Abstract
Inflammatory myofibroblastic tumors are uncommon lesions composed of spindled myofibroblasts within a variable background of collagen and inflammatory cells. Although the true nature of these lesions is not fully elucidated, identification of consistent cytogenetic alterations in the anaplastic lymphoma kinase (ALK) gene suggests that they may be neoplastic. A small number of inflammatory myofibroblastic tumors have been reported to harbor human herpesvirus-8 (HHV-8), implicating the virus in its pathogenesis. In this study, 20 cases of pulmonary inflammatory myofibroblastic tumor were analyzed for the presence of HHV-8 with immunohistochemical and molecular methods. In all cases, antibodies to the latent nuclear antigen of the virus were applied. Four open reading frames (ORFs), including ORFs K2, 16, 26, and 72, were targeted utilizing real-time polymerase chain reaction (PCR). The cohort included 9 men and 11 women with a mean age of 37 years (range, 1–81). Microscopically, the tumors were composed of cytologically bland spindle cells with myofibroblastic differentiation. On immunohistochemical studies, 20% of cases (4/20) demonstrated diffuse cytoplasmic positivity with ALK. Immunohistochemical staining for the latent nuclear protein of the virus was negative in all cases (0/20). All tumors (100%, 20/20) tested with real-time PCR were negative for all four ORFs, whereas 100% (10/10) of positive control Kaposi sarcoma cases were positive. Her2 gene expression was present in all (20/20) inflammatory myofibroblastic tumors confirming the presence of amplifiable deoxyribonucleic acid in the tissue lysate. This study documents the absence of HHV-8 in pulmonary inflammatory myofibroblastic tumors, suggesting that further investigation is required to clarify the pathogenesis of this lesion.
Similar content being viewed by others
Main
Inflammatory myofibroblastic tumor of the lung occurs in all age groups without gender bias but, most commonly, in individuals under 40 years of age.1, 2 Microscopically, inflammatory myofibroblastic tumor is composed of a proliferation of spindled myofibroblasts within a variable background of collagen and inflammatory cells. Although the pathogenesis of these lesions is not fully elucidated, recent studies suggest they may be neoplastic proliferations with potential to invade the mediastinum, hilar lymph nodes, and diaphragm.3 The neoplasia concept is supported by the presence of cytogenetic alterations in the anaplastic lymphoma kinase (ALK) gene, including TPM3–ALK, TPM4–ALK, and CLTC–ALK fusions, and ALK protein expression.4, 5 Clonal aberrations in the 2p23 and ALK gene regions have been demonstrated in both pulmonary and extrapulmonary inflammatory myofibroblastic tumors.3, 6
Viral infections, in particular human herpesvirus-8 (HHV-8), have been implicated in inflammatory myofibroblastic tumor pathogenesis. HHV-8 infects a wide range of normal cells including endothelial cells, lymphoid cells, dendritic cells, and fibroblasts. This parallels the spectrum of the neoplasms with a well-established role for HHV-8 in their pathogenesis, including Kaposi sarcoma, primary effusion lymphoma, and multicentric Castleman disease. HHV-8 infection of human fibroblasts is well documented in experimental studies. It is known that the virus enters cells utilizing receptor-mediated endocytosis7 and displays activation of lytic and persistence of latent genes.7, 8 In light of these findings, inflammatory myofibroblast tumor appears to be a reasonable choice for HHV-8 testing. Gómez-Román et al,9 reported HHV-8 deoxyribonucleic acid (DNA) sequences in seven cases of inflammatory myofibroblast tumor, and also identified viral transcripts from several open reading frames (ORF).10 In the English language literature, only three additional cases of pulmonary inflammatory myofibroblastic tumor have been studied for HHV-8 by immunohistochemical and molecular methods.11 Thus, in the largest study to date, we investigated the presence of HHV-8 in pulmonary inflammatory myofibroblast tumor.
Materials and methods
Case Selection
Seventy-five cases diagnosed as inflammatory pseudotumor or inflammatory myofibroblastic tumor between 1988 and 2004 were retrieved from the registry of the Department of Pulmonary and Mediastinal Pathology, Armed Forces Institute of Pathology. The cases were re-reviewed to exclude inflammatory/reactive and frankly sarcomatoid lesions. Availability of tissue blocks and/or unstained slides served as another exclusion criterion. Following such selection, 20 cases comprised the current study. Clinical and demographic findings were compiled from the charts.
Immunohistochemistry
Tissue blocks were routinely processed and serial sections of 3 μm thick and mounted on positive-charged microscope slides, incubated in a heat bath, deparaffinized, and rehydrated. Citrate buffer (pH 6.0, at 100°C for 30 min) was used for antigen retrieval. Antibodies were used according to the manufacture's instructions. Slides were counterstained with hematoxylin and covered by nonaqueous medium. Antibodies against HHV-8 latent nuclear antigen (clone 13B10, 1:40, Vector Laboratories, Burlingame, CA, USA) and ALK (clone ALK-1, 1:100, Dako, Carpinteria, CA, USA) were applied in all 20 cases.
Real-Time Polymerase Chain Reaction
Two 7 μm unstained slides from formalin-fixed, paraffin-embedded tissue for each case were deparaffinized and DNA was obtained through proteinase K digestion, phenol/chloroform/isoamyl alcohol extraction, and ethanol precipitation. DNA was stored at −20°C before use. Primers and probes for real-time polymerase chain reaction (PCR) were designed based on the published sequence in the GenBank database (U75698) available via the National Center for Biotechnology Information. Four sets of primers and probes, as shown in Table 1, aimed to detect four ORFs of HHV-8, were synthesized by Integrated DNA Technologies Inc. The real-time PCR was performed in an ABI 7500 Real-Time PCR System. PCR cycles were 2 min at 50°C, followed by 10 min at 95°C and 40 cycles of 15 s at 95°C and 1 min at 60°C. Her2 gene was used to test for the presence of amplifiable DNA in the tissue lysate. BC-1, a lymphoma cell line containing HHV-8 genome from ATCC (ATCC no. CRL-2230), and 10 cases of Kaposi sarcoma were used as positive controls.
Results
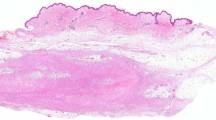
The cohort included 9 men and 11 women with a mean age of 37.3 years (range, 1–81) (Table 2). Eighty percent (16/20) of cases presented as well-circumscribed parenchymal masses, 15% (3/20) were central involving bronchi, and one case (5%) presented as a 7.5 cm mass involving the chest wall. The average tumor size was 3.8 cm (range, 1.5–7.5). Grossly, tumors were firm, white to gray masses without necrosis. Histologically, tumors were comprised of spindle cells with fibroblastic and myofibroblastic differentiation arranged in fascicles and/or storiform pattern (Figure 1a). The spindle cells had abundant, bipolar, pale eosinophilic cytoplasm, and contained oval nuclei with fine nuclear chromatin and inconspicuous nucleoli. Variable inflammatory infiltrates of plasma cells, lymphocytes, foamy macrophages, and histiocytes were admixed. Cytologic atypia was minimal and mitoses rare. On immunohistochemical studies, 20% (4/20) of cases showed diffuse cytoplasmic staining with ALK (Figure 1b) and all cases were negative (20/20) with HHV-8. All tumors (20/20) were negative for the four ORFs of HHV-8 in real-time PCR, whereas 100% (10/10) of Kaposi sarcomas, serving as positive control, were positive. Her2 gene expression in all of the inflammatory myofibroblastic tumors confirmed the presence of amplifiable DNA in the tissue lysate.
Discussion
There is a strong association between HHV-8 and Kaposi sarcoma, multicentric Castleman disease, and primary effusion lymphoma. HHV-8 has also been reported to be present in pemphigus vulgaris, extranodal marginal zone lymphoma of salivary gland, hemophagocytic syndrome, multiple myeloma, Kikuchi lymphadenitis, and sarcoidosis.12, 13, 14, 15, 16, 17 However, the latter list of diseases is controversial as viral detection varies among studies.18, 19, 20, 21 Two publications by Gómez-Román et al,9, 10 documenting HHV-8 in lesional myofibroblasts of inflammatory myofibroblastic tumor, drew attention to the possible role of the virus in the pathogenesis of this tumor. In the largest series to date, twenty cases of pulmonary inflammatory myofibroblastic tumor were studied for the presence of HHV-8. Whereas the demographic, clinical, and histological features in all cases were typical for inflammatory myofibroblastic tumor, no viral DNA or latent nuclear antigen was identified utilizing immunohistochemical or molecular studies.
The observations reported by Gómez-Román et al,10 were based on five cases of ALK-negative pulmonary inflammatory myofibroblastic tumor and raised the question of whether the presence of virus is restricted to the lesions lacking ALK expression and/or to lesions of the lung (Table 3). In a subsequent report, Yamamoto et al22 addressed this issue utilizing 21 ALK-positive and ALK-negative tumors from multiple sites including lung. All 21 cases were negative for HHV-8, leading the authors to suggest the virus does not play a role in the pathogenesis of inflammatory myofibroblastic tumor. However, the Yamamoto et al study22 had a limited number of pulmonary inflammatory myofibroblastic tumors, only three cases, and targeted only one ORF (ORF26). Similar to the study by Gómez-Román et al,10 we focused on pulmonary lesions and expanded the number of cases to 20, including 4 ALK-positive tumors; all 20 were negative for HHV-8. As we found no viral DNA, it was not surprising that all our cases were negative for latent nuclear antigen, corroborating the immunohistochemical findings on inflammatory myofibroblastic tumor from varying sites reported by Yamamoto et al22 and pediatric cases reported by Mergan et al.23
Molecular identification of HHV-8 is known to produce both false-positive and false-negative results.24, 25, 26 The latter is thought, in part, to be related to HHV-8 sequence variation, which can range up to 35% in certain regions of the viral genome, as in ORFK1.26 The use of a single primer set based on a sequence with a high level of sequence variation can lower the PCR sensitivity and, therefore, the rate of HHV-8 detection. Another potential source of false-negative results is targeting large fragments of viral DNA. Based on our experience and data in the literature, 250 base pairs are often beyond the upper size limit of what can readily be amplified by PCR from formalin-fixed, paraffin-embedded tissue.24 False-positive results are thought to be due to utilization of high cycle protocols and/or complimentary primer sets, as in nested PCR. Through a set of validation tests, Pan et al,25 demonstrated that nested PCR is readily contaminated, even in strictly controlled environments, and use of standard PCR with more than one set of primers is recommended. In their study, 6 of 16 negative controls tested positive for HHV-8 sequences in nested PCR using primers to ORF26, but none were positive utilizing standard PCR. The contamination by nucleic acids, particularly from previously amplified material (carry-over), is likely the main source of false-positive results.
To achieve reliable results, we employed a detection system addressing the issues surrounding the occurrence of false-positive and -negative results described in the literature. First, our detection system used four ORFs of the viral genome (Table 4), including two primer pairs that enabled detection of HHV-8 in the Gómez-Román et al study,10 namely ORFK2 (viral interleukin-6 homolog) and ORF72 (cyclin D homolog), a primer pair used in the Ding et al27 study ORF26 (minor capsid protein), and another employed in several Kaposi sarcoma studies, that is, ORF16 (viral Bcl-2 homolog). Second, to increase efficiency of PCR amplification, the targeted sequences did not exceed 234 base pairs. Third, to overcome the problem of carry-over contamination, a closed-tube detection system, real-time PCR, was used. Nevertheless, application of this more stringent and sensitive detection system revealed no evidence of the viral genome in a large set of cases. These data suggest that: (1) HHV-8 plays no role in pathogenesis of pulmonary inflammatory myofibroblastic tumor and (2) further investigation is needed to elucidate other potential causative factors for this lesion.
References
Gal AA, Koss MN, McCarthy WF, et al. Prognostic factors in pulmonary fibrohistiocytic lesions. Cancer 1994;73:1817–1824.
Souid AK, Ziemba MC, Dubansky AS, et al. Inflammatory myofibroblastic tumor in children. Cancer 1993;72:2042–2048.
Yousem SA, Shaw H, Cieply K . Involvement of 2p23 in pulmonary inflammatory pseudotumors. Hum Pathol 2001;32:428–433.
Griffin CA, Hawkins AL, Dvorak C, et al. Recurrent involvement of 2p23 in inflammatory myofibroblastic tumors. Cancer Res 1999;59:2776–2780.
Lawrence B, Perez-Atayde A, Hibbard MK, et al. TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic tumors. Am J Pathol 2000;157:377–384.
Coffin CM, Patel A, Perkins S, et al. ALK1 and p80 expression and chromosomal rearrangements involving 2p23 in inflammatory myofibroblastic tumor. Mod Pathol 2001;14:569–576.
Akula SM, Naranatt PP, Walia NS, et al. Kaposi's sarcoma-associated herpesvirus (human herpesvirus 8) infection of human fibroblast cells occurs through endocytosis. J Virol 2003;77:7978–7990.
Krishnan HH, Naranatt PP, Smith MS, et al. Concurrent expression of latent and a limited number of lytic genes with immune modulation and antiapoptotic function by Kaposi's sarcoma-associated herpesvirus early during infection of primary endothelial and fibroblast cells and subsequent decline of lytic gene expression. J Virol 2004;78:3601–3620.
Gomez-Roman JJ, Ocejo-Vinyals G, Sanchez-Velasco P, et al. Presence of human herpesvirus-8 DNA sequences and overexpression of human IL-6 and cyclin D1 in inflammatory myofibroblastic tumor (inflammatory pseudotumor). Lab Invest 2000;80:1121–1126.
Gomez-Roman JJ, Sanchez-Velasco P, Ocejo-Vinyals G, et al. Human herpesvirus-8 genes are expressed in pulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). Am J Surg Pathol 2001;25:624–629.
Yamamoto H, Kohashi K, Oda Y, et al. Absence of human herpesvirus-8 and Epstein–Barr virus in inflammatory myofibroblastic tumor with anaplastic large cell lymphoma kinase fusion gene. Pathol Int 2006;56:584–590.
Smith KJ, Skelton HG . Human herpesvirus 8 DNA sequences in pemphigus: the role of the virus in oncogenic and autoimmune manifestations. Arch Dermatol 1998;134:751.
Yamasaki S, Iino T, Nakamura M, et al. Detection of human herpesvirus-8 in peripheral blood mononuclear cells from adult Japanese patients with multicentric Castleman's disease. Br J Haematol 2003;120:471–477.
Fredricks DN, Martin TM, Edwards AO, et al. Human herpesvirus 8 and sarcoidosis. Clin Infect Dis 2002;34:559–560.
Marioni G, Marchese-Ragona R, Marino F, et al. MALT-type lymphoma and Warthin's tumour presenting in the same parotid gland. Acta Otolaryngol 2004;124:318–323.
Li CF, Ye H, Liu H, et al. Fatal HHV-8-associated hemophagocytic syndrome in an HIV-negative immunocompetent patient with plasmablastic variant of multicentric Castleman disease (plasmablastic microlymphoma). Am J Surg Pathol 2006;30:123–127.
Tedeschi R, Luostarinen T, De PP, et al. Joint Nordic prospective study on human herpesvirus 8 and multiple myeloma risk. Br J Cancer 2005;93:834–837.
Cathomas G, Stalder A, Regamey N, et al. No evidence of HHV-8 infection in patients with pemphigus vulgaris/foliaceus. Arch Dermatol 1998;134:1162.
Knoell KA, Hendrix Jr JD, Stoler MH, et al. Absence of human herpesvirus 8 in sarcoidosis and crohn disease granulomas. Arch Dermatol 2005;141:909–910.
Folk GS, Abbondanzo SL, Childers EL, et al. Plasmablastic lymphoma: a clinicopathologic correlation. Ann Diagn Pathol 2006;10:8–12.
Malnati MS, Dagna L, Ponzoni M, et al. Human herpesvirus 8 (HHV-8/KSHV) and hematologic malignancies. Rev Clin Exp Hematol 2003;7:375–405.
Yamamoto H, Oda Y, Saito T, et al. p53 Mutation and MDM2 amplification in inflammatory myofibroblastic tumours. Histopathology 2003;42:431–439.
Mergan F, Jaubert F, Sauvat F, et al. Inflammatory myofibroblastic tumor in children: clinical review with anaplastic lymphoma kinase, Epstein-Barr virus, and human herpesvirus 8 detection analysis. J Pediatr Surg 2005;40:1581–1586.
Krafft AE, Duncan BW, Bijwaard KE, et al. Optimization of the isolation and amplification of RNA from formalin-fixed, paraffin-embedded tissue: the armed forces institute of pathology experience and literature review. Mol Diagn 1997;2:217–230.
Pan L, Milligan L, Michaeli J, et al. Polymerase chain reaction detection of Kaposi's sarcoma-associated herpesvirus-optimized protocols and their application to myeloma. J Mol Diagn 2001;3:32–38.
Zong JC, Ciufo DM, Alcendor DJ, et al. High-level variability in the ORF-K1 membrane protein gene at the left end of the Kaposi's sarcoma-associated herpesvirus genome defines four major virus subtypes and multiple variants or clades in different human populations. J Virol 1999;73:4156–4170.
Ding Y, Saylors RL, Brown H, et al. Pulmonary inflammatory pseudotumor with HHV-8. Am J Surg Pathol 2002;26:1089–1091.
Author information
Authors and Affiliations
Corresponding author
Additional information
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Departments of the Army or Defence. This is a US Government work, and as such, is in the public domain in the United States of America.
Rights and permissions
About this article
Cite this article
Tavora, F., Shilo, K., Ozbudak, I. et al. Absence of human herpesvirus-8 in pulmonary inflammatory myofibroblastic tumor: immunohistochemical and molecular analysis of 20 cases. Mod Pathol 20, 995–999 (2007). https://doi.org/10.1038/modpathol.3800938
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800938