Abstract
The molecular analysis of serum is an important field for the definition of potential diagnostic markers or disease-related protein alterations. Novel proteomic technologies such as the mass spectrometric-based surface-enhanced laser desorption/ionization (SELDI) ProteinChip® technique facilitate a rapid and reproducible analysis of such protein mixtures and affords the researcher a new dimension in the search for biomarkers of disease. Here, we have applied this technology to the study of a cohort of serum samples from well-characterized renal cell carcinoma patients for the identification of such proteins by comparison to healthy controls. We detected and characterized haptoglobin 1 α and serum amyloid α-1 (SAA-1) as disease related, in addition to an as-yet-unidentified marker of 10.84 kDa. Of particular note is the detection of multiple variants of SAA-1 in multiplex that have not been described in the sera of cancer patients. SAA-1 is detected as full-length protein, des-Arginine and des-Arginine/des-Serine variants at the N terminus by SELDI. In addition, we could also detect a low-abundant variant minus the first five N-terminal amino acids. Such variants may impact the function of the protein. We conclude the technique to be a reproducible, fast and simple mode for the discovery and analysis of marker proteins of disease in serum.
Similar content being viewed by others
Main
Recent technical advances in the analysis of complex protein mixtures for the detection, interaction, and function or modification of a given protein or sets of proteins of interest have been greatly influenced by the application of mass spectrometry (MS) to clinical biomedicine. One technology of note that is being employed across a broad spectrum of protein analyses is surface-enhanced laser desorption/ionization (SELDI) mass spectrometry, first introduced by Hutchens and Yip1 and reviewed by Wright,2 which combines activated or chromatographic surfaces (ProteinChip® Arrays) with solid-state time of flight (TOF) MS for the high-throughput, sensitive analysis of proteins in mixtures. A rapid, sensitive and reproducible ‘protein profile’ of proteins within a complex mixture that are retained on the array by chemical, physical or functional properties is achieved according to mass in high resolution, affording the detection or visualization of known and unknown proteins that are relevant to the disease state.
The technique has already been used for the discovery of disease-related biomarkers in biological fluids. Examples include the detection of hepatocarcinoma–intestine–pancreas/pancreatitis-associated protein I (HIP/PAP I) in pancreatic juice of pancreatic ductal adenocarcinoma,3 as well as the study of a known candidate biomarker of disease: the quantitation of serum prostate-specific membrane antigen (PSMA) in malignant prostate cancer.4 The application of powerful analytical algorithm software to the analysis of high volumes of SELDI data, particularly the profiling of serum, has led to the ability to distinguish breast cancer from normal tissue;5 neoplastic from non-neoplastic disease of the ovary;6 and prostate cancer from both benign hyperplasia and healthy men7 by pattern analysis, with a predictive accuracy of more than 90%. An overview of current and future techniques available combining MS with proteomic studies is provided by Aebersold and Mann8 and, further, its clinical application to the detection of cancer is discussed by Srinivas et al.9
Renal cell carcinoma (RCC) accounts for approximately 3% of adult solid tumors, the incidence of which has risen by 30% from the previous decade.10 Clinical blood analyses of patients presenting with the disease have revealed negative prognosis factors, including anemia at the time of diagnosis, hypercalcemia, hypoalbuminemia, and elevations in serum alkaline phosphatase, erythropoietin levels and erythrocyte sedimentation rate.11 However, no satisfactory serum-born biomarker of the disease has yet been identified. It is of paramount importance to apply newly developed proteomic technologies to study the serology of such a disease for the discovery of novel disease-related proteins or early markers of disease. Commonly, RCC is discovered after symptomatic presentation such as gross hematuria, and 30% will have metastasized.12 Thus, a biomarker or a pattern of biomarkers would revolutionize the detection of early, more treatable disease as well as serve as a monitoring agent for the disease during an after therapy.
Traditionally, proteomic analyses of complex protein mixtures such as serum have largely relied upon two-dimensional gel electrophoretic studies for the characterization of tumor markers,13 but suffer from resolution and reproducibility problems, especially in the lower-mass range. Conversely, SELDI MS can offer highly resolved proteomic patterns according to mass especially in the low-mass range, is reproducible and can be operated in a high-throughput fashion.
In this study, we describe the application of SELDI MS technology to the study of the proteome of serum, utilizing presurgical serum samples from a cohort of well-documented RCC patients. By comparison with sera of normal, healthy donors, we characterized several upregulated proteins and correlated the overall sensitivity of the technique with a standard quantitative method (enzyme-linked immunosorbent assay (ELISA)) using an identified protein. The technique clearly visualized in multiplex different acute and chronic inflammatory parameters associated with the disease. Furthermore, the technique revealed a previously rarely observed variant of the acute-phase protein, serum amyloid α-1 (SAA-1) to be present within the sera of seven RCC patients and readily detectable simultaneously with other disease-related proteins. The high-throughput format of the ProteinChip Array has, to our knowledge, for the first time facilitated a study of the simultaneous distribution of SAA-1 and its variants within multiple cancer sera.
Materials and methods
All chemicals were supplied by Sigma, Taufkirchen, Germany, unless otherwise stated.
Serum Samples
Serum was prepared by collection of blood in 9 ml Monovette® sterile serum collection tubes (Sarstedt, Nuembrecht, Germany), and stood on end overnight at 4°C to allow for blood cells to coagulate and settle. In all, 1 ml of serum was pipetted under sterile conditions from the top of the tube, transferred to sterile polypropylene tubes and stored at –70°C until analysis. In total, 25 patient serum samples were prepared from renal carcinoma patients 1 day prior to undergoing surgical removal of the tumor within the urology departments of the Evangelical Hospital in Goettingen, Germany, and the University Clinic, Tuebingen, Germany, between November 2001 and December 2003. In all, 26 control, ‘normal’ serum samples, age- and sex-matched as closely as possible to the patients, were obtained from blood donors registered in the University of Tuebingen Hospital Blood Bank, Tuebingen, Germany.
Serum Preparation and SELDI TOF Protein Profiling
40 μl volumes of the serum samples were diluted in 60 μl 8 M urea, 1% (w/v) CHAPS in phosphate-buffered saline (PBS) and depleted of albumin with the use of a Cibacron blue spin column (Bio Rad, Munich, Germany). Columns were washed twice with 100 μl 1 M urea, 0.125% (w/v) CHAPS and the eluted fractions combined. The albumin-depleted samples were stored at –70°C until analysis. Protein profiling of the serum samples was performed using the eight-spot format WCX2 (Weak Cation Exchange) ProteinChip Arrays (Ciphergen Biosystems, Fremont, CA, USA) at pH 4.0 (binding buffer, 100 mM sodium acetate, 0.05% (v/v) triton X-100), and measured in parallel using a 96-well format Bioprocessor (Ciphergen Biosystems, Fremont, CA, USA). Arrays were prepared as follows: 15 μl of albumin-depleted serum were diluted with 60 μl of pH 4.0 binding buffer, vortexed for 20 s and then centrifuged at high speed to pellet debris. Each array was pre-equilibrated 2 × 5 min in 100 μl binding buffer on a horizontal shaker before sample addition. Sample supernatant was added and incubated for 45 min with gentle agitation. After incubation, the sample was removed, and each spot washed for 3 × 5 min with binding buffer on the agitator. After washing, each ProteinChip Array was dismantled carefully from the bioprocessor and washed briefly in 5 ml high-performance liquid chromatography (HPLC)-grade water in a 15 ml conical polystyrene tube. After air drying, 2 × 0.6 μl saturated sinapinic acid matrix (Ciphergen Biosystems, Fremont, CA, USA) suspended in 49.5% H2O, 50% acetonitrile (ACN), 0.5% trifluoroacetic acid (TFA) was spotted and air dried. Analysis was performed with a ProteinChip Reader (Ciphergen Biosystems, Fremont, CA, USA) using an automated data collection protocol within the ProteinChip Software (version 3.0), collecting data to a maximum of 80 kDa. Laser intensity was set to 220 U, detector sensitivity to 10 and the focus mass to 8000 Da. An average of 130 laser shots were collected. Data were also collected from the same array at different subpositions, but at higher laser intensity (250) to facilitate analyses of proteins in the higher mass range (∼10–100 kDa). The ProteinChip Reader was calibrated externally using vasopressin, somatostatin and bovine insulin β chain, and the spectra were normalized with the software using total ion current.
Protein Identification by In-gel Trypsin Digestion and Peptide Fingerprinting
Serum samples were analyzed by both one-dimensional (1-D) polyacrylamide gel electrophoresis (PAGE) and two-dimensional (2-D) gel electrophoresis. For 1-D PAGE, the Novex NuPAGE® precast gel system (Invitrogen, Karlsruhe, Germany) was employed. Briefly, 20 μl of albumin-depleted serum was fully reduced and loaded upon a 4–12% gradient Bis–Tris precast gel. Gels were stained using the SimplyBlue™ SafeStain Coomassie system (Invitrogen, Karlsruhe, Germany) according to the manufacturer's instructions. Gel bands were excised and stored at −80°C until digested with trypsin.
For 2-D gel electrophoresis, proteins were first separated according to pI using ReadyStrip IPG strips (Bio Rad, Munich, Germany) between pH 3 and 10. Briefly, 6 μl of serum were diluted to 150 μl in sample buffer (8 M urea, 0.5% (v/v) carrier ampholite pH 3–10, 3% (w/v) CHAPS, 60 mM dithreothreitol (DTT), 1% (w/v) bromophenol blue) before strip rehydration and focusing using a Protean IEF cell (Bio Rad, Munich, Germany). Before the second dimension, IPG strips were equilibrated with first 1% (w/v) DTT, then 2.5% (w/v) iodacetamide sequentially within a buffer containing 6 M urea, 30% (w/v) glycerol and 2% (w/v) SDS in 0.05 M Tris-HCl buffer, pH 8.8, for 20 min each. Proteins were resolved in the second dimension by SDS-PAGE according to the Laemmli system, using 12% polyacrylamide gel, and spots were stained by Coomassie brilliant blue. As before, spots were excised and stored at −80°C before tryptic digestion.
Excised gel bands/spots were diced to approximately 1 mm3 and transferred into 0.5 ml microcentrifuge tubes, washed once for 15 min with HPLC-grade water before being resuspended in 40 μl 50% (v/v) ACN/water and incubated for a further 15 min. Gel pieces were then shrunk with 40 μl 100% ACN before its removal by pipette and replacement with 40 μl of 100 mM NH4HCO3. In all, 40 μl ACN was added to make a 1:1 solution, incubated for 15 min before removal of all buffer and vacuum-centrifugation to complete dryness. A measure of 40 μl of trypsin (Promega, Mannheim, Germany) digestion solution (10 ng/μl trypsin in 5 mM CaCl2, 50 mM NH4HCO3 digestion buffer) was added per cup, and incubated for 45 min on ice, after which the solution was removed and discarded. Gel pieces were resuspended in 40–60 μl digestion buffer (without trypsin) and incubated overnight at 37°C. The gel piece suspension was then acidified with 10 μl 2% (v/v) TFA in water and after 2 min the supernatant was removed and stored in a fresh, clean microcentrifuge tube. Tryptic peptides were eluted from the gel pieces by covering them with 0.1% (v/v) TFA in water and sonicated for 30 min in an ultrasonic bath. The extraction step was repeated twice, first with 30% and (v/v) ACN/water then with 60% (v/v) ACN/water, before the supernatants were pooled and vacuum centrifuged to 50% of the original volume to remove TFA and ACN. Finally, 10 μl formic acid were added, the samples vortexed and stored at −80°C until measurement by matrix-assisted laser desorption/ionization (MALDI)-ReTOF MS on a Voyager DE-STR (Applied Biosystems, Foster City, CA, USA). Peptide fingerprints were exported for database matching, and subsequent identification using the Mascot program, available through www.matrixscience.com. Sequencing of peptides of interest was performed by fragmentation analysis using an Ultraflex™ TOF/TOF (Bruker Daltonik GmbH, Bremen, Germany) mass spectrometer.
ProteinChip Immunoaffinity Capture of Serum Amyloid α (SAA)
Immunoaffinity capture was performed with the use of a Protein G Array (Ciphergen Biosystems, Fremont, CA, USA), following the manufacturer's protocol. A mouse monoclonal anti-SAA antibody (Abcam Ltd, Cambridge, UK) was diluted to a concentration of 0.2 μg/μl in PBS, 2 μl of which were pipetted per spot on the array before incubation for 1 h at room temperature in a humidified chamber. Unbound monoclonal antibody (mAb) were removed by inserting the array into a conical tube containing 8 ml of wash buffer A (0.5% (v/v) triton X-100 in PBS) and agitated for 10 min on a horizontal shaker. The same washing step was repeated two more times with 5 min agitation, before the array was removed and dried around the spots with a lint-free tissue without touching the spot surface itself. The array was then inserted into an eight-well Bioprocessor for sample incubation. Serum samples, depleted of albumin as described earlier, were diluted 1:1 with wash buffer B (0.1% (v/v) triton X-100 in PBS) to a volume of 100 μl and pipetted into their designated wells. The array was incubated for 1 h at room temperature on a horizontal shaker to facilitate antibody–antigen capture, after which the array was removed from the Bioprocessor and washed 1 × 10 min followed by 2 × 5 min in 8 ml wash buffer B. Finally, the array was washed once in 1 mM HEPES buffer before air drying and 2 × 0.6 μl of saturated sinapinic acid matrix was added to each spot. The array was measured in a PBS II instrument using the following parameters: high mass set to 170 kDa, laser intensity to 258 U, detector sensitivity to 10, optimization range 8000–15 000 Da and a focus mass of 12 000 Da. In all, 120 laser shots were averaged on each spot.
Phenotyping of Sera for Haptoglobin Polymorphism
Determination of each patient's haptoglobin phenotype (1-1, 2-1, 2-2) was achieved with the use of a native PAGE method followed by utilizing the peroxidase activity displayed by the haptoglobin–hemoglobin complex. To ensure maximal haptoglobin-hemoglobin complexing in the serum sample, serum was preincubated with hemolysate. Hemolysate was prepared by collecting 9 ml of whole blood in an ethylenediamine tetracetic acid (EDTA) Monovette® before overnight storage upright at 4°C. The blood sample was then centrifuged at 800 g; plasma was removed and discarded. The red pellet was resuspended to 10 ml in PBS, transferred to a 50 ml conical tube and made up to 50 ml in PBS. Centrifugation at 800 g, followed by removal of supernatant, acted to wash the cells. Cells were resuspended in 30 ml 4 mM EDTA, stirred for 1 min before the addition of 10 ml 3.5% (w/v) NaCl, 4 mM EDTA. The hemolysate was vortexed briefly before centrifugation at 800 g to remove all white cells and unlysed red blood cells. Hemolysate was transferred to a fresh 50 ml tube and stored at 4°C until use. In all, 1 μl of serum was mixed with 19 μl of a 1:100 dilution (in PBS) of hemolysate and left to stand for 5 min at room temperature. A measure of 10 μl of a 3 × native PAGE sample buffer (30 ml glycerol, 18.8 ml 1 M Tris-HCl (pH 6.8), 1.5 ml 1% (w/v) bromophenol blue made to 100 ml in water) was added and mixed before samples were loaded onto a 3–8% gradient Tris-Acetate NuPAGE® precast gel (Invitrogen, Karlsruhe, Germany). Tris-glycine was used as the running buffer (25 mM Tris, 250 mM glycine), adjusted to pH 8.6, and the samples were run at a constant 150 V, gradient 18–7 mA for 2.75 h. Visualization of the developed haptoglobin bands is easier against a red background, so the gel was first stained with a 1% (w/v) rhodamine solution, after which the gel was incubated for 5 min in a 1:1 water-diluted leucomalachite green peroxidase-development buffer (0.2 g leucomalachite green, 0.02 g EDTA in 25 ml 40% (v/v) acetic acid with 0.06% (v/v) H2O2). Bands appeared as blue/black and each sample was typed according to the migration pattern.
Haptoglobin occurs etiologically as three phenotypes: 1-1, 2-2 and 2-1. The 1-1 phenotype contains only 1-α (9.2 kDa), the 2-2 has only 2-α (15.9 kDa), whereas the 2-1 phenotype contains both forms of the α chain. Bands are interpreted on the gel according to their migration distances and/or presence or absence of multimeric complexes (Figure 4).
Haptoglobin phenotyping of sera using a native PAGE system coupled with in-gel peroxidase activity of the haptoglobin–hemoglobin complex for band development. The 1-1 phenotype is characterized by its single band due as the 1-α can only form a dimer. The 2-α chain, structurally a repeat of the 1-α sequence, is able to form tandem repeats of itself in conjunction with the β chain; thus, it can form larger complexes, for example trimers and tetramers. The many permutations of the complex are seen in the appearance of multiple bands in the 2-1 and 2-2 phenotypes. The 2-2 phenotype is characterized by the lack of a band at the 1-α region.
Quantitative Analysis of Serum Samples for SAA
The concentration of SAA was determined in both patient and normal sera using a commercially available ELISA in sandwich format, performed according to the manufacturer's instructions (Tridelta Development Ltd, Maynooth, Ireland).
Results
Protein Profiling by SELDI MS Reveals RCC-related Proteins in Patient Serum
Serum samples from 25 patients (15 male, 10 female; aged 33–83 years) diagnosed with RCC were collected within 24 h before undergoing surgical removal of the tumor. Histological grading, referring to the tumor status, grading, lymph node status and metastases, was performed postsurgically according to the revised TNM system.
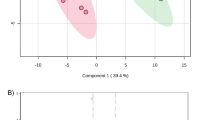
Serum samples from patients as well as corresponding age- and sex-matched normal donors were initially depleted of albumin using affinity dye beads. Protein profiling of all samples was performed in parallel using Weak Cation Exchange (WCX2) ProteinChip Arrays at pH 4.0 binding conditions, and data were collected by a ProteinChip Reader (Model PBSII) (Ciphergen Biosystems, Fremont, CA, USA). Reproducible profiles according to mass accuracy and relative peak intensities were achieved for both patient and normal samples; obvious additional peaks were present only in patient sera. A cluster of three peaks was seen at m/z (mass to change ratio) ∼11.4, ∼11.5 and ∼11.7 kDa in seven patients, with an eighth possessing ∼11.5, ∼11.7 but not the ∼11.4. None of the peaks were detected in normal controls. Other peaks of note separating the patients from the controls, according to relative abundance and higher frequency of detection, occurred at m/z ∼9.2 and ∼10.84 kDa. A summary of peaks of interest from patient profiles as well as a selection of shared peaks is outlined in Table 1. Figure 1 shows representative profiles of three patients (R4, R9, R14) and two control samples. Highlighted masses are those of proteins of interest seen with a higher frequency in multiple RCC patients than in normal samples, and the peak intensity is a reflection of the protein's relative abundance.
SELDI profile of three patient sera (R4, R9, R14) and two normal (N6, N8) between mass ranges 8 and 16.5 kDa, performed on WCX2 surface at pH 4.0 binding conditions and measured with a laser intensity set to 250 (high); the protein profile revealing peaks of interest at approximately 9.2, 10.8 kDa as well as a cluster at 11.4–11.7 kDa, which are not present in control serum spectra (dotted boxes), or in lower relative abundances. Other differential, patient-related peaks visualized in this figure were determined to be too infrequently detected in all patients to be considered peaks of interest.
Serum Amyloid 1-α and Haptoglobin 1-α are Identified as Differential Proteins
Proteins of interest as well as a selection of common, shared proteins between patient sera and their normal counterparts could be identified with a combination of 1-D SDS-PAGE, 2-D gel electrophoresis and in-gel tryptic digestion followed by mass spectrometric peptide fingerprinting. Common proteins visualized on the WCX2 surface at pH 4.0 included transthyretin (average mass 13 761 Da), α and β globin (average mass 15 126 and 15 867 Da, respectively) as well as apolipoprotein A-I with a high intensity (average mass 28 078 Da). Figure 2 displays the protein profile of patient R9, between 8 and 16.5 kDa, in conjunction with the identities and observed molecular masses of both peaks of interest and normal, shared peaks. Other proteins separated by either 1- or 2-D electrophoresis were also identified that were not visible on the WCX2 surface under the selected binding conditions, such as apolipoprotein C-III (average mass 8764 Da), apolipoprotein A-II (average mass 8707 Da) as well as C-reactive protein (C-RP) from patient sera (average mass 23 047 Da). These proteins are not visualized under these binding conditions due to their acidic pI values.
SELDI profile of patient R9 serum, using a laser intensity of 250. Proteins identified by in-gel tryptic digestion and peptide mapping are labelled and fit accurately to the expected average masses as given in Table 1. The RCC-related protein at m/z 10 835.3 Da remains unidentified. The peak corresponding to SAA-1 des-R occurs at m/z 11 526.5.
The proteins of interest observed at ∼9.2 and ∼11.7 kDa were identified as haptoglobin 1-α (Hpt 1a) and serum amyloid 1-α (SAA-1), respectively, by both 1- and 2-D separation followed by in-gel tryptic digestion and peptide sequencing by MALDI fragmentation analysis using patient R9 serum (Figure 3). The database average masses agree very closely with the m/z observed in the samples, m/z 9191.6 Da being the closest fit for Hpt 1a (average mass 9192 Da) and m/z 11 683.2 Da for SAA-1 (average mass 11 682 Da) (Figure 3b). The peak detected at m/z 10 835 Da is as yet unidentified.
(a) Hpt 1a (average mass 9192.25 Da) as visualized by SELDI on a cationic exchange surface and binding conditions of pH 4 using patient R4 serum. Lower laser intensity (220) was employed to enhance peak resolution. Hpt 1a could be detected in 15 of 25 patients as well as 12 of 26 normal serum samples. (b) SAA-1 (average mass 11 682.7 Da) and derivatives as detected in patient R6. The second and third peaks correspond to SAA-1 des-R (R—156.188 Da, average mass) and subsequently SAA-1 des-RS (S—87.078 Da, average mass). (c) MALDI-ReTOF spectra of tryptic digest of SAA-1 excised from 2-D gel electrophoresis of patient serum. SAA-1 des-RS is confirmed by the generation of a new tryptic peptide at the expected monoisotopic mass of 1463.6953 Da correlating to positions 3–15. Tryptic fragments corresponding to positions 48–62 (expected monoisotopic mass 1456.7179) and positions 2–15 (expected monoisotopic mass 1550.7274), the latter confirming a mixture of des-R and des-RS variants. (d) SELDI immunoaffinity capture of SAA and its derivatives. Monoclonal anti-SAA antibody was immobilized on a Protein G Array in order to capture SAA from albumin-depleted serum. Peaks corresponding to SAA-1 and SAA-1 des-R were resolved (upper panel) in patient R6, while none could be clearly resolved from normal serum (N20, lower panel).
Haptoglobin phenotyping of the patient serum was performed by native gel electrophoresis followed by peroxidase staining to further confirm the identity of the 9.2 kDa peak (Figure 4, left panel). Haptoglobin occurs in vivo as polymers of an α and β chain complex, existing as three phenotypes due to a longer and shorter form of the alpha chain: the longer (Hpt 2a) being a partial duplication of a portion of the shorter (Hpt 1a). The 1-1 phenotype contains only Hpt 1a (9.2 kDa) and the 2–2 only Hpt 2a, whereas the 2-1 phenotype contains both polymorphs. The β chain is a conserved, 45 kDa protein. Polymerization of the complex relies upon the interaction of the alpha chains with each other via disulfide bridges, the 1-1 phenotype existing only as a homodimer as Hpt 1a chain possesses a single site for disulfide linking (Figure 5, right panel). However, the partial duplication within the 2-α chain facilitates a second disulfide bridge to be formed within the complex and subsequently variable-length multimers are found of Hpt 2a-β, flanked by Hpt 1a-β in the 2-1 phenotype or as a ring structure in the 2-2. As expected, the patients of a 2-2 phenotype (Hpt 1a-negative) indeed proved to be missing the Hpt 1a peak in their serum protein profile (data not shown).
N-terminal sequences of SAA-1 and SAA-2 from 2-D electrophoresis as determined by in-gel tryptic digestion and measurement by MALDI Re-TOF MS. All fragments terminated at Arginine 15, the expected tryptic cleavage site. Of note are the two peptides spanning positions 3–15 (spots 1 and 3) and 5–15 (spots 1, 2 and 3), which correspond to uncommon N-terminal post-translationally modified variants of SAA-1 visualized simultaneously by SELDI (Figure 3). Expected masses are given of the full-length protein variant.
Detection of a des-1Arg/des-2Ser Variant of SAA-1 by SELDI in seven Patients
It is apparent that the peaks between 11.4 and 11.7 kDa are clustered and are detected only as a triplicate. This is in part confirmed with the detection of multiple peaks within this mass range by immunoaffinity capture of SAA from albumin-depleted serum on a Protein G Array, although the peak at 11.4 kDa was not clearly resolved (Figure 3d, upper panel). SAA was barely detectable within normal serum by the same procedure, as seen in the lower panel of Figure 3d. From the WCX2 data, it is postulated that the peaks at 11 518 and 11 432 Da in Figure 3b are derivatives from the original SAA-1 protein as the mass differences correspond very closely to SAA-1 minus its amino-terminal R (Arginine, 156 Da) and SAA-1 minus the amino-terminal R and S (Serine, 87 Da) (SAA-1-R and SAA-1-RS, respectively). Furthermore, this is confirmed by the detection and subsequent sequencing of a peptide from the in-gel tryptic digest at m/z 1463.61, corresponding to positions 3–15 of SAA-1 (Figure 3c).
SAA could be resolved into three separate spots by 2-D electrophoresis (data not shown), two of which focused between pI 5 and 6 in the first dimension and were identified to contain SAA-1. The third occurred at approximately pI 8 and was identified as SAA-2, a member of the SAA family sharing over 90% homology to SAA-1. The more acidic SAA-1 spot (spot 1, Figure 5), as well as the SAA-2 spot (spot 3, Figure 5), contained a mixture of the des-R and des-RS variants due to the presence of both peptides at m/z 1463.61 (positions 3–15) and m/z 1550.64 (positions 2–15), and were confirmed by PSD sequencing (data not shown). The second SAA-1 spot contained no peptide at m/z 1463.61 after tryptic digestion and its resolution at a pI slightly higher than that of the des-RS isoform suggests it contains full-length SAA-1. SAA-2 could not be resolved by SELDI. Also detected by tryptic digest of all three spots was a nontryptic peptide at m/z 1169.49 corresponding to positions 5–15 of SAA-1 (expected m/z 1169.56) and SAA-2 (data not shown). This peptide is indicative of a 99 amino-acid variant of SAA-1, with an expected average mass of 11 145.08. Indeed, a low-abundant peak is detected at m/z 11 144 Da in the SELDI profile of patient R9 (Figure 2; SAA-1-RSFF). A summary of the N-terminal peptides achieved after tryptic digestion of the SAA-containing spots is given in Figure 5.
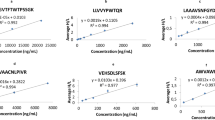
Concentration of SAA in Serum to Determine the Detection Sensitivity of SELDI and Correlation of SAA and 10.84 kDa Marker with Patient Status
Peak intensity on the SELDI protein profile can be correlated with relative abundance of a protein of interest within a sample. It would therefore be of interest to correlate the relative abundance of such proteins with absolute concentrations determined by routine methods to compare the sensitivity of detection. A signal intensity-related value was assigned to both SAA-1 and the 10.84 kDa marker on a diminishing scale, from highly abundant (+++) to undetectable (−) (Table 2). SAA was measured by a sandwich-formatted ELISA in both patient and normal sera. The results are summarized in Figure 6.
Quantitation of SAA in RCC patient and normal sera: SAA concentration was measured by sandwich format ELISA, detecting 14 patients to be raised while all control sera were determined to be below the normal limit of ∼10 μg/ml (dotted line), five examples of which are included (N1, N5, N13, N17, N24). Patients R3, R4, R6 and R9 all possessed concentrations in excess of 200 μg/ml, the limit detectable by the assay. The detection limit by SELDI is in the region of 25–35 μg/ml as shown by the range bar, nominally estimated at 30 μg/ml.
All normal samples revealed an SAA concentration of less than 6.25 μg/ml by ELISA, while the greatest value measured in the patient samples was in excess of 200 μg/ml (greater than the detection range). The four patient samples scored +++ from the SELDI data were also the only ones found to be in excess of 200 μg/ml by ELISA; although the ELISA revealed 14 of 25 patients to be elevated, in contrast to eight by SELDI. Relative abundance according to peak intensity was achieved. Patient R14, scoring++by SELDI and 82.6 μg/ml by ELISA, as well as R16, R19 and R22, which were scored+and measured between 24 and 39 μg/ml by ELISA. The approximate limit of detection of SAA-1 by SELDI is estimated to be 30 μg/ml (Figure 6, dashed line).
The potential 10.84 kDa marker protein was detected in 16 of 25 patients, but in only six of 26 normal controls and in low abundance. Of the 16 patients, four could be scored++and higher (R9, R14, R26, R27), with R9 scoring +++. In addition, R9 was also scored+++and R14++for SAA-1. Of the remaining 12 patients, two also scored+++for SAA-1 by SELDI (R4, R6) and three were awarded+for each marker (R16, R19, R22). Only in one patient (R3) could SAA-1 be detected without the 10.84 marker. All patients that scored highly for SAA-1, the 10.8 kDa marker or both also possessed tumors of a minimum T2.G2 after histology (except R14 who presented with T3b.G1). In particular, patient R9, who scored+++for each, presented with a T2.G3 tumor and two metastatic lesions.
Discussion
In this study, we applied the mass-spectrometric proteomic technique SELDI to the analysis of serum from patients with RCC for the discovery of disease-related proteins by contrast with healthy, age- and sex-matched control samples. In addition, the sensitivity of detection of such proteins was correlated with standard quantitative immunoassays. We were able to detect and subsequently identify Hpt 1a, SAA-1 and variants thereof as being elevated in patients, as well as a third ‘marker’ of disease, yet to be identified, at approximately 10.84 kDa. Protein profiles were reproducible according to mass accuracy, standard-occurring masses and peak intensity. The technique facilitated not only chromatographic retention of proteins to the array, but could be utilized for the capture of specific proteins by the immobilization of a desired antibody to a Protein G ProteinChip Array — also to differentiate patient serum from normal, demonstrated here with the capture of SAA. Accurate mass determination adds a new dimension to the study of specific proteins within a sample and in this case has revealed information about the SAA-1 protein (104 amino acids, average molecular mass 11 682 Da) and variants within the serum of RCC patients. A 102 amino-acid variant of SAA-1, SAA-1 des-1Arg/des-2Ser (SAA-1 des-RS) was present in almost all patients with elevated SAA levels detected by SELDI in addition to SAA-1 des-R.
SAA-1, a member of the SAA gene family including SAA-2 and the constitutive SAA-4 (C-SAA), has been described as an acute-phase protein that is produced in the liver in response to inflammatory stimuli. Circulatory levels can increase as much as 1000-fold during inflammation or infection and is found in association with high-density lipoproteins (HDL) as an apolipoprotein and has been reviewed by Urieli-Shoval et al.14 Raised SAA in serum of cancer patients has been described in different tumors, O’Hanlon et al15 noting a correlation between the highest levels of SAA, as well as C-RP, and ulcerating T4 tumors in breast carcinoma. A study by Glojnaric et al16 even concluded SAA to be a reliable parameter for clinical routine as a nonspecific tumor marker for colorectal carcinoma from a statistical study of patient serum from preoperative through postoperative clinical course, also with reference to normal controls. The mode by which SAA is stimulated in cancer patients is not entirely clear: Interleukin-6 (IL-6) holds an important role in the regulation of acute-phase proteins during an acute-phase response (including SAA, haptoglobin and C-RP), but Bíró et al17 observed no correlation for IL-6 with SAA in multiple myeloma patients. It did, however, correlate positively with C-RP. Blay et al18 reported raised C-RP and haptoglobin in correlation to raised IL-6 in metastatic RCC patients, which were later reduced following a course of anti-IL-6 antibody treatment in a cohort of the same patients. This would suggest an alternate mode of regulation of SAA production within tumor patients. Indeed, a study into the regulation of SAA production in a human hepatoma cell line by Raynes et al19 showed it to be primarily stimulated by IL-1 as opposed to IL-6, increasing synthesis by a factor in excess of 100-fold.
The detection of a des-R variant of SAA-1 and SAA-2 has been widely reported in serum,20, 21, 22 but the description of a des-RS variant has been infrequent and not thoroughly investigated for its distribution and frequency. Baba et al23 and Strachan et al24 reported its detection, but were working from pooled acute-phase serum so would not have had the opportunity to study its frequency. Very recently, Kiernan et al25 reported the application of a mass spectrometric immunoassay (MSIA) for the detection of truncated variants of SAA-1 and SAA-2 in serum, also detecting des-R and des-RS variants (the latter in low abundance in all samples). Interestingly, although only from a comparison of two inflammatory sera with four controls, they describe a differential distribution of the variants between the chronic and acute inflammatory samples with a greater abundance of the des-R form in the chronic. The des-RSFF variant was not detected. The infrequency of the des-RS description and our clear detection within the sera of seven of eight patients with RCC with raised serum SAA levels raises the question of it being a disease-specific variant. Post-translational modification is more than likely the mode by which the N-terminal arginine is removed as opposed to genetic polymorphism,20 and is supported by our observation of the des-R and des-RS variants occurring within both SAA-1 and SAA-2. This is supported by the observation by Raynes et al19 that levels of SAA des-R reach a maximum up to 24 h later than the full-length protein. Extrahepatic expression of SAA has been shown to be widespread, including kidney epithelia26 and more relevantly in RCC tissue by transcription profiling;27 therefore, the detection of SAA des-RS cannot be discounted as cancer-specific and an investigation to resolve this question is underway, incorporating sera from different noncancer inflammatory conditions as well as tumors.
In addition to the detection of SAA-1 and the des-R and des-RS variants, a fourth was identified and could be visualized in low abundance by SELDI. The peak at molecular m/z 11 144.0 Da correlates with SAA-1 minus positions 1–4 (RSFF; F—Phenylalanine, 147.177 Da) and is confirmed by the presence of a tryptic peptide at m/z 1169.46 Da (positions 5–15, expected m/z 1169.585 Da) in digested gel spots (data not shown). This variant has been previously described by Ducret et al,28 who also observed the modification in SAA-1 and -2 in tryptic digests of SAA extracted from sera of rheumatoid arthritis (RA) patients. Interestingly, no SAA des-RS could be detected—although des-R was, as is frequently observed in studies of SAA. In addition, we observed no intact N-terminal SAA-2 in contrast to SAA-1.
The occurrence of modifications at the N terminus of SAA could potentially have an impact upon its function: the N terminus contains the HDL- binding region.22, 29 Moreover, des-R variants of SAA showed a differential susceptibility to matrix metalloproteinase (MMP) digestion than to that of intact SAA; MMPs suggested as being contributory factors to amyloid deposit formation in reactive amyloidosis.30
Haptoglobin, as with SAA, is an acute-phase protein produced by the liver. Its functions are well characterized and are reviewed by Wassell.31 It has long been known to be elevated in the serum of tumor patients and correlates positively within RCC patients to IL-6 concentration, as mentioned earlier. Recently, using the SELDI technique, the 9.2 kDa α chain of haptoglobin was shown to be elevated in the plasma of ovarian cancer and has been used in combination with other Biomarkers for differentiating ovarian cancer samples from controls.32 However, although readily detected by SELDI, Hpt 1a cannot be considered as a specific disease marker using SELDI due to its phenotypic distribution as well as the lack of Hpt 2a detection, but remains an example of the power of the technique to visualize differential proteins present in disease-group sera.
The identification of the protein at 10.84 kDa is unknown. It remains a candidate marker for poor prognosis as detected by SELDI, occurring in 16 patients in total and in four of six metastatic patients. The peak could only be detected in low amounts in six normal samples (data not shown). However, it should be noted that of the patients to possess large signals for the peak (++minimum), two also scored at least++for SAA detection (R9, R14). In addition, patient 26 scored ++ for the marker and was proven to be elevated for SAA by ELISA although not detected by SELDI. Finally, when considering that all patients with ++or+++for the 10.84 kDa marker presented a minimum T2.G2 tumor (except R14 with T3.G1), its relevance as a potential marker of disease status can be alluded to. Efforts are currently underway to identify the protein and to study its distribution among patients and controls.
Although SELDI is not directly quantitative, it could detect changes in the relative abundance of given proteins in a sensitive manner that compares favorably to immunoquantitative methods, such as ELISA. Although more sensitive in their antigenic detection, such methods are indiscriminant of the distribution of isotypes, polymorphs or even abnormal modifications of the target antigen, whereas SELDI adds a new dimension for structural information. It is interesting to note that while a concentration of 24.1 μg/ml of SAA could be detected by SELDI in patient R19, 34.2 μg/ml could not be in R26. The absence of SAA1 but the presence of elevated SAA2 would still show an elevated result by ELISA, as it detects both species simultaneously. The detection limit of SAA, approximately 30 μg/ml, was sufficiently low to distinguish the chronically elevated patients from the normal, although the sample group is too small to draw any firm conclusions about its significance prognostically. A wider study incorporating higher patient numbers will analyze the significance of the SAA variants in conjunction with the 10.84 kDa marker.
To summarize, the SELDI technique affords a rapid and mass-accurate mode of analysis for the detection of multiple disease-related proteins simultaneously, reproducibly and in high throughput. The detection of multiple variants of SAA provides an example of novel information obtained regarding the frequency and distribution of a given protein within a disease model and SELDI will become an invaluable tool for the analysis of proteins within complex protein mixtures, particularly serum.
References
Hutchens TW, Yip TT . New desorption strategies for the mass spectrometric analysis of macromolecules. Rapid Commun Mass Spectrom 1993;7:576–580.
Wright Jr GL . SELDI Proteinchip MS: a platform for biomarker discovery and cancer diagnosis. Expert Rev Mol Diagn 2002;2:549–563.
Rosty C, Christa L, Kuzdzal S, et al. Identification of hepatocarcinoma–intestine–pancreas/pancreatitis-associated protein I as a biomarker for pancreatic ductal adenocarcinoma by protein biochip technology. Cancer Res 2002;62:1868–1875.
Xiao Z, Adam BL, Cazares LH, et al. Quantitation of serum prostatespecific membrane antigen by a novel protein biochip immunoassay discriminates benign from malignant prostate disease. Cancer Res 2001;61:6029–6033.
Li J, Zhang Z, Rosenweig J, et al. Proteomics and bioinformatics approaches for identification of serum biomarkers to detect breast cancer. Clin Chem 2002;48:1296–1304.
Petricoin EF, Ardekani AM, Hitt BA, et al. Use of proteomic patterns in serum to identify ovarian cancer. Lancet 2002;359:572–577.
Adam BL, Qu Y, Davis JW, et al. Serum protein fingerprinting coupled with a pattern-matching algorithm distinguishes prostate cancer from benign prostate hyperplasia and healthy men. Cancer Res 2002;62:3609–3614.
Aebersold R, Mann M . Mass spectrometry-based proteomics. Nature 2003;422:198–207.
Srinivas PR, Srivastava S, Hanash S, et al. Proteomics in early detection of cancer. Clin Chem 2001;47:1901–1911.
Kirkali Z, Tuzel E, Mungan MU . Recent advances in kidney cancer and metastatic disease. BJU Int 2001;88:818–824.
Godley PA, Ataga KI . Renal cell carcinoma. Curr Opin Oncol 2000;12:260–264.
Russo P . Renal cell carcinoma: presentation, staging, and surgical treatment. Semin Oncol 2000;27:160–176.
Poon TC, Johnson PJ . Proteome analysis and its impact on the discovery of serological tumor markers. Clin Chim Acta 2001;313:231–239.
Urieli-Shoval S, Linke RP, Matzner Y . Expression and function of serum amyloid A, a major acute-phase protein, in normal and disease states. Curr Opin Hematol 2000;7:64–69.
O’Hanlon DM, Lynch J, Cormican M, et al. The acute phase response in breast carcinoma. Anticancer Res 2002;22:1289–1293.
Glojnaric I, Casl MT, Simic D, et al. Serum amyloid A protein (SAA) in colorectal carcinoma. Clin Chem Lab 2001;39:129–133.
Bíró L, Domján Gy, Falus A, et al. Cytokine regulation of the acute-phase protein levels in multiple myeloma. Eur J Clin Invest 1998;28:679–686.
Blay J-Y, Rossi J-F, Wijdenes J, et al. Role of interleukin-6 in the paraneoplastic inflammatory syndrome associated with renal cell carcinoma. Int J Cancer 1997;72:424–430.
Raynes JG, Eagling S, McAdam KP . Acute-phase protein synthesis in human hepatoma cells: differential regulation of serum amyloid A (SAA) and haptoglobin by interleukin-1 and interleukin-6. Clin Exp Immunol 1991;83:488–491.
Kluve-Beckerman B, Dwulet FE, Benson MD . Human serum amyloid A: three hepatic mRNAs and the corresponding proteins in one person. J Clin Invest 1988;82:1670–1675.
Raynes JG, McAdam KP . Serum amyloid A isoforms in inflammation. Scand J Immunol 1991;33:657–666.
Patel H, Bramall J, Waters H, et al. Expression of recombinant human serum amyloid A in mammalian cells and demonstration of the region necessary for high-density lipoprotein binding and amyloid fibril formation by site-directed mutagenesis. Biochem J 1996;318:1041–1049.
Baba S, Takahashi T, Kasama T, et al. A novel polymorphism of human serum amyloid A protein, SAA1γ, is characterized by alanines at both residues 52 and 57. Arch Biochem Biophys 1993;303:361–366.
Strachan AF, Brandt WF, Woo P, et al. Human serum amyloid A protein: the assignment of six major isoforms to three published gene sequences and evidence for two gene loci. J Biol Chem 1989;264:18368–18373.
Kiernan UA, Tubbs KA, Nedelkov D, et al. Detection of novel truncated forms of human serum amyloid A protein in human plasma. FEBS Lett 2003;537:166–170.
Urieli-Shoval S, Cohen P, Eisenberg S, et al. Widespread expression of serum amyloid A in histologically normal tissues: predominant localization to the epithelium. J Histochem Cytochem 1998;46:1377–1384.
Huber W, Boer JM, von Heydebreck A, et al. Transcription profiling of renal cell carcinoma. Verh Dtsch Ges Pathol 2002;86:153–164.
Ducret A, Foyn Bruun C, Bures EJ, et al. Characterization of human serum amyloid A protein isoforms separated by two-dimensional electrophoresis by liquid chromatography/electrospray ionization tandem mass spectrometry. Electrophoresis 1996;17:866–876.
Turnell W, Sarra R, Glover ID, et al. Secondary structure prediction of human SAA1. Presumptive identification of calcium and lipid binding sites. Mol Biol Med 1986;3:387–407.
Stix B, Kähne T, Sletten K, et al. Proteolysis of AA amyloid fibril proteins by matrix metalloproteinases-1, -2, and -3. Am J Pathol 2001;159:561–570.
Wassell J . Haptoglobin: function and polymorphism. Clin Lab 2000;46:547–552.
Rai AJ, Zhang Z, Rosenzweig BS, et al. Proteomic approaches to tumor marker discovery. Arch Pathol Lab Med 2002;126:1518–1526.
Acknowledgements
We thank Dr Christoph Weinstock and Joerg Hennenlotter for their roles in the organization of control and patient sera, respectively. This project was supported by the Fortuene program, Project No. 829-0-0.
Author information
Authors and Affiliations
Corresponding author
Additional information
Duality of interest is none.
Rights and permissions
About this article
Cite this article
Tolson, J., Bogumil, R., Brunst, E. et al. Serum protein profiling by SELDI mass spectrometry: detection of multiple variants of serum amyloid alpha in renal cancer patients. Lab Invest 84, 845–856 (2004). https://doi.org/10.1038/labinvest.3700097
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700097
Keywords
This article is cited by
-
Fluorescent paper strip immunoassay with carbon nanodots@silica for determination of human serum amyloid A1
Microchimica Acta (2021)
-
Rapid discrimination of multiple myeloma patients by artificial neural networks coupled with mass spectrometry of peripheral blood plasma
Scientific Reports (2019)
-
Serum amyloid A – a review
Molecular Medicine (2018)
-
Haptoglobin-α1, -α2, vitamin D-binding protein and apolipoprotein C-III as predictors of etanercept drug response in rheumatoid arthritis
Arthritis Research & Therapy (2015)
-
Identification of potential serum biomarkers for Wilms tumor after excluding confounding effects of common systemic inflammatory factors
Molecular Biology Reports (2012)