Abstract
To clarify the genetic aberrations involved in the development and progression of hepatitis C virus-associated hepatocellular carcinoma (HCV-HCC), we investigated DNA copy number aberrations (DCNAs) in 19 surgically resected HCCs by conventional CGH and array CGH. Conventional CGH revealed that increases of DNA copy number were frequent at 1q (79% of the cases), 8q (37%), 6p (32%), and 10p (32%) and that decreases were frequent at 17p (79%), 16q (58%), 4q (53%), 13q (42%), 10q (37%), 1p (32%), and 8p (32%). In general, genes that showed DCNAs by array CGH were usually located in chromosomal regions with DCNAs detected by conventional CGH analysis. Increases in copy numbers of the LAMC2, TGFB2, and AKT3 genes (located on 1q) and decreases in copy numbers of FGR/SRC2 and CYLD (located on 1p and 16q, respectively) were observed in more than 30% of tumors, including small, well-differentiated carcinomas. These findings suggest that these genes are associated with the development of HCV-HCC. Increases of MOS, MYC, EXT1, and PTK2 (located on 8q) were detected exclusively in moderately and poorly differentiated tumors, suggesting that these alterations contribute to tumor progression. In conclusion, chromosomal and array CGH technologies allow identification of genes involved in the development and progression of HCV-HCC.
Similar content being viewed by others
Main
Hepatocellular carcinoma (HCC) is one of the most frequent tumors in the world. HCC is frequently associated with hepatitis B virus (HBV) or hepatitis C virus (HCV) infection. A recent increase in the incidence of HCC is the result of an increase in chronic HCV hepatitis.1, 2
Carcinogenesis is a consequence of the accumulation of genetic and epigenetic alterations in a cell. Chromosomal aberrations frequently occur in cancers. The genetic pathways of hepatocarcinogenesis are still poorly understood, despite extensive studies on the relation of changes in oncogenes and tumor suppressor genes to HCC.
Conventional comparative genomic hybridization (CGH) allows assessment of changes in chromosomal DNA sequence copy numbers across the entire genome3, 4 and provides valuable information regarding genetic alterations in cancer.3, 4, 5, 6, 7, 8, 9 However, CGH cannot detect changes in small chromosomal regions. The reported resolution for CGH is approximately 2 Mb for amplifications and 10–20 Mb for deletions.4, 5, 6 Recent advances in high-throughput technologies for identifying target molecules may permit identification of genes involved in tumors. Array CGH, which is based on microarray technology, allows analysis of DNA copy number aberrations (DCNAs) at the gene level.10, 11
In the present study, we investigated DCNAs in HCC with HCV infection by conventional CGH and array CGH to identify genetic aberrations involved in tumor development and progression.
Materials and methods
Tumor Tissue Specimens and DNA Extraction
We examined 19 cases of surgically resected HCCs (Table 1). Patients consisted of 14 men and five women with an average age of 66.9 years (range, 39–78 years). All patients were positive for anti-HCV antibody. Tumor staging was performed according to the International Union against Cancer TNM classification.12 Tumor tissue specimens were stored frozen at −80°C until use. The study protocol was approved by the Institutional Review Board for Human Use at the Yamaguchi University School of Medicine, and informed consent for this study was obtained from all patients. High-molecular-weight DNA was extracted from each tumor specimen with a DNA extraction kit (SepaGene, Sankojunyaku Co., Tokyo, Japan) according to the manufacturer's instructions.
Conventional CGH
Chromosomal CGH and digital image analyses were carried out according to the protocols described previously.13 Briefly, DNA extracts from tumor tissues and normal lymphocytes were labeled with SpectrumGreen-dUTP and SpectrumRed-dUTP (Vysis Inc., Downers Grove, IL, USA), respectively, by nick translation. Each labeled DNA sample and Cot-1 DNA were dissolved in hybridization buffer and cohybridized onto normal denatured metaphase chromosomes for 72 h at 37°C. The QUIPS™ XL digital image analysis system (Vysis) was used, and increases and decreases of DNA sequence copy number were detected as green/red ratios higher than 1.2 and lower than 0.8, respectively.
Array CGH
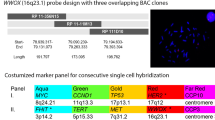
We used commercially available genomic DNA microarray slides (GenoSensorTM Array 300, Vysis Inc.) that were developed for use in microarray-based CGH assays. The microarray contains 287 target DNA clones (P1, PAC, and BAC clones) representing regions that are important in cytogenetics and oncology. DNA clones comprising the desired target sequences are arrayed in target spots of approximately 75–125 μm diameter, and each clone is represented by three target spots.
Labeling DNAs with Fluorochromes for Array CGH
Tumor DNAs and reference DNAs were labeled with 1 mM Cy3 dCTP and 1 mM Cy5 dCTP (Perkin Elmer Life Sciences, Inc., Boston, MA, USA), respectively, according to the manufacturer's protocols (Vysis).
Hybridization in Array CGH
DNAs labeled with fluorochromes were mixed together with Cot-1 DNA, denatured at 80°C for 10 min, and incubated at 37°C for 2 h. The hybridization mixture was then introduced into the hybridization chamber of the microarray slide, and the slide was incubated at 37°C for 72 h. After removal of the hybridization chamber, the microarray slide was rinsed in washing solution (50% formamide/2 × SSC) at 40°C and then transferred into 1 × SSC solution. The microarray slide was counterstained with DAPI IV mounting solution and covered with a coverslip. Hybridized microarray slides were analyzed with a specially designed microarray reader system with software (GenoSensor Reader System and GenoSensor™ Array 300 Software, Vysis) according to the manufacturer's instructions. The test (Cy3)/reference (Cy5) (T/R) ratio was determined automatically for each sample, and P values were assigned to each set of target spots. Increases and decreases in DNA copy number of spots were detected as T/R ratios higher than 1.25 and lower than 0.8, respectively. The P value is the probability that the data value for an individual set of target spots is part of the normal distribution. All ratios were filtered by P value, and only those samples with P values of 0.01 or less were displayed.
Results
Conventional CGH
In all tumors, conventional CGH analysis revealed changes in DNA copy number in at least four chromosomal regions. Copy number alterations detected by CGH in 19 HCC cases are shown in Table 2 and Figure 1. In brief, the frequent DNA copy number increases were detected at 1q (79% of the cases), 8q (37%), 6p (32%), and 10p (32%), and decreases were detected at 17p (79%), 16q (58%), 4q (53%), 13q (42%), 10q (37%), 1p (32%), and 8p (32%). There was no statistical correlation between chromosomal aberrations and clinicopathological parameters.
Array CGH
Array CGH analysis revealed DCNAs at many spots in all tumors. The average number of target clones detected for each sample DNA with changes in copy number was 33.5±21.7(±s.d.). Increases in DNA copy number were observed frequently at LAMC2 and TGFB2 (10 of 19 cases, 53%), and AKT3, MOS, and MYC (6 of 19 cases, 32%). Decreases in DNA copy number were observed frequently for FGR/SRC2 and CYLD (6 of 19 cases, 32%) (Figure 2). Increases of LAMC2, TGFB2, and AKT3 (located on 1q) and decreases of FGR/SRC2 and CYLD (located on 1p and 16q, respectively) were observed in tumors including small, well-differentiated carcinomas. In contrast, increases of MOS, MYC, EXT1, and PTK2 (located on 8q) were detected exclusively in moderately differentiated and poorly differentiated tumors. No significant association was found between DCNAs of target clones and any other clinical factors.
Comparison between Conventional CGH and Array CGH
In all, 80% of target clones identified by array CGH were included in chromosomal regions with DCNAs detected by conventional CGH analysis. As anticipated, increases in LAMC2 and TGFB2 were detected most frequently by array CGH, and the chromosomal regions containing these genes were also found to have DNA copy number gains by conventional CGH. However, changes in copy number for FGR/SRC2 and HRAS (six cases), TNFRSF6B/DCR3 (five cases), and THRA and GSCL (four cases) detected by array CGH were not always found by chromosomal CGH.
Alterations in copy number were detected for chromosomal regions containing HRAS (two of six cases), FGR/SRC2 (three of six cases), TNFRSF6B/DCR3 (one of five cases), GSCL (two of four cases), and THRA (zero of four cases) (Figure 3).
Summary of the chromosomal locations of array clones detected by array CGH, and comparison of conventional CGH and array CGH results. DNA copy number increases are shown on the right side of the chromosome ideograms, and decreases are shown on the left side. Filled circles indicate agreement between results of both types of CGH. Open circles indicate that these changes were identified only by array CGH.
Discussion
Conventional CGH studies have revealed frequent increases of 1q and 8q and decreases of 1p, 4q, 8p, 13q, 16q, and 17p in HCC.13, 14, 15, 16, 17 The present data are comparable with the published results of conventional CGH analyses. Increase of 1q and decrease of 17p, which were observed in 79% of cases in the present study, appear to be crucial changes in hepatocarcinogenesis. We used array CGH to examine DCNAs in genes located on 1q. Copy number increases in the LAMC2 (1q25–31), TGFB2 (1q41), and AKT3 (1q44) genes were frequent in both early and advanced stages of HCC. These three genes may be involved in the development of HCV–HCC. It was reported that transforming growth factor-beta is a potentially important link between fibrosis and neoplasia in the liver, and its expression appears to be increased in HCC, suggesting a tumor-promoting effect.18 Our present data confirmed that the DNA copy number of TGFB2 is increased in HCV–HCC. Although the LAMC2 and AKT3 genes have been implicated in a wide variety of biological processes, their roles in development of HCC have not been reported previously. Our results suggest that these genes might be a new target for amplification in the initiation of HCV–HCC. However, changes in genes on 17p were not detected with this array. Although loss of p53 has been reported in HCC.19, 20, 21 and other solid tumors, it was rare in the present series. Our results indicate that loss of p53 is not a primary factor in the development of HCV-HCC and that other genes on 17p are involved in hepatocellular carcinogenesis. Decreases in copy numbers of the FGR/SRC2 (1p36.1–36.2) and CYLD (16q12–13) genes were also frequent (32% of cases). Loss of heterozygosity at 1p appears to occur at an early stage of carcinogenesis, and loss of heterozygosity at 16q is associated with progression of HCC.22, 23 Our present results together with those of other studies suggest that FGR/SRC2 and CYLD are associated with hepatocarcinogenesis.
DNA copy number increases in four genes located on 8q, MOS (8q11), MYC (8q24.1), EXT1 (8q24.1), and PTK2 (8q24) were observed frequently in moderately and poorly differentiated HCC and rarely in small, well-differentiated tumors, suggesting that copy number increases in these genes act as a driving force for tumor progression. Amplification of MYC has been observed frequently in large HCC nodules, suggesting that it is a late genetic alteration in the progression of HCC.24 The PTK2 gene has also been identified as a target for the amplification event at 8q23–24, and elevated expression of PTK2 is associated with a large tumor size in HCC.25 Our data revealed that four genes were correlated with poor differentiation of HCV-HCC. As the percentage of poorly differentiated tumor cells is higher in large HCC tumors,26 the increase in copy number of the other two genes on 8q, MOS and EXT1, may be closely associated with disease progression.
Comprehensive analyses of genetic imbalances in tumors are essential to clarify the mechanisms of cancer development and progression. With a single experiment, conventional CGH provides extensive information on DNA sequence copy number aberrations in a tumor.3 However, the resolution and sensitivity of conventional CGH are not sufficient to allow identification of specific genes involved in malignant tumors. A more efficient method with higher resolution is required for identification of specific genes. Array CGH technology permits detection of specific genes with copy number variations, and it has been used to screen human solid cancers for genomic imbalances.27, 28, 29, 30, 31, 32, 33, 34 We also used a genomic DNA microarray to investigate DCNAs for 287 target clones in HCV-HCC; however, the number of DNA clones was very small. Array CGH detected DNA copy number alterations for the HRAS, THRA, TNFRSF6B/DCR3, FGR/SRC2, and GSCL genes, whereas conventional CGH did not always detect such changes. This is most likely because CGH cannot detect small changes. The combined use of conventional CGH and array CGH provides valuable and useful information concerning genetic changes associated with carcinogenesis. We used this combined strategy to identify genes related to HCV–HCC. The genetic pathways and molecular targets involved in the development and progression of HCC are complicated and still controversial. Our results may provide several entry points for the identification of candidate genes associated with hepatocarcinogenesis in HCV infection. Further detailed studies are necessary to clarify genetic pathways of the hepatocarcinogenesis.
References
Okuda K . Hepatocellular carcinoma. J Hepatol 2000;32:225–237.
Colombo M . Hepatitis C virus and hepatocellular carcinoma. Bailliere's Clin Gastroenterol 1999;13:519–528.
Kallioniemi A, Kallioniemi OP, Sudar D, et al. Comparative genomic hybridization for molecular cytogenetic analysis of solid tumors. Science 1992;258:818–821.
Kallioniemi OP, Kallioniemi A, Piper J, et al. Optimizing comparative genomic hybridization for analysis of DNA sequence copy number changes in solid tumors. Genes Chromosomes Cancer 1994;10:231–243.
Hermsen MA, Meijer GA, Baak JP, et al. Comparative genomic hybridization: a new tool in cancer pathology. Hum Pathol 1996;27:342–349.
Bentz M, Plesch A, Stilgenbauer S, et al. Minimal sizes of deletions detected by comparative genomic hybridization. Genes Chromosomes Cancer 1998;21:172–175.
Knuutila S, Bjorkqvist AM, Autio K, et al. DNA copy number amplifications in human neoplasms: review of comparative genomic hybridization studies. Am J Pathol 1998;152:1107–1123.
Knuutila S, Aalto Y, Autio K, et al. DNA copy number losses in human neoplasms. Am J Pathol 1999;155:683–694.
James LA . Comparative genomic hybridization as a tool in tumour cytogenetics. J Pathol 1999;187:385–395.
Pinkel D, Segraves R, Sudar D, et al. High resolution analysis of DNA copy number variation using comparative genomic hybridization to microarrays. Nat Genet 1998;20:207–211.
Pollack JR, Perou CM, Alizadeh AA, et al. Genome-wide analysis of DNA copy-number changes using cDNA microarrays. Nat Genet 1999;23:41–46.
Sobin LH, Wittekind C . TNM Classification of Malignant Tumours. 6th edn. UICC, Wiley-Liss: New York, 81–83.
Kusano N, Shiraishi K, Kubo K, et al. Genetic aberrations detected by comparative genomic hybridization in hepatocellular carcinomas: their relationship to clinicopathological features. Hepatology 1999;29:1858–1862.
Marchio A, Meddeb M, Pineau P, et al. Recurrent chromosomal abnormalities in hepatocellular carcinoma detected by comparative genomic hybridization. Genes Chromosomes Cancer 1997;18:59–65.
Wong N, Lai P, Lee SW, et al. Assessment of genetic changes in hepatocellular carcinoma by comparative genomic hybridization analysis: relationship to disease stage, tumor size, and cirrhosis. Am J Pathol 1999;154:37–43.
Sakakura C, Hagiwara A, Taniguchi H, et al. Chromosomal aberrations in human hepatocellular carcinomas associated with hepatitis C virus infection detected by comparative genomic hybridization. Br J Cancer 1999;80:2034–2039.
Guan XY, Fang Y, Sham JS, et al. Recurrent chromosome alterations in hepatocellular carcinoma detected by comparative genomic hybridization. Genes Chromosomes Cancer 2000;29:110–116.
Bissell DM . Chronic liver injury, TGF-beta, and cancer. Exp Mol Med 2001;33:179–190.
Murakami Y, Hayashi K, Hirohashi S, et al. Aberrations of the tumor suppressor p53 and retinoblastoma genes in human hepatocellular carcinomas. Cancer Res 1991;51:5520–5525.
Yumoto Y, Hanafusa T, Hada H, et al. Loss of heterozygosity and analysis of mutation of p53 in hepatocellular carcinoma. J Gastroenterol Hepatol 1995;10:179–185.
Nishida N, Fukuda Y, Ishizaki K, et al. Alteration of cell cycle-related genes in hepatocarcinogenesis. Histol Histopathol 1997;12:1019–1025.
Kuroki T, Fujiwara Y, Tsuchiya E, et al. Accumulation of genetic changes during development and progression of hepatocellular carcinoma: loss of heterozygosity of chromosome arm 1p occurs at an early stage of hepatocarcinogenesis. Genes Chromosomes Cancer 1995;13:163–167.
Tsuda H, Zhang WD, Shimosato Y, et al. Allele loss on chromosome 16 associated with progression of human hepatocellular carcinoma. Proc Natl Acad Sci USA 1990;87:6791–6794.
Wang Y, Wu MC, Sham JS, et al. Prognostic significance of c-myc and AIB1 amplification in hepatocellular carcinoma. A broad survey using high-throughput tissue microarray. Cancer 2002;95:2346–2352.
Okamoto H, Yasui K, Zhao C, et al. PTK2 and EIF3S3 genes may be amplification targets at 8q23–q24 and are associated with large hepatocellular carcinomas. Hepatology 2003;38:1242–1249.
Suehiro T, Matsumata T, Itasaka H, et al. Clinicopathologic features and prognosis of resected hepatocellular carcinomas of varied sizes with special reference to proliferating cell nuclear antigen. Cancer 1995;76:399–405.
Takeo S, Arai H, Kusano N, et al. Examination of oncogene amplification by genomic DNA microarray in hepatocellular carcinomas: comparison with comparative genomic hybridization analysis. Cancer Genet Cytogenet 2001;130:127–132.
Arai H, Ueno T, Tangoku A, et al. Detection of amplified oncogenes by genome DNA microarrays in human primary esophageal squamous cell carcinoma: comparison with conventional comparative genomic hybridization analysis. Cancer Genet Cytogenet 2003;146:16–21.
Daigo Y, Chin SF, Gorringe KL, et al. Degenerate oligonucleotide primed-polymerase chain reaction-based array comparative genomic hybridization for extensive amplicon profiling of breast cancers: a new approach for the molecular analysis of paraffin-embedded cancer tissue. Am J Pathol 2001;158:1623–1631.
Hui AB, Lo KW, Yin XL, et al. Detection of multiple gene amplifications in glioblastoma multiforme using array-based comparative genomic hybridization. Lab Invest 2001;81:717–723.
Hui AB, Lo KW, Teo PM, et al. Genome wide detection of oncogene amplifications in nasopharyngeal carcinoma by array based comparative genomic hybridization. Int J Oncol 2002;20:467–473.
Wilhelm M, Veltman JA, Olshen AB, et al. Array-based comparative genomic hybridization for the differential diagnosis of renal cell cancer. Cancer Res 2002;62:957–960.
Zhao J, Roth J, Bode-Lesniewska B, et al. Combined comparative genomic hybridization and genomic microarray for detection of gene amplifications in pulmonary artery intimal sarcomas and adrenocortical tumors. Genes Chromosomes Cancer 2002;34:48–57.
Ishizuka T, Tanabe C, Sakamoto H, et al. Gene amplification profiling of esophageal squamous cell carcinomas by DNA array CGH. Biochem Biophys Res Commun 2002;296:152–155.
Acknowledgements
This work was supported by Grants-in-Aid for Science Research (No. 14370071) from the Ministry of Education, Science, Sports and Culture of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hashimoto, K., Mori, N., Tamesa, T. et al. Analysis of DNA copy number aberrations in hepatitis C virus-associated hepatocellular carcinomas by conventional CGH and array CGH. Mod Pathol 17, 617–622 (2004). https://doi.org/10.1038/modpathol.3800107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800107
Keywords
This article is cited by
-
The role of BCL9 genetic variation as a biomarker for hepatitis C-related hepatocellular carcinoma in Egyptian patients
Journal of Genetic Engineering and Biotechnology (2022)
-
Single-cell resolved ploidy and chromosomal aberrations in nonalcoholic steatohepatitis-(NASH) induced hepatocellular carcinoma and its precursor lesions
Scientific Reports (2022)
-
Recurrent genetic alterations in hepatitis C-associated hepatocellular carcinoma detected by genomic microarray: a genetic, clinical and pathological correlation study
Molecular Cytogenetics (2014)
-
Array-based comparative genomic hybridization for genomic-wide screening of DNA copy number alterations in aggressive bone tumors
Journal of Experimental & Clinical Cancer Research (2012)
-
CYLD regulates keratinocyte differentiation and skin cancer progression in humans
Cell Death & Disease (2011)