705–708.
Cunningham J, Lust JA, Schaid DJ, Bren GD, Carpenter HA, Rizza E, et al. Expression of p53 and 17p allelic loss in colorectal carcinoma. Cancer Res 1992; 52: 1974–1980.
Levine AJ, Momand J, Finlay CA . The p53 tumour suppressor gene. Nature 1991; 351: 453–456.
Kikuchi YR, Konishi M, Ito S, Seki M, Tanaka K, Maeda Y, et al. Genetic changes of both p53 alleles associated with the conversion from colorectal adenoma to early carcinoma in familial adenomatous polyposis and non-familial adenomatous polyposis patients. Cancer Res 1992; 52: 3965–3971.
Lothe RA, Fossli T, Danielsen HE, Stenwig AE, Nesland JM, Gallie B, et al. Molecular genetic studies of tumor suppressor gene regions on chromosomes 13 and 17 in colorectal tumors. J Natl Cancer Inst 1992; 84: 1100–1108.
Wu AH, Paganini HA, Ross RK, Henderson BE . Alcohol, physical activity and other risk factors for colorectal cancer: a prospective study. Br J Cancer 1987; 55: 687–694.
Esrig D, Spruck CH III, Nichols PW, Chaiwun B, Steven K, Groshen S, et al. P53 nuclear protein accumulation correlates with mutations in the p53 gene, tumor grade, and stage in bladder cancer. Am J Pathol 1993; 143: 1389–1397.
Acknowledgements
The surgical specimens and clinical data reported here were obtained from the following institutes: Kyushu University Hospital, Wakamatsu Public Hospital, Kimura Hospital, Kuroki Hospital, and Nougata Central Hospital. We thank Tomoko Tahira, Akari Suzuki, Yoji Kukita (Division of Genome Analysis, Institute of Genetic Information, Kyushu University), Yoichi Hachitanda (Division of Pathology, Clinical Laboratory, Kitakyushu Municipal Medical Center), and Takashi Utsunomiya (National Kyushu Medical Center) for their laboratory help and advice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eguchi, K., Yao, T., Konomoto, T. et al. Discordance of P53 Mutations of Synchronous Colorectal Carcinomas. Mod Pathol 13, 131–139 (2000). https://doi.org/10.1038/modpathol.3880024
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880024
Keywords
This article is cited by
-
Germline and somatic genetic predictors of pathological response in neoadjuvant settings of rectal and esophageal cancers: systematic review and meta-analysis
The Pharmacogenomics Journal (2016)
-
Patients with genetically heterogeneous synchronous colorectal cancer carry rare damaging germline mutations in immune-related genes
Nature Communications (2016)
-
Synchronous collision malignant melanoma and adenocarcinoma of the rectum
Techniques in Coloproctology (2010)
-
Epigenetic profiling of synchronous colorectal neoplasias by quantitative DNA methylation analysis
Modern Pathology (2006)
-
Complete single-stage management of left colon cancer obstruction with a new device
Surgical Endoscopy (2005)