Abstract
We have reported that in thymectomized miniature swine treated with a 12-day course of cyclosporin A that major histocompatibility complex class I-mismatched renal allografts either progress to chronic rejection (progression group; n = 4) or tolerance after acute rejection (recovery group; n = 4). Two types of glomerulopathies, termed acute and chronic allograft glomerulopathy, occur in allografts in this model. Morphological and immunohistochemical studies were performed on serial renal biopsies from both groups to examine the pathogenic mechanisms of acute and chronic allograft glomerulopathy. In acute rejection, acute allograft glomerulopathy developed in both groups by Day 18, with antibody deposition and T cell and macrophage infiltration. In situ DNA nick end-labeling (TUNEL)+ injured glomerular endothelial cells appeared from the early phase, followed by destruction of the glomerular capillary network with segmental mesangiolysis. Thereafter, in the progression group, acute allograft glomerulopathy progressed to chronic allograft glomerulopathy during the development of chronic rejection. This process was associated with persistent T cell and macrophage infiltration, antibody deposition, and TUNEL+ glomerular endothelial injury in the glomeruli. Impaired capillary repair, mesangial cell proliferation, and activation were still noted at Day 100, together with accumulation of mesangial matrix and duplication of glomerular basement membrane. In contrast, in the recovery group, acute allograft glomerulopathy recovered by Day 100, associated with the resolution of cellular infiltration and reduction of antibody deposition. We conclude that the acute and persistent cell- and antibody-mediated rejection against glomerular endothelial cells is the key pathogenic determinant of acute allograft glomerulopathy and progression toward chronic allograft glomerulopathy. Impaired capillary repair and phenotypic change of endothelial and mesangial cells also contribute to the development of chronic allograft glomerulopathy. With the development of tolerance, substantial recovery of acute allograft glomerulopathy can occur after the resolution of glomerular inflammation.
Similar content being viewed by others
Introduction
In addition to recurring and de novo glomerulonephritis, two types of glomerulopathies arising in transplanted renal grafts have been identified (Colvin, 1998; Habib and Broyer, 1993; Habib et al, 1993; Maryniak et al, 1985). The first is termed acute allograft glomerulopathy, characterized by hypercellularity, activated endothelial cells, mononuclear cell infiltration, and webs of periodic acid-Schiff-positive materials (Habib and Broyer, 1993; Habib et al, 1993; Richardson et al, 1981; Tuazon et al, 1987). The second is chronic allograft glomerulopathy, which is characterized by increased mesangial cells and matrix and duplication of the glomerular basement membrane (GBM), with a variable degree of scarring (Colvin, 1998; Habib and Broyer, 1993; Habib et al, 1993; Maryniak et al, 1985). Development of allograft glomerulopathy is often associated with poor prognosis (Habib and Broyer, 1993; Habib et al, 1993; Maryniak et al, 1985), however, the pathogenic mechanisms, intraglomerular events, and sequelae are not well understood.
We previously demonstrated that inbred miniature swine treated with a 12-day course of high dose cyclosporin A develop tolerance to major histocompatibility complex (MHC) class II-matched, class I-mismatched renal allografts (Rosengard et al, 1992). The thymus is necessary for the induction of rapid and stable tolerance in this model, presumably due to central selection mechanisms. When the protocol included thymectomy 21 or 42 days before transplantation, only peripheral mechanisms of tolerance could operate. These thymectomized pigs developed acute vascular rejection between Days 8 to 18 (Yamada et al, 1997, 1999). Subsequently, in half of these animals, this progressed to chronic rejection by Day 100 (Shimizu et al, 2000d, 2002). In the remaining half, rejection resolved gradually with subsequent graft tolerance. The mechanism underlying the diverse course of the two groups in the same experimental protocol may depend on the effect of peripheral mechanisms of tolerance, ie, animals of the recovery group may exhibit more effective peripheral mechanisms.
We recently investigated the mechanisms of chronic renal allograft rejection in this model and demonstrated the process of progressive interstitial fibrosis in chronic rejection (Shimizu et al, 2002). In the present study, we focused on the mechanism of progressive allograft glomerulopathy in this model. An acute allograft glomerulopathy similar to that in humans was noted in all allografts during acute rejection. Our model, therefore, provides a novel opportunity to investigate the pathogenic mechanisms, assess the intraglomerular events, and evaluate the prognosis of acute allograft glomerulopathy during the progression to chronic rejection or recovery from acute rejection. We studied the immune-mediated glomerular injury and the development of acute and chronic allograft glomerulopathy with special emphasis on (1) inflammatory cell infiltration, (2) antibody deposition, (3) endothelial cell death and capillary destruction, and (4) progression of glomerular inflammation.
Results
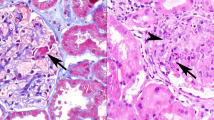
In both the progression and recovery groups, acute allograft glomerulopathy developed by Day 18 (Fig. 1, A and D) with acute vascular rejection and graft dysfunction (Fig. 2). Thereafter, during the development of chronic rejection and graft dysfunction in the progression group, mesangial cell proliferation and matrix accumulation developed by Day 60 (Fig. 1B), and typical chronic allograft glomerulopathy developed by Day 100, characterized by mesangial hypercellularity, matrix accumulation, and GBM duplication (Fig. 1C). In contrast, in the recovery group, the glomerular lesions in acute allograft glomerulopathy improved by Day 100 leaving segmental proliferative lesions based on the resolution of acute vascular rejection and improvement of graft function (Figs. 1, E and F, and 2). No evidence of viral infection, including cytomegalovirus infection was detected in any allografts. In the pretolerized control animals, acute and chronic glomerular lesions did not develop in allografts (data not shown).
Progression (A–C) or recovery (D–F) of acute allograft glomerulopathy. In the progression group, acute allograft glomerulopathy occurs by Day 18 (A) and gradually progresses to chronic allograft glomerulopathy from Day 60 (B) to Day 100 (C). In the recovery group, acute allograft glomerulopathy also develops by Day 18 (D), however, this gradually recovers on Day 60 (E) to Day 100 (F), leaving mild segmental proliferative lesions. A to F, Periodic acid silver methenamine stain, ×500.
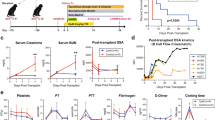
Graft function (A), antidonor cytotoxic T lymphocyte (CTL) reactivity in cell mediated lympholysis (CML) assay (B), and circulating antidonor major histocompatibility complex (MHC) class I IgG (C) in the progression (• or ▪: n = 4) and recovery (• or □: n = 4) groups. (□) and (□) in (B) represent values of CTL responses against third party type antigen in animals of the progression (□: n = 4) and recovery (□: n = 4) groups. Note that animals of the progression group show long-term graft dysfunction (A), prolonged donor specific CTL reactivity (B), and persistent production of antidonor class I antibody (C). In contrast, animals of the recovery group show a transient elevation in Cr (A), development of donor specific hyporesponsiveness by Day 30 (B), and reduced levels of circulating antidonor class I IgG by Day 60 (C). B and C, Values are expressed as mean ± sd.
During the development of acute and chronic allograft glomerulopathy in the progression group, antidonor cytotoxic T lymphocyte (CTL) reactivity maintained similar to pretransplant levels by Day 60 (Fig. 2B), and antidonor class I IgG in serum was detected through Day 60 (Fig. 2C). In contrast, the animals in the recovery group developed specific hyporesponsiveness to the donor class I antigens by Day 30 and had transient antidonor class I IgG in serum. Later samples (Day 100) had only low levels of cell-mediated lympholysis (CML) or no detectable antibody in either group.
Acute Allograft Glomerulopathy in the Progression and Recovery Groups
In the early phase, cellular infiltration in glomeruli was similar between the progression and recovery groups (Figs. 3 and 4). CD3+ T cells and macrophages accumulated in the glomeruli by Day 8 and reached peak levels on Day 18 (Figs. 3 and 4). No CD21+ B cells were found. The majority of lymphocytes were CD8+ with a smaller number of CD4+ cells, some expressing the activation marker interleukin 2 receptor (IL2R; CD25). Deposition of IgM and IgG was also seen in glomeruli as capillary and mesangial pattern by Day 18 in both groups (Fig. 5, A and B). In parallel with the accumulation of inflammatory cells and antibody deposition in glomeruli, terminal deoxynucleotidyl transferase (TdT)-mediated dUTP-biotin nick end-labeling (TUNEL)+ cells began to appear in glomerular capillaries and were prominent during the development of acute allograft glomerulopathy (Fig. 5, C and D). The majority of TUNEL+ glomerular cells did not express CD3 but expressed Griffonia (Bandeiraea) Simpliciforia Isolectin B4 (GS-IB4), suggesting that these cells were of endothelial origin. Electron microscopic examination showed loss of glomerular endothelial cells and the presence of apoptotic and necrotic dead cells (Fig. 6). Loss of immunostaining for GS-IB4 confirmed that the glomerular capillary network was destroyed segmentally with loss of endothelial cells (Fig. 5H). The remaining glomerular endothelial cells were hypertrophied and lacked fenestration (Fig. 6), and some had proliferating cell nuclear antigen (PCNA)+ nuclei (Fig. 5, E and F), suggesting proliferation and activation of endothelial cells in damaged glomeruli. In expanded mesangial areas, focal and segmental mesangiolysis was seen and some of the remaining mesangial cells expressed PCNA and α-actin (Fig. 5G), indicating that mesangial cells also began to proliferate and activate.
Inflammatory cell infiltration in acute allograft glomerulopathy on Day 18. The glomeruli contain numerous CD3+ (A) and CD8+ (B) cells and macrophages (D) with an activated phenotype (IL-2R) (E), but less prominent CD4+ cells (C) and no CD21+ B cells (F). A, CD3 stain; B, CD8 stain; C, CD4 stain; D, macrophage stain; E, IL-2R stain; F, CD21 stain; ×600.
Glomerular infiltrating cells in the progression (•; n = 4) and recovery (□ n = 4) groups. In both groups, numerous CD3+ cells (CD8 > CD4), macrophages, and IL-2R+ cells infiltrate during the early phase. Thereafter, a significant number of T cells, macrophages, and IL-2R+ cells persist in the progression group, although they gradually disappear in the recovery group. A to E, Values are expressed as mean ± sd. * p < 0.05, ** p < 0.01, *** p < 0.001.
Acute allograft glomerulopathy on Day 18. IgM (A) and IgG (B) deposition is detected in glomeruli. Double staining with terminal deoxynucleotidyl transferase (TdT)-mediated dUTP-biotin nick end-labeling (TUNEL) (blue) and CD3 (brown) (C) or GS-IB4 (brown) (D) show that TUNEL+ cells do not express CD3 are GS-IB4+. Double staining with proliferating cell nuclear antigen (PCNA) (blue) and CD3 (brown) (E), GS-IB4 (brown) (F), or α-actin (G) demonstrate that PCNA+ cells do not express CD3 but express GS-IB4 or α-actin. Marked destruction of glomerular capillary network is indicated by the loss of GS-IB4 staining (H). A and B, ×600; C to G, ×800; H, ×700.
Electron microscopy reveals loss of endothelial cells and activation of the remaining endothelial cells in acute allograft glomerulopathy on Day 18. A, Destruction of glomerular capillaries occur with loss of endothelial cells. Note the presence of apoptotic bodies in these areas (×5000). B, Marked swelling of the glomerular endothelium is found with loss of fenestration, indicative of activated endothelial cells (×5000).
Progression of Acute Allograft Glomerulopathy in the Progression Group
In the progression group, acute allograft glomerulopathy progressed to chronic allograft glomerulopathy by Day 100. During this process, CD3+ cells, macrophages, and diffuse deposition of IgM and IgG persisted until Day 60 (Figs. 4 and 7). During this period, frequent TUNEL+ GS-IB4+ damaged endothelial cells were observed, suggesting persistent immune-mediated glomerular endothelial injury (Figs. 8, A and B, and 9). Numerous PCNA+ GS-IB4+ proliferating endothelial cells were also seen in damaged glomeruli (Figs. 8, C and D, and 9). However, capillary endothelial repair was incomplete by Day 100, characterized by the presence of a few small glomerular capillaries and endothelial cell separation from GBM (Fig. 8, G and H). In widespread mesangial areas, PCNA+ and/or α-actin+ mesangial cells were prominent, and mesangial matrix gradually accumulated with the development of glomerular sclerosis (Figs. 8, E and F, and 9). Glomerular hypertrophy progressed during the development of chronic allograft glomerulopathy (Fig. 9). In electron microscopic examination, injured glomerular endothelial cells separated from GBM in acute allograft glomerulopathy (Fig. 10A). Thereafter, during the development of chronic allograft glomerulopathy, mesangial interposition developed with formation of a new basement membrane under activated endothelial cells (ie, duplication of GBM) (Fig. 10B), and by Day 100, the GBM was thickened and duplicated and extensive deposition of extracellular matrix was noted in the capillary wall (Fig. 10C).
Progression group showing CD3+ cell infiltration (A, B) and IgG deposition (C, D) on Day 30 (A, C) and Day 60 (B, D). CD3+ cell infiltration and IgG deposition are detected in glomeruli by Day 60 during the development of chronic allograft glomerulopathy. A and B, CD3 stain, ×800; C and D, IgG stain, ×600.
Progression group showing TUNEL (blue) and GS-IB4+ (brown) damaged endothelial cells (A, B), PCNA (blue) and GS-IB4+ (brown) proliferating endothelial cells (C, D), PCNA (blue) and α-actin+ (brown) activated and proliferating mesangial cells (E, F), and incomplete recovery of capillary structure in GS-IB4 staining (G, H) on Day 30 (A, C, E, G) and Day 60 (B, D, F, H). During the development of chronic allograft glomerulopathy, endothelial cell injury, mesangial cell proliferation, and activation is still evident at Day 60. Capillary repair with endothelial cell proliferation occurs after acute allograft glomerulopathy, however, glomerular capillary structure shows incomplete recovery at Day 60. A to F, ×800; G, H, ×700.
Damaged endothelial cells (TUNEL+ GS-IB4+) (A), proliferating endothelial cells (PCNA+ GS-IB4+) (B), proliferating and activated mesangial cells (PCNA+ α-actin+) (C), α-actin+ activated mesangial areas (μm2) (D), glomerular hypertrophy (glomerular tuft area: μm2) (E), and areas of accumulation of mesangial matrix (μm2) (F) in the progression (•; n = 4), the recovery (□ n = 4), and the pretolerized control (□; n = 2) groups. A, Values are expressed as mean ± sem. B to F, Values are expressed as mean ± sd. * p < 0.05, ** p < 0.01, *** p < 0.001.
Changes in glomerular capillaries and glomerular basement membrane (GBM) in the progression (A–C) and recovery (D) groups on Day 30 (A), Day 60 (B), and Day 100 (C, D). In acute allograft glomerulopathy, injured capillaries separate from GBM with widening subendothelial space. Thereafter, in the progression group, mesangial interposition develops by Day 60, and thickening and duplicated GBM develops by Day 100. By contrast, in the recovery group, glomerular capillaries contact GBM on Day 100, resulting in focal and mild duplication of the GBM. A to D, ×4000.
Recovery from Acute Allograft Glomerulopathy in the Recovery Group
In the recovery group, resolution of acute allograft glomerulopathy was noted by Day 100 leaving only segmental mesangial hypercellularity. Before recovery from acute allograft glomerulopathy, a progressive decrease in T cell and macrophage infiltration was noted together with reduced antibody deposition in glomeruli (Figs. 4 and 11, A and B). There was also a decrease in TUNEL+ GS-IB4+ damaged endothelial cells (Figs. 9 and 11C). After a reduction in the number of damaged endothelial cells, glomerular capillary network recovered with endothelial cell proliferation (PCNA+ GS-IB4+) by Day 60 (Fig. 11, D and F). PCNA+ and α-actin+ mesangial cells diminished (Fig. 11E), and glomerular hypertrophy, which was detected with acute allograft glomerulopathy around Day 30, also gradually resolved by Day 100 (Fig. 9). Electron microscopic examination showed the presence of normal capillary lumina, and endothelial cells contacted on GBM by Day 60. Only rare segmental duplication of GBM was evident by Day 100 (Fig. 10D).
Recovering glomeruli in the recovery group on Day 60. Only a few T cells (A), little IgG deposition (B), no injured endothelial cells (C), a few proliferating endothelial cells (D), and a small number of proliferating and activated mesangial cells (E) are observed. Capillary repair appears by Day 60 (F). A, CD3 stain; B, IgG stain; C, double staining with TUNEL (blue) and GS-IB4 (brown); D, double staining with PCNA (blue) and GS-IB4 (brown); E, double staining with PCNA (blue) and α-actin (brown); F, GS-IB4 stain. A, C to E, ×800; B, ×600; F, ×700.
Discussion
Our study is the first to describe a reproducible experimental large animal model of acute allograft glomerulopathy that shows either progression to chronic allograft glomerulopathy or recovery. These processes evolve in the absence of immunosuppressive drugs or viral infection and require histoincompatibility, suggesting that specific antidonor immune responses may mediate these pathologic features. In this model, cellular- and antibody-mediated rejection directed at glomerular endothelial cells seem to be crucial pathogenic determinants of acute allograft glomerulopathy as well as this progression to chronic allograft glomerulopathy.
Similarly, in humans, either T cells or antidonor antibody are associated with acute allograft glomerulopathy (Olsen et al, 1995; Trpkov et al, 1996; Tuazon et al, 1987). In our model, the glomeruli contained numerous CD3+ cells (CD8+ > CD4+) and macrophages but no B cells, a similar phenotypic proportion to that described in humans (Bishop et al, 1986; Olsen et al, 1995; Tuazon et al, 1987). Donor type MHC class I specific CTL were evident in peripheral blood. In the humoral immunity, deposition of IgM and IgG was seen in glomeruli, and anti-MHC class I donor type IgM and IgG were present in the circulation. These findings are consistent with the hypothesis that infiltrating CTL and immunoglobulin deposits are directed against MHC class I antigens on glomerular endothelial cells.
T cell-mediated cytotoxicity plays an important role in allograft rejection through the destruction of MHC incompatible cells by lysis or apoptosis of target cells (Doherty, 1993; Kägi et al, 1994). Antibody- and complement-mediated cell injury also plays an important role in graft rejection by cell lysis, apoptosis, or both of target cells by terminal complement components (Sato et al, 1999; Schwartzman and Cidlowski, 1993; Shimizu et al, 2000a). The TUNEL method can detect DNA damage in the process of apoptosis and necrosis (cell-lysis) (Gavrieli et al, 1992; Mundle, 1995). This method, therefore, may have a practical value in the detection of cell injury in antibody- and cell-mediated graft rejection. Indeed, numerous TUNEL+ cells were observed during the development of allograft glomerulopathy. After T cell and macrophage infiltration and antibody deposition in glomeruli, the first abnormality recognized in acute allograft glomerulopathy was endothelial cell labeling with TUNEL, suggesting that glomerular endothelium is the primary target in acute allograft glomerulopathy.
Repeat biopsies of human renal allografts demonstrate that some cases of chronic allograft glomerulopathy evolve after an episode of acute allograft glomerulopathy (Habib and Broyer, 1993; Habib et al, 1993; Maryniak et al, 1985). The present study also demonstrated that acute allograft glomerulopathy progressed to chronic allograft glomerulopathy, associated with persistent T cell and macrophage infiltration, prolonged antibody deposition, and continuation of glomerular endothelial cell injury. We, therefore, suspect that acute and persistent immune-mediated rejection directed at the glomerular endothelium induces acute allograft glomerulopathy, which progresses to chronic allograft glomerulopathy, and is probably a key event in the pathogenesis.
Following injury of glomerular endothelial cells, activation and proliferation of the remaining endothelial and mesangial cells and glomerular hypertrophy were noted during the progression of chronic allograft glomerulopathy. Activation of endothelial cells is thought to contribute to progression of tissue rejection, because activated endothelial responses include increased expression of cell adhesion and antigen-presentation molecules, enhanced procoagulant activity, and production of chemokines, cytokines, and growth factors (Ballermann, 1997; Briscoe and Cotran, 1993). Activated mesangial cells are also involved in the development of glomerular sclerosis, as proinflammatory effector cells, through the release of various oxidants, prostaglandins, cytokines, and extracellular matrix (Johnson, 1994; Sterzel and Rupprecht, 1997). Glomerular hypertrophy plays a crucial role in the pathogenesis of glomerular sclerosis (Nagata and Kriz, 1992; Rennke and Klein, 1989). Responses against endothelial and capillary injury, including activation and proliferation of remaining endothelial cells as well as mesangial cells and glomerular hypertrophy, may together contribute to the progression of chronic allograft glomerulopathy. In human renal allograft glomerulopathy, the mesangium has α-actin, associated with cell proliferation (PCNA+) (Alpers et al, 1992) and with poor prognosis (Ko et al, 1997). In the present study, morphological examination showed that an increased number of PCNA+ and α-actin+ cells in glomeruli was an early and potentially useful diagnostic marker of progression from acute to chronic allograft glomerulopathy.
In this model, destruction of the glomerular capillary network occurred in acute allograft glomerulopathy. This implies that capillary repair is necessary for recovery from acute allograft glomerulopathy. In experimental glomerular disease, complete capillary repair leads to full recovery of the glomerular architecture (Iruela-Arispe et al, 1995; Kitamura et al, 1995; Masuda et al, 2001; Shimizu et al, 1998). In contrast, incomplete repair of the capillary network is associated with development of glomerular sclerosis (Masuda et al, 2001; Shimizu et al, 1997). In our results, during progressive allograft glomerulopathy, capillary repair was incomplete with prolonged TUNEL+ endothelial cell injury. Thus, capillary repair may play an important role in the prognosis of allograft glomerulopathy.
Acute allograft glomerulopathy is resistant to conventional antirejection therapy and has a poor prognosis (Habib and Broyer, 1993; Habib et al, 1993; Tuazon et al, 1987). However, this form of glomerulopathy is not always associated with a poor outcome (Olsen et al, 1995), suggesting that recovery can be expected at least in some cases. Indeed, treatment using FK506, an antilymphocyte preparation (ATG or OKT3), combined with physical removal of the antibody (plasmapheresis or plasma exchange) can reverse the clinical course in some cases of acute allograft glomerulopathy (Faull et al, 1988; Hibberd et al, 1991; Woodle et al, 1996). The recovery group in our study demonstrated a gradual recovery of injured glomeruli, probably reflecting reduced antibody deposition, resolution of T cell and macrophage infiltration, and diminished immune-mediated glomerular endothelial cell injury. Transplant tolerance develops in these animals (Yamada et al, 1997). We conclude that several strategies of aggressive therapy, which can result in resolution of antidonor immune response, including active tolerance induction therapy, might be necessary in the treatment of acute and progressive allograft glomerulopathy.
In summary, cell- and antibody-mediated rejection directed at the glomerular endothelium is a crucial determinant of acute allograft glomerulopathy and progression to chronic allograft glomerulopathy. The incomplete repair of the capillary network, and the activation and proliferation of remaining endothelial cells and mesangial cells, contributes to the progression of chronic allograft glomerulopathy. However, cell- and antibody-mediated acute allograft glomerulopathy may recover following resolution of glomerular inflammation and immune activation.
Materials and Methods
Animals, Surgery, and Immunosuppression
Transplant donors and recipients were selected from our herd of inbred, Massachusetts General Hospital miniature swine at 5 to 7 months of age. Recombinants swine lymphocyte antigen (SLA)gg (class Ic/c, class IId/d) animals were donors, and SLAdd (class Id/d, class IId/d) animals were recipients of orthotopic kidney grafts to achieve a transplantation of SLA class II matched, class I mismatched kidneys (Rosengard et al, 1992; Yamada et al, 1997, 1999). In all animals, a complete (n = 6) or partial (n = 2) thymectomy was carried out 21 to 42 days before kidney transplantation (Yamada et al, 1997, 1999). Cyclosporin A was provided by Novartis Pharmaceutical Corporation (Hanover, New Jersey) and was administered daily in a single infusion dose of 10 to 13 mg/kg (adjusted to maintain a blood level of 400–800 ng/ml) for 12 consecutive days, commencing on the day of kidney transplantation. Based on the results of our previous study (Shimizu et al, 2000d, 2002), we divided eight thymectomized animals into two groups based on their prognosis. One was the progression group (complete thymectomy: n = 3, partial thymectomy: n = 1), which progressed to chronic rejection by Day 100. The other was the recovery group (complete thymectomy: n = 3, partial thymectomy: n = 1), which was characterized by recovery from acute vascular rejection (NIH-CCTT type II) with development of transplant tolerance by Day 100. To examine the intragraft features associated with nonimmunological factors, the kidney graft was transplanted into a nonthymectomized animal that was already tolerant to the donor before transplant, using the same procedures without cyclosporin A treatment (pretolerized control group: n = 2). In each group, sequential wedge kidney biopsies were obtained on postoperative Days 8, 11, 18, 30, 60, and 100. The experimental protocol was approved by the Ethics Review Committee for Animal Experimentation of Massachusetts General Hospital.
Histological Examination
For light microscopic examination, tissue was fixed with 10%-buffered formalin and embedded in paraffin. Tissues were stained with hematoxylin and eosin, periodic acid-Schiff, and periodic acid silver methenamine.
To detect the phenotype of infiltrating cells, a standard avidin-biotin-peroxidase complex (ABC) technique (Shimizu et al, 2000b) was applied using frozen sections. Primary antibodies included antiswine monoclonal antibodies BB23–8E6 (anti-CD3), 74–12–4 (anti-CD4), 76–2–11 (anti-CD8), BB6–11C9 (anti-CD21; B cell), K231–3B2 (anti-interleukin 2 receptor; IL2R), and 74–22–15A (antimacrophage) (Saalmüller, 1996), and antihuman CD3 polyclonal antibody (Dako, Glostrup, Denmark). The antihuman CD3 antibody was confirmed to react with swine pan T cells using swine thymus, lymph nodes, and spleen. Glomerular endothelial cells were identified as those expressing galactose (α1–3) galactose (gal(α1–3)gal), which is known as a major xenoantigen, expressed uniformly on pig vascular endothelial cells but not on glomerular epithelial and mesangial cells (Shimizu et al, 2000b). Gal(α1–3)gal on endothelial cells can be detected by the immunoperoxidase technique using biotin-labeled Griffonia (Bandeiraea) Simpliciforia Isolectin B4 (GS-IB4; Sigma Chemical Company, St. Louis, Missouri) on formalin-fixed paraffin embedded sections. Gal(α 1–3)gal is also present weakly on pig inflammatory cells. Therefore, we determined glomerular endothelial cells carefully, using not only expression of GS-IB4 but also its location and morphology. Activated mesangial cells were identified by the expression of α-actin. In renal glomeruli, α-actin is not expressed in mesangial cells, endothelial cells, and epithelial cells, however, only activated mesangial cells express α-actin (Alpers et al, 1992; Johnson et al, 1992; Ko et al, 1997). Formalin-fixed paraffin embedded sections were stained by the ABC technique using anti-α smooth muscle actin antibody (Dako). Proliferating cells were identified by the expression of PCNA. To optimize the detection of PCNA, formalin-fixed paraffin embedded sections were heated in a microwave (for 2 × 5 minutes in 0.01 M sodium citrate, pH 6.0, in a 750-watt microwave oven at full power followed by immediate chilling to 4° C) followed by treatment with 1/1000 dilution of PC10 (Dako) (Lan et al, 1995). Double immunostaining with PCNA and CD3, α-actin, or GS-IB4 was performed using the two-color staining technique (Shimizu et al, 2000c). In the first step, sections were stained with PC10, incubated with alkaline phosphatase-labeled antimouse IgG (Vector Laboratories, Burlingame, California) with a blue reaction product (Alkaline Phosphatase Substrate Kit III; Vector Laboratories). After denaturalization of bound antibody molecules, which used first staining (Nakane, 1968), sections were stained with antihuman CD3 or anti-α-actin antibodies, biotin-labeled antigoat or mouse antibodies (Dako), and were visualized using hydrogen peroxide (H2O2) containing 3,3′-diaminobendizine (DAB) (Research Genetics, Huntsville, Alabama) (brown reaction product). Sections for GS-IB4 were stained with biotin-labeled GS-IB4, ABC, and H2O2 containing DAB. In negative controls, the primary antibody was omitted or substituted with an irrelevant antibody.
To detect antibody deposition in glomeruli, frozen tissue sections were stained with FITC-conjugated goat antiswine IgG or IgM (both from Kirkegaard and Perry Laboratories, Gaithersburg, Maryland) and examined under an epifluorescence microscope (Zeiss, Oberkochen, Germany).
In histological sections, fragmented nuclear DNA associated with apoptosis or occasionally cell necrosis was labeled by the TdT-mediated TUNEL method (Gavrieli et al, 1992). After deparaffinization and incubation with proteinase K, sections were rinsed in TdT buffer and incubated with TdT 1:25 and biotinylated-dUTP 1:20 in TdT buffer for 60 minutes at 37° C. Biotinylated nuclei were detected with avidin-peroxidase and H2O2 containing DAB. Double staining with TUNEL and CD3 or GS-IB4 was performed by immunoalkaline phosphatase using the TUNEL method, followed by 0.1% avidin and 0.01% biotin, an antibody to CD3 or avidin-biotinylated GS-IB4, and the ABC technique with H2O2 containing DAB. In control sections, the antibody dUTP or TdT was omitted in these procedures.
For electron microscopic examination, the kidney tissue was fixed with 2.5% glutaraldehyde solution in phosphate buffer (pH 7.4) and postfixed with 1% osmium tetroxide, dehydrated, and embedded in Epon 812. Ultrathin sections were stained with lead citrate.
Quantification of Histological Findings
In each kidney specimen, 40 cross-sections of glomeruli were examined sequentially for the following: (1) glomerular infiltrating cells; the number CD3+, CD8+, CD4+, CD21+, and IL2R+ cells and macrophages per glomerular cross-section; (2) injured endothelial cells; the number of TUNEL+ and GS-IB4+ cells per glomerular cross-section, (3) proliferating endothelial cells; the number of PCNA+ and GS-IB4+ cells per glomerular cross-section; and (4) proliferating and activated mesangial cells; the number of PCNA+ and α-actin+ cells per glomerular cross-section. For the evaluation of (5) glomerular hypertrophy (glomerular tuft area in glomerular cross-section), (6) activated mesangial cells (α-actin+ area in glomerular cross-section), and (7) mesangial matrix accumulation (periodic acid silver methenamine+ area in glomerular cross-section), 40 cross-sections of glomeruli were assessed by Luzex IIIU digital image processor analyzer (Nireco, Tokyo, Japan), and expressed in μm2, as described previously (Masseroli et al, 1998; Nishimoto et al, 1997; Tóth and Takebayashi, 1998). These results were expressed as the mean ± sd or sem, and statistical analysis was performed using the unpaired Student’s t test.
CML Assay
CML assays were performed using peripheral blood leukocytes (PBL), as described previously (Yamada et al, 1997, 1999). Briefly, lymphocyte cultures containing 4 × 106 responder and 4 × 106 irradiated (25G) stimulator PBL in 2 ml of medium were incubated for 6 days at 37° C in 7.5% CO2 and 100% humidity. Bulk cultures were harvested and effector cells were tested on 51Cr-labeled blasts. The tests were run at serially diluted ratios (100:1, 50:1, 25:1, 12.5:1). After 5.5 hours of effector cell incubation with the 5 × 103 specific targets, supernatants were harvested and 51Cr release was determined on a gamma counter (Micromedics, Huntsville, Alabama). Maximum lysis was obtained with 1% solution of the nonionic detergent NP-40 (BLR, Rockville, Maryland). Baseline levels were measured as the rate of spontaneous release of 51Cr from 5 × 103 targets. The data were expressed as percentage of specific lysis: [experimental release (cpm) − spontaneous release (cpm)]/maximum release (cpn) − spontaneous release (cpm)] × 100. The results of the progression and the recovery groups were expressed as the mean ± sd.
Flow Cytometry
The presence of antidonor class I (SLA class Ic/c) IgM and IgG in the serum of experimental swine was detected by indirect flow cytometry using a Becton-Dickinson FACScan (Sunnyvale, California) (Yamada et al, 1999) and recombinant SLA PBL to determine the SLA-binding specificity of the antibody. For staining, 1 × 106 cells per tube of recombinant SLA PBL or donor-type PBL (SLAgg, class Ic/c, class IId/d) were resuspended in Hank’s balanced salt solution (Invitrogen, Carlsbad, California) containing 0.1% BSA and 0.05% NaN3 and incubated for 30 minutes at 4° C with decomplemented test sera. FITC-labeled goat antiswine IgM or IgG polyclonal antibodies were used as secondary reagents (BD PharMingen, San Diego, California). After a final wash, cells were analyzed by flow cytometry using propidium iodide gating to exclude dead cells. Both normal pig serum and pretransplant sera from each respective experimental animal were used to ensure specific binding. Data were expressed as median fluorescence intensity, and the results in the progression and the recovery groups were expressed as the mean ± sd.
References
Alpers CE, Hudkins KL, Gown AM, and Johnson RJ (1992). Enhanced expression of “muscle-specific” actin in glomerulonephritis. Kidney Int 41: 1134–1142.
Ballermann BJ (1997). Endothelial responses to immune injury. In: Nilson EG and Couser WG, editors. Immunologic renal disease. Philadelphia: Lippincott-Raven, 627–654.
Bishop GA, Hall BM, Duggin GG, Horvath JS, Sheil AGRS, and Tiller DJ (1986). Immunopathology of renal allograft rejection analyzed with monoclonal antibodies to mononuclear cell markers. Kidney Int 29: 708–717.
Briscoe DM and Cotran RS (1993). Role of leukocyte-endothelial cell adhesion molecules in renal inflammation: In vitro and in vivo studies. Kidney Int 44 (Suppl 42): S27–S34.
Colvin RB (1998). Renal transplant pathology. In: Jennette JC, Olson JL, Schwartz MM, and Silva FG, editors. Heptinstall’s pathology of the kidney, 5th ed. Philadelphia: Lippincott-Raven, 1409–1540.
Doherty PC (1993). Cell-mediated cytotoxicity. Cell 75: 607–612.
Faull RJ, Russ GR, Nicholls C, and Mathew TH (1988). Early glomerular rejection in sensitized patients: Treatment with plasma exchanges and antithymocyte globulin. Transplant Proc 20: 14–16.
Gavrieli Y, Sherman Y, and Ben-Sasson SA (1992). Identification of programmed cell death in situ via specific labeling of nuclear DNA fragmentation. J Cell Biol 119: 493–501.
Habib R and Broyer M (1993). Clinical significance of allograft glomerulopathy. Kidney Int 44 (Suppl 43): S95–S98.
Habib R, Zurowska A, Hinglais N, Gubler MC, Antignac C, Niaudet P, Broyer M, Gagnadoux MF, Lacoste M, Beziau A, and Sich M (1993). A specific glomerular lesion of the graft: Allograft glomerulopathy. Kidney Int 44 (Suppl 42): S104–S111.
Hibberd AD, Nanra RS, White KH, and Trevillian PR (1991). Reversal of acute glomerular renal allograft rejection: A possible effect of OKT3. Transplant Int 4: 264
Iruela-Arispe L, Gordon K, Hugo C, Duijvestijn AM, Claffey KP, Reilly M, Couser WG, Alpers CE, and Johnson RJ (1995). Participation of glomerular endothelial cells in the capillary repair of glomerulonephritis. Am J Pathol 147: 1715–1727.
Johnson RJ (1994). The glomerular response to injury: Progression or resolution? Kidney Int 45: 1769–1782.
Johnson RJ, Floege J, Yoshimura A, Iida H, Couser WG, and Alpers CE (1992). The activated mesangial cell: A glomerular “myofibroblast”? J Am Soc Nephrol 2: S190–S197.
Kägi D, Vignaux F, Ledermann B, Bürki K, Depraetere V, Nagata S, Hengartner H, and Golstein P (1994). Fas and perforin pathways as major mechanisms of T cell-mediated cytotoxicity. Science 265: 528–530.
Kitamura H, Sugisaki Y, and Yamanaka N (1995). Endothelial regeneration during the repair process following Habu-snake venom induced glomerular injury. Virchows Arch 427: 195–204.
Ko YJ, Sugar L, Zaltzman J, and Paul LC (1997). α-smooth muscle actin and collagen deposition in dysfunctional renal transplants. Transplantation 63: 156–169.
Lan HY, Mu W, Nikolic-Paterson DJ, and Atkins RC (1995). A novel, simple, reliable and sensitive method of multiple immunoenzymic staining: Use of microwave oven heating to block antibody cross-reactivity and retrieve antigens. J Histochem Cytochem 43: 97–102.
Maryniak RK, First MR, and Weiss MA (1985). Transplant glomerulopathy: Evolution of morphologically distinct changes. Kidney Int 27: 799–806.
Masseroli M, O’Valle F, Andúar M, Ramíez C, Góez-Morales M, Luna JD, Aguilar M, Aguilar D, Rodríuez-Puyol M, and Del Moral RG (1998). Design and validation of a new image analysis method for automatic quantification of interstitial fibrosis and glomerular morphometry. Lab Invest 78: 511–522.
Masuda Y, Shimizu A, Mori T, Ishiwata T, Ohashi R, Ishizaki M, Asano G, Sugisaki Y, and Yamanaka N (2001). Vascular endothelial growth factor enhances glomerular capillary repair and accelerates resolution of experimentally-induced glomerulonephritis. Am J Pathol 159: 599–608.
Mundle SD (1995). The two in situ techniques do not differentiate between apoptosis and necrosis but rather reveal distinct patterns of DNA fragmentation in apoptosis. Lab Invest 72: 611–612.
Nagata M and Kriz W (1992). Glomerular damage after uninephrectomy in young rats. II. Mechanical stress on podocytes as a pathway to sclerosis. Kidney Int 42: 148–160.
Nakane PK (1968). Simultaneous localization of multiple tissue antigens using the peroxidase-labeled antibody method. A study of pituitary glands of the rat. J Histochem Cytochem 16: 557–560.
Nishimoto K, Shiiki H, Nishino T, Uyama H, Iwano M, and Dohi K (1997). Reversible glomerular hypertrophy in adult patients with primary focal segmental glomerulosclerosis. J Am Soc Nephrol 8: 1668–1678.
Olsen S, Spencer E, Cookfield S, Marcussen N, and Solez K (1995). Endocapillary glomerulitis in the renal allograft. Transplantation 59: 1421–1425.
Rennke HG and Klein PS (1989). Pathogenesis and significance of nonprimary focal and segmental glomerulosclerosis. Am J Kidney Dis 13: 443–456.
Richardson WP, Colvin RB, Cheeseman SH, Tolkoff-Rubin NE, Herrin JT, Cosimi AB, Collins AB, Hirsch MS, McCluskey RT, Russell PS, and Rubin RH (1981). Glomerulopathy associated with cytomegalovirus viremia in renal allografts. N Engl J Med 305: 57–63.
Rosengard BR, Ojikutu CA, Guzzetta PC, Smith CV, Sundt TM III, Nakajima K, Boorstein SM, Hill GS, Fishbein JM, and Sachs DH (1992). Induction of specific tolerance to class I-disparate renal allografts in miniature swine with cyclosporin. Transplantation 54: 490–497.
Saalmüller A (1996). Characterization of swine leukocyte differentiation antigens. Immunol Today 17: 352–354.
Sato T, van Dixhoorn MGA, Prins FA, Mooney A, Verhagen N, Muizert Y, Savill J, van Es LA, and Daha MR (1999). The terminal sequence of complement plays an essential role in antibody-mediated renal cell apoptosis. J Am Soc Nephrol 10: 1242–1252.
Schwartzman RA and Cidlowski JA (1993). Apoptosis: The biochemistry and molecular biology of programmed cell death. Endocrine Rev 14: 133–151.
Shimizu A, Kitamura H, Masuda Y, Ishizaki M, Sugisaki Y, and Yamanaka N (1997). Rare glomerular capillary regeneration and subsequent capillary regression with endothelial cell apoptosis in progressive glomerulonephritis. Am J Pathol 151: 1231–1239.
Shimizu A, Masuda Y, Kitamura H, Ishizaki M, Sugisaki Y, and Yamanaka N (1998). Recovery of damaged glomerular capillary network with endothelial cell apoptosis in experimental proliferative glomerulonephritis. Nephron 79: 206–214.
Shimizu A, Masuda Y, Kitamura H, Ishizaki M, Ohashi R, Sugisaki Y, and Yamanaka N (2000a). Complement-mediated killing of mesangial cells in experimental glomerulonephritis: Cell death by a combination of apoptosis and necrosis. Nephron 86: 152–160.
Shimizu A, Meehan SM, Kozlowski T, Sablinski T, Ierino FL, Cooper DKC, Sachs DH, and Colvin RB (2000b). Acute humoral xenograft rejection: Destruction of the microvascular capillary endothelium in pig-to-nonhuman primate renal grafts. Lab Invest 80: 815–830.
Shimizu A, Meehan SM, Yamada K, Sachs DH, and Colvin RB (2000c). Acceptance reaction: Intragraft events associated with tolerance to renal allografts in miniature swine. J Am Soc Nephrol 11: 2371–2380.
Shimizu A, Yamada K, Sachs DH, and Colvin RB (2000d). Intragraft events preceding chronic renal allograft rejection in a modified tolerance protocol. Kidney Int 58: 2546–2558.
Shimizu A, Yamada K, Sachs DH, and Colvin RB (2002). Persistent rejection of peritubular capillaries and tubules is associated with progressive interstitial fibrosis. Kidney Int 61: 1867–1879.
Sterzel RB and Rupprecht HD (1997). Glomerular mesangial cells. In: Nilson EG and Couser WG, editors. Immunologic renal disease. Philadelphia: Lippincott-Raven, 595–626.
Tóth T and Takebayashi S (1998). Glomerular hypertrophy as a prognostic marker in childhood IgA nephropathy. Nephron 80: 285–291.
Trpkov K, Campbell P, Pazderka F, Cockfild S, Solz K, and Halloran PF (1996). Pathologic features of acute renal allograft rejection associated with donor-specific antibody. Transplantation 61: 1586–1592.
Tuazon TV, Schneeberger EE, Bhan AK, McCluskey RT, Cosimi AB, Schooley RT, Rubin RH, and Colvin RB (1987). Mononuclear cells in acute allograft glomerulopathy. Am J Pathol 129: 119–132.
Woodle ES, Spargo B, Ruebe M, and Charette J (1996). Treatment of acute glomerular rejection with FK 506. Clin Transpl 10: 266–270.
Yamada K, Gianello PR, Ierino FL, Lorf T, Shimizu A, Meehan SM, Colvin RB, and Sachs DH (1997). Role of the thymus in transplantation tolerance in miniature swine. I. Requirement of the thymus for rapid and stable induction of tolerance to class I-mismatched renal allografts. J Exp Med 186: 497–506.
Yamada K, Ierino FL, Gianello PR, Shimizu A, Colvin RB, and Sachs DH (1999). Role of the thymus in transplantation tolerance in miniature swine. III. Surgical manipulation of the thymus interferes with stable induction of tolerance to class I mismatched renal allografts. Transplantation 67: 1112–1119.
Acknowledgements
This work was supported in part by grants from the National Institutes of Health: RO1-AI 31046, PO1-H218646, and PO1-HL 18646; and the Japan Society for the Promotion of Science, Grant-in-Aid for Scientific Research (C2 642 4578).
Portions of this study were previously published in abstract form (Shimizu A, Yamada K, Meehan SM, Sachs DH, and Colvin RB (1996). Progressive allograft glomerulopathy arises in a modified tolerance induction protocol in inbred pigs. J Am Soc Nephrol 7:1895). The expert technical assistance of Ms. Patricia Della Pelle and Dr. Joseph Ambroz is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shimizu, A., Yamada, K., Sachs, D. et al. Mechanisms of Chronic Renal Allograft Rejection. II. Progressive Allograft Glomerulopathy in Miniature Swine. Lab Invest 82, 673–686 (2002). https://doi.org/10.1097/01.LAB.0000017370.74529.89
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.LAB.0000017370.74529.89
This article is cited by
-
Dendritic cells and macrophages in the kidney: a spectrum of good and evil
Nature Reviews Nephrology (2014)
-
Mycophenolic acid inhibits oleic acid-induced mesangial cell activation through both cellular reactive oxygen species and inosine monophosphate dehydrogenase 2 pathways
Pediatric Nephrology (2009)