Abstract
Available results highlight the lack of good level of evidence studies on the pure prognostic value of histological grade. In the present study, the prognostic relevance of histological grade and of its three components, tubule formation, nuclear pleomorphism and mitotic count, was analyzed in a series of 372 patients with node-negative breast cancer treated with locoregional therapy alone until early relapse. Histological grade was determined blindly by two observers and discordance between evaluations was resolved after joint review using a multihead microscope. No relation was observed between histological grade and any of its three components and disease-free survival. Conversely, a significant relation was observed between histological grade and distant metastasis-free survival (at 6 years, 94, 86 and 76% for grades 1, 2 and 3, respectively, P=0.013) as well as overall survival (98, 90 and 86%, P=0.001). A breakdown analysis as a function of the three components showed that neither tubule formation nor nuclear pleomorphism was associated with prognosis, and only mitotic count strongly influenced both distant metastasis-free survival (91, 82 and 74%, P=0.014) and overall survival (97, 87 and 85%, P=0.011). Histological grade suffers from a much higher subjectivity than any other microscopic evaluation of biomarkers as it is the sum of three different morphological features. Within the Italian Network for Quality Assessment of Tumor Biomarkers program we observed that histological grade is an independent prognostic variable, but also that this role is ascribable only to the number of mitotic figures. In conclusion, due to the ever smaller size of diagnosed breast cancers, resulting in less cancer tissue for biofunctional and molecular analysis, mitotic count evaluated under strict quality control conditions seems to be an accurate and feasible prognostic variable.
Similar content being viewed by others
Main
Over the last 20 years, laboratory research has proposed many markers that are related to essential aspects of cell life, proliferation, transformation and apoptosis. Prognostic and predictive biofunctional or molecular markers have been investigated in many studies and tested in clinical settings. Most of them are not determined in all laboratories. Conversely, even in the smallest or least experienced Pathology Unit, the histological grade of breast cancer is generally evaluated along with the histotype, tumor size and presence of metastases in axillary lymph nodes. Histological grade is universally accepted and used by clinicians for patient management, is included in all the consensus classifications of risk for breast cancer patients1, 2, 3, 4 and is often used in treatment decision-making.
However, histological grade suffers from a higher subjectivity than any other microscopic marker evaluation as it is the sum of three different morphological aspects of breast cancer tissue, one of which (nuclear pleomorphism) is poorly reproducible.
A good level of evidence for marker prognostic relevance in breast cancer5 requires studies to be carried out on an adequate number of patients with node-negative tumors not treated with systemic therapy until early relapse. It is very difficult to get an overall picture of the prognostic value of histological grade in breast cancer from literature data. In fact, an extensive PubMed search for original articles in the period 1988–2003 using breast cancer and histological grade as search terms revealed a total of more than 5000 papers.
Conversely, a search limited to the field title using node-negative breast cancer and histological grade produced only five papers published over the same period. This would seem to indicate that the correct assessment of the pure prognostic value of histological grade has not been a central aim or fully investigated, notwithstanding its use by clinicians is a daily practice.
It is our opinion that histological grade, although widely accepted and used as an indicator of risk of relapse and death for breast cancer patients, has never been questioned and has not passed through the validation steps which are nowadays required to attain a good level of evidence for prognostic tumor markers.5
For this reason, we aimed to evaluate the pure prognostic role of histological grade and of its three components, tubule formation, nuclear pleomorphism and mitotic count on a large and consecutive retrospective series of node-negative breast cancer patients treated with locoregional therapy alone until early relapse. More importantly, we guaranteed the reliability and reproducibility of histological grade and single-component determinations through a complete double-blind re-evaluation of all cases.
Materials and methods
Case Series
The prognostic relevance of histological grade was studied on a series of 372 patients with histologically confirmed node-negative (at least 10 axillary lymph nodes examined) breast cancer, radically resected and recruited between 1989 and 1993 by Istituto Oncologico Romagnolo (IOR) and the National Oncology Institute of Bari (IRCCS Bari). The median age of patients was 54 years (range 26–74 years) and about 60% were postmenopausal. About two-thirds of tumors were 2 cm or less in diameter. Slightly less than 70% were estrogen receptor-positive and about 50% were progesterone receptor-positive. All patients received locoregional therapy alone (surgery±radiotherapy), more than 50% underwent quadrantectomy plus radiotherapy and the remaining patients were subjected to mastectomy. No adjuvant systemic treatment was given prior to relapse.
All patients had a clinical, hematological, biochemical and instrumental check-up at 3-month intervals for the first 2 years, every 6 months during the 3rd, 4th and 5th year, and once a year thereafter up to the 10th year. Median follow-up was 75 months (range 3–125 months).
Histological Grade
Paraffin-embedded sections 4–6-μm thick of formalin-fixed breast cancer tissue were conventionally stained with hematoxylin and eosin. Histological grade for individual tumors was determined through the assessment of three morphological features: tubule formation, nuclear pleomorphism and the number of mitotic figures, according to the Elston and Ellis method.6
For each of these features, a score of 1–3 was used. Briefly, for tubule formation the proportion of tumor area displaying tubular structures was defined. When more than 75% of the tumor area was composed of definite tubules, a score of one point was given. Two and three points were assigned to tumors in which the area composed of tubules either ranged from 10 to 75% or represented less than 10%, respectively.
For nuclear pleomorphism, size, shape and outlines of nuclei along with chromatin uniformity were evaluated. When the nuclei were small, with little increase in size compared to normal breast epithelial cells and had regular outlines and uniformity of nuclear chromatin, one point was given. A score of two points was attributed when the cells appeared larger than normal, had open, vesicular nuclei with visible nucleoli, and varied moderately in both shape and size. A pronounced variation in shape and size, especially in concomitance with very large and abnormal nuclei, scored three points.
Mitotic activity was assessed at the periphery of the tumor where active growth is most likely to occur. A minimum of 10 high-power fields were evaluated and strict criteria for the identification of mitotic figures were employed. One-, two- or three-point scores were attributed when up to nine mitotic figures per 10 high-power fields, 10–19 mitotic figures or more than 19 mitotic figures were counted, respectively. The microscope used was a Leitz Ortholux and the field diameter was 0.58 mm.
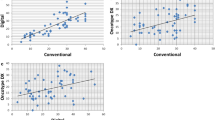
Tumors were graded independently by two pathologists. Any disagreement was resolved by consensus after joint review using a multihead microscope.
Steroid Receptor Content
Estrogen and progesterone receptors were assayed by the dextran-coated charcoal method according to the European Organization for Research and Treatment of Cancer (EORTC).7 Quality control procedures for hormone receptor dosage were co-ordinated by the Italian ad hoc Committee. 10 and 25 fmol/mg were used as cutoff values for ER and PgR content, respectively.
Statistical Analysis
The relationship between histological grade and other clinico-pathological and biological characteristics was investigated in univariate analysis using the χ2-test.
Disease-free survival was calculated as the period from surgery until the first documented evidence of new disease manifestation in locoregional or distant sites or in the contralateral breast, or until death without evidence of disease. Moreover, the distant metastasis-free survival was calculated considering only these metastases as an event, while other events were censored at the time of occurrence. Overall survival was calculated as the period from surgery to death due to any cause.
Univariate analysis was performed tracing Kaplan–Meier curves8 and comparison of survival curves was based on log-rank test.9 The 6-year disease-free, distant metastasis-free and overall survival and their 95% confidence intervals (95% CI) were calculated.
The prognostic relevance of histological grade was evaluated in univariate and multivariate analyses using a Cox regression model10 including tumor size and estrogen and progesterone receptor content.
All P-values were based on two-sided testing and none were adjusted for the multiplicity of the performed tests. Statistical analyses were carried out by SAS statistical software for Windows version 8.2 (SAS, Cary, NC, USA).
Results
The relationship between histological grade and the clinical, pathological or biological characteristics is reported in Table 1. In our series of node-negative breast cancers, 57 (15.3%) tumors were classified as grade 1, 152 (40.9%) as grade 2 and 163 (43.8%) as grade 3.
The different histological grade scores were equally distributed in tumors from younger and older patients as well as in those from premenopausal and postmenopausal patients.
Conversely, a poor differentiation was observed in two-thirds of tumors larger than 2 cm and in only one-third of smaller tumors. This may explain the higher proportion of grade 3 tumors in patients submitted to mastectomy than in those who underwent quadrantectomy. Moreover, the frequency of grade 3 tumors was significantly higher in ductal than in other histotypes and was more than 70 and 65% in estrogen and progesterone receptor-negative tumors, respectively, whereas slightly less than one-third of receptor positive tumors were classified as poorly differentiated.
Of the 372 patients, 98 relapsed, of whom 17 with locoregional and 62 with distant recurrences, and 16 patients developed contro-lateral tumors. Three patients died without evidence of disease.
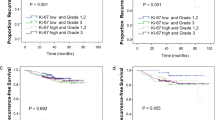
No relation was observed between tumor grade and disease-free survival (6-year disease-free survival 79, 77, 71% for grades 1, 2, and 3, respectively; logrank 2.15, P=0.340) (Figure 1a), whereas a progressively significant decrease in distant metastasis-free survival (94, 86 and 76%; logrank 8.75, P=0.013) was observed as tumor grade increased (Figure 1b). The same finding was observed for overall survival (98, 90 and 86%; logrank 13.19, P=0.001) (Figure 1c).
When prognosis was analyzed as a function of the three histological grade components, neither tubule formation nor nuclear pleomorphism was found to be associated with disease-free, distant metastasis-free or overall survival, and only mitotic count emerged as a prognostic indicator of distant metastasis-free and overall survival (Table 2).
A further analysis aimed at evaluating the possible effect of mitotic count in discriminating patients at different risk of relapse and death within the grade 2 tumor subgroup did not contribute any useful information (data not shown).
Cox regression models including tumor size and estrogen and progesterone receptor status were used to examine the contribution of histological grade and mitotic count in terms of prognostic accuracy. Histological grade maintained its role in overall survival, independently of other factors, but not in distant metastasis-free survival (Table 3, model A). Conversely, mitotic count remained an independent indicator of both distant metastasis-free and overall survival (Table 3, model B).
Discussion
Guidelines3, 5 and consensus statements1, 2 consider a very limited number of biomorphological tumor characteristics to allocate breast cancer patients to different risk categories. This is mainly due to the lack of definitive evidence on the usefulness of tumor prognostic markers, validated according to accepted guidelines.
In routine practice, clinicians may be justifiably perplexed about the information received from the pathology and experimental laboratory. Inconsistencies are often registered for markers that are the expression of the same biological process, such as cell proliferation, or for the same marker determined by different approaches, such as steroid receptors. This makes the overall biofunctional picture of the tumor as well as patient prognosis hazier rather than clearer.
The issue of marker reproducibility is relatively recent and was raised chiefly for the biofunctional indicators and molecular characteristics that have been proposed over time.
Different methods for histological grade evaluation have been used over time. Although some authors have demonstrated that these approaches have almost the same potential for predicting patient survival,11, 12, 13 the basic problem remains that the prognostic value of histological grade has been studied in series of patients who are heterogeneous in terms of stage and treatment and therefore unsuitable for correctly determining the pure prognostic value of any marker. Moreover, the few initiatives of interlaboratory quality controls on histological grade evaluations have mainly highlighted rather unsatisfactory concordance results with correlation coefficients more frequently around 0.55 and never higher than 0.75.12, 14, 15, 16, 17, 18, 19, 20
We aimed to evaluate the pure prognostic role of histological grade and of its three distinct components. The study was conducted on a homogeneous consecutive series of node-negative breast cancer patients treated with locoregional therapy (surgery±radiotherapy) alone according to guidelines. Histological grade determination was performed under strict intralaboratory quality control conditions and within the context of the Italian Network for Quality Assessment of Tumor Biomarkers (INQAT) program. In univariate analysis, histological grade significantly influenced distant metastasis-free and overall survival and the same impact was observed for only mitotic score. Multivariate analysis containing steroid receptor and tumor size variables confirmed the independent role of both histological grade and mitotic count in predicting overall survival. However, regression analysis also demonstrated a significant independent impact of only mitotic count on distant metastasis-free survival. Therefore, and in accordance with other authors,11, 12, 13, 21, 22 the results of the present study highlighted the sole and decisive importance of mitotic count within histological grade determination to predict prognosis and indicated the importance of devoting all due care and attention to mitotic figure counting, as previously demonstrated.23 Unlike other authors,24 we did not highlight the usefulness of mitotic count in improving the accuracy of predicting the clinical outcome of patients with grade 2 tumors. However, a comparison of results is not possible when these are obtained in heterogeneous populations. Our data can be compared, on the basis of case series homogeneity, with those of one other group22 which found, as we did, that both histological grade and mitotic count were unrelated to disease-free survival but significantly and independently related to mortality. However, our study also highlighted an independent impact of histological grade on distant metastasis-free survival.
In terms of standardization and reproducibility, high levels of interobserver agreement are much easier to achieve for one parameter than for the sum of three, especially if one parameter is quantifiable, providing that preanalytical procedures are optimized and scrupulously followed.14, 25, 26, 27
In conclusion, in times when diagnostic tools permit the identification of ever smaller tumors of the breast, resulting in less cancer tissue for biofunctional and molecular analyses, ‘old’ morphometric parameters such as mitotic index are regaining importance and must be evaluated with rigorous interobserver quality control procedures.
References
National Institutes of Health Consensus Development Panel. National Institutes of Health Consensus Development Conference Statement: adjuvant therapy for breast cancer, November 1–3, 2000. J Natl Cancer Inst 2001;30:5–15.
Goldhirsch A, Wood WC, Gelber RD, et al. Meeting highlights: updated international expert consensus on the primary therapy of early breast cancer. J Clin Oncol 2003;21:3357–3365.
Fitzgibbons PL, Page DL, Weaver D, et al. Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124:966–978.
ASCO Expert Panel. Clinical practice guidelines for the use of tumor markers in breast and colorectal cancer: report of the American Society of Clinical Oncology Expert Panel. J Clin Oncol 1996;14:2843–2877.
Hayes DF, Bast RC, Desch CE, et al. Tumor marker utility grading system: a framework to evaluate clinical utility of tumor markers. J Natl Cancer Inst 1996;88:1456–1466.
Elston CW, Ellis IO . Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 1991;19:403–410.
Piffanelli A, Pelizzola D, Giovannini G, et al. Characterization of laboratory working standard for quality control of immunometric and radiometric estrogen receptor assays. Clinical evaluation on breast cancer biopsies. Italian Committee for Hormone Receptor Assays Standardization. Tumorigenesis 1989;75:550–556.
Kaplan EL, Meier P . Non parametric estimation for incomplete observation. J Am Stat Assoc 1958;53:457–481.
Lawless JS . Statistical Models and Methods for Life-time Data. John Wiley and Sons: New York, 1982.
Cox DR . Regression models and life tables. J R Stat Soc 1972;34:187–220.
Genestie C, Zafrani B, Asselain B, et al. Comparison of the prognostic value of Scarff–Bloom–Richardson and Nottingham histological grades in a series of 825 cases of breast cancer: major importance of the mitotic count as a component of both grading systems. Anticancer Res 1998;18:571–576.
Latinovic L, Heinze G, Birner P, et al. Austrian Breast and Colorectal Cancer Study Group. Prognostic relevance of three histological grading methods in breast cancer. Int J Oncol 2001;19:1271–1277.
Frkovic-Grazio S, Bracko M . Long term prognostic value of Nottingham histological grade and its components in early (pT1N0M0) breast carcinoma. J Clin Pathol 2002;55:88–92.
Robbins P, Pinder S, de Klerk N, et al. Histological grading of breast carcinomas: a study of interobserver agreement. Hum Pathol 1995;26:873–879.
Dalton LW, Page DL, Dupont WD . Histologic grading of breast carcinoma. A reproducibility study. Cancer 1994;73:2765–2770.
Raabe NK, Schistad O, Sauer T, et al. Prognosis of radically operated breast carcinoma patients. A retrospective study of 167 consecutive patients with emphasis on histopathological grading, reproducibility and mean nuclear area. APMIS 1997;105:363–370.
Boiesen P, Bendahl PO, Anagnostaki L, et al. Histologic grading in breast cancer—reproducibility between seven pathologic departments. South Sweden Breast Cancer Group. Acta Oncol 2000;39:41–45.
Jacquemier J, Charpin C . Reproducibility of histoprognostic grades of invasive breast cancer. Ann Pathol 1998;18:385–390.
Kronqvist P, Montironi R, Kuopio T, et al. Subjective breast cancer grading. Analyses of reproducibility after application of Bayesian belief networks. Anal Quant Cytol Histol 1997;19:423–429.
Theissig F, Kunze KD, Haroske G, et al. Histological grading of breast cancer. Interobserver, reproducibility and prognostic significance. Pathol Res Pract 1990;186:732–736.
Simpson JF, Gray R, Dressler LG, et al. Prognostic value of histologic grade and proliferative activity in axillary node-positive breast cancer: results from the Eastern Cooperative Oncology Group Companion Study, EST 4189. J Clin Oncol 2000;18:2059–2069.
Page DL, Gray R, Allred DC, et al. Prediction of node-negative breast cancer outcome by histologic grading and S-phase analysis by flow cytometry: an Eastern Cooperative Oncology Group Study (2192). Am J Clin Oncol 2001;24:10–18.
Medri L, Volpi A, Nanni O, et al. Prognostic relevance of mitotic activity in patients with node-negative breast cancer. Mod Pathol 2003;16:1067–1075.
Lynch J, Pattekar R, Barnes DM, et al. Mitotic counts provide additional prognostic information in grade II mammary carcinoma. J Pathol 2002;196:275–279.
Donhuijsen K, Schmidt U, Hirche H, et al. Changes in mitotic rate and cell cycle fractions caused by delayed fixation. Hum Pathol 1990;21:709–714.
Cross SS, Start RD, Smith JH . Does delay in fixation affect the number of mitotic figures in processed tissue? J Clin Pathol 1990;43:597–599.
Start RD, Flynn MS, Cross SS, et al. Is the grading of breast carcinomas affected by a delay in fixation? Virchows Arch A Pathol. Anat Histopathol 1991;419:475–477.
Acknowledgements
We wish to thank Professor Rosella Silvestrini for her invaluable scientific contribution and Gráinne Tierney for editing the manuscript.
The coauthorship of all the following study participants is acknowledged: Angela Riccobon, Paola Rosetti, Roberta Maltoni, Ruggero Ridolfi (Department of Medical Oncology), Franco Padovani(Histopathology Unit), Pierantoni Hospital, Forlì; Oriana Nanni, Patrizia Serra, Istituto Oncologico Romagnolo, Forlì; Amelia Tienghi, Maurizio Marangolo, Bernadette Vertogen, Federica Zumaglini (Department of Medical Oncology), Giuseppe Lanzanova (Histopathology Unit), S Maria delle Croci Hospital, Ravenna; Artur Timurian (Radiotherapy Unit), Vito Lorusso (Medical Oncology Unit), Mario Brandi, Antonio Guido (Senology Unit), National Oncology Institute, Bari, Italy.
This work is supported by Istituto Oncologico Romagnolo, Forlì and by Consiglio Nazionale della Ricerca/Ministero della Istruzione, Università e Ricerca (CNR/MIUR-Progetto Strategico), Grant nos. CU03.00393 and 03.00074.ST97, Rome, Italy. The study was conducted within the Italian Network for Quality Assessment of Tumor Biomarkers (INQAT) program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Volpi, A., Bacci, F., Paradiso, A. et al. Prognostic relevance of histological grade and its components in node-negative breast cancer patients. Mod Pathol 17, 1038–1044 (2004). https://doi.org/10.1038/modpathol.3800161
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800161
Keywords
This article is cited by
-
The prognostic relevance of the mitotic activity index in axillary lymph node-negative breast cancer
Breast Cancer Research and Treatment (2015)
-
Peritumoral vascular invasion and NHERF1 expression define an immunophenotype of grade 2 invasive breast cancer associated with poor prognosis
BMC Cancer (2012)
-
Randomized phase III trial of adjuvant epirubicin followed by cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) versus CMF followed by epirubicin in patients with node-negative or 1–3 node-positive rapidly proliferating breast cancer
Breast Cancer Research and Treatment (2011)
-
Racial differences in the incidence of breast cancer subtypes defined by combined histologic grade and hormone receptor status
Cancer Causes & Control (2010)
-
High cyclin B1 expression is associated with poor survival in breast cancer
British Journal of Cancer (2009)