Abstract
The link between mesangial cell (MC) proliferation and migration during glomerular repair in the experimental mesangial proliferative glomerulonephritis suggests that cell cycle regulation and cell migration require similar pathways, such as cell cycle proteins. The immunosuppressant RAD inhibits mesangial cell (MC) proliferation via G1/S arrest. Moreover, RAD dramatically impairs glomerular healing in the anti-Thy1 model. We tested the hypothesis that RAD alters MC migration in vitro and that this effect was mediated by the CDK-inhibitors p21CIP1 and p27KIP1. Using a modified Boyden chamber in vitro migration assay, our results showed that RAD dose dependently (1–50 nM) inhibited fibronectin-induced chemotaxis in wild-type (wt) MC. RAD treatment prevented the decrease in p27KIP1 induced by mitogenic growth factors, but had no effect on p21CIP1 by Western blot analysis. The antimigratory effect of RAD in wt MC was substantially dependent on p27KIP1, but not p21CIP1, since the inhibitory effects of 1–10 nM RAD on MC migration were similar in p21CIP1 deficient and wild-type MC. The effect of RAD on MC migration was also examined in the anti-Thy1 model by BrdU-labeling of proliferating MC on day 3 that typically repopulate the glomerulus from the hilus. A control biopsy on day 3 was taken to define the starting point prior to the initiation of RAD (3 mg/kg or placebo). MC migration was determined on day 7 by measuring the distances of BrdU-labeled MC (OX-7+/BrdU+cells) from the glomerular hilus using computerized morphometry. RAD significantly reduced the migratory response of BrdU-labeled MC compared to controls.
We conclude that the immunosuppressant RAD effectively inhibits MC migration in vivo and in vitro thereby limiting the normal glomerular repair process after severe injury. Moreover, RAD-induced inhibition of MC migration in vitro is partially mediated by the CDK-inhibitor p27KIP1, but not p21CIP1.
Similar content being viewed by others
Main
Severe disruption of the mesangium (mesangiolysis) occurs in many human renal diseases such as IgA nephropathy, hemolytic uremic syndrome, mesangiocapillary glomerulonephritis, allograft rejection, and diabetic nephropathy.1 Incomplete repair of the mesangiolytic injury may be an important determinant of glomerular disease progression. Successful and complete glomerular repair after very severe disruption of the mesangium is demonstrated in experimental mesangial proliferative glomerulonephritis in the rat (anti-Thy1 nephritis),2 which serves as a useful model to study the mechanisms underlying these events. In the anti-Thy1 model, complete restoration of the glomerular architecture after injury is followed by capillary angiogenesis, matrix remodeling, and simultaneous mesangial cell (MC) proliferation and migration.3, 4, 5 While recent studies in the anti-Thy1 model demonstrated that about 11% of the glomerular repopulation after injury is derived from bone marrow, the major part of the glomerular reconstitution originates in the kidney.4, 6 Within 1–2 days, surviving ‘reserve’ cells from the extraglomerular and hilar region reconstitute the major part of the mesangium by a coordinated proliferative and migratory response which is complete by days 7–10.3, 4 Although glomerular cell migration and proliferation can be dissociated in certain experimental nephritis models5 and by blockade of certain cytokines such as FGF-27 both mechanisms are required for glomerular repair/regeneration and timely as well as spatially closely connected in the anti-Thy1 model. This apparent link between cell proliferation and migration suggests that cell cycle regulation and cell migration may be governed by similar pathways, such as cyclins, cyclin-dependent kinases (CDK), and in particular the CDK-inhibitors p21CIP1 and p27KIP1. We have previously shown that p27KIP1 and p21CIP1 expression is altered during glomerular repopulation in the anti-Thy1 model.8
The potent antiproliferative rapamycin derivative RAD is a new promising immunosuppressive drug for the treatment of organ and kidney transplantation, and more recently, has been shown to inhibit proliferation via G1/S arrest in inflammatory renal disease.9 Although RAD and rapamycin are generally considered to lack nephrotoxicity of the calcineurin inhibitors cyclosporine and tacrolimus, we (unpublished results) and others10 have recently demonstrated detrimental long term effects on the glomerular architecture when RAD therapy was given during the early proliferative/migratory phase of anti-Thy1 nephritis. Taken together, we hypothesized that RAD therapy may have a specific antimigratory effect in addition to being antiproliferative, which may contribute to its puzzling detrimental effects.
Accordingly, we designed studies to determine if RAD inhibits MC migration in vitro and in vivo during glomerular repopulation in addition to being antiproliferative, and asked if these effects required the CDK-inhibitors p27KIP1 or p21CIP1. Our results show that the immunosuppressant RAD effectively inhibits MC migration in vivo and in vitro and that this is partially mediated by p27KIP1.
Materials and methods
Cell Culture
Cultured mouse mesangial cells (MMC) were isolated from p21CIP1-, p27KIP1-, and p21CIP1/p27KIP1-null or wild-type (wt) mice as previously described.11, 12 MC were grown in DMEM containing 4.5 g glucose/l−1 and supplemented with 10% fetal calf serum, L-glutamine, insulin, and penicillin/streptavidin.
In Vitro Cell Migration Assay
MC migration was investigated using a 48-well-modified Boyden chamber and 0.1% gelatin-coated polyvinyl–pyrrolidone-free polycarbonate membranes with 8 μm poresize (Neuroprobes, Inc. Gaithersburg, MD, USA). After 16 h preincubation with 0, 1, 10 and 50 nM RAD (provided by Dr Schuler, Novartis Pharma AG Basel) 28 000 mesangial cells/well were loaded into the upper chamber. In two initial experiments, RAD was administered to wt-MMC without preincubation. The bottom wells were filled with 40 μg/ml fibronectin, used as the chemoattractant, or 0.1% BSA, used as a negative control. The Boyden chamber was incubated for 5 h at 37°C and 5% CO2 to allow migration of cells through the membrane. Cells that had transmigrated were stained with Qick diff and three fields of vision per well were analyzed using phase-contrast microscopy at a 250 × magnification. All assays were done in triplicate and each experiment was done a minimum of three times.
Animal Model and Experimental Design
The effect of RAD therapy on MC migration was also examined in the anti-Thy1 model of mesangioproliferative glomerulonephritis. Three days after disease induction proliferating MC repopulating the glomerulus from the hilus region, were labeled with i.p. BrdU-injection in 12 Sprague–Dawley rats. A kidney biopsy was taken simultaneously as previously described4 to define the baseline. Half the nephritic rats (n=6) were given RAD by gavage at a concentration of 3 mg/kg bw and six rats were given placebo (only containing the solvent of RAD). MC migration was measured on day 7 of disease by measuring the distances of BrdU labeled MC (OX-7+/BrdU+ cells) from the glomerular hilus using computerized morphometry,4, 7 and we used the baseline biopsy obtained at day 3 (ie before the initiation of RAD) in these calculations. The exact protocol for our in vivo migration assay has been previously described in detail.3, 4, 7
Experimental mesangial proliferative glomerulonephritis (anti-Thy1 model) was induced by a single injection of the monoclonal anti-Thy1.1 antibody OX-7 (0.35 ml/100 g bw) in male Sprague–Dawley rats13 (Charles River, Sulzfeld, Germany). 54, 62, and 70 h after disease induction, intraperitoneal injections of 10 mg/100 g bw BrdU were given in all rats to label surviving mesangial reserve cells located at the extraglomerular mesangium and hilar region that just start to repopulate the glomerulus via proliferation (DNA synthesizing) and migration. Three injections were given to increase the number of labeled cells. At 2 h after the last BrdU injection (72 h after disease induction), a baseline renal survival biopsy was performed. Immediately after recovery from anesthesia either microemulsion preconcentrate as vehicle or RAD (Novartis Pharma AG, Basel, Switzerland) was given once daily orally by gavage at a dose of 3 mg/kg bw/day. The first two RAD doses were given as loading doses containing two-fold the amount of the later doses. All rats were killed 7 days after disease induction and renal tissues harvested.
To assess the effect of RAD therapy on the CDK inhibitor p27KIP1 and total or phosphorylated p70S6 kinase during glomerular repopulation, anti-Thy1 disease was induced in a second set of 12 rats, and RAD or placebo therapy was started on day 3. Afterwards, a survival biopsy was done on day 4 and all rats were killed on day 7. The percentage of glomerular cells staining positive for total or phosphorylated p70S6 kinase and the CDK inhibitor p27KIP1 was evaluated as previously described.
In an additional third experiment, three nephritic rats each were given RAD or placebo as described in the second experiment, and protein from isolated glomeruli was extracted on day 4 for determination of the CDK-inhibitor p27KIP1 and total and phosphorylated p70S6 kinase by Western blot analysis (see below).
Immunohistochemistry
Tissue for light microscopy was fixed in methyl Carnoy's solution, embedded in paraffine, and cut into 5 μm sections for indirect immunoperoxidase staining as described elsewhere.4, 13
MC were identified using an antibody against OX-7 (Serotec, Ltd., Kidlington, Oxford, UK).4 The following additional antibodies were used in this study: Peroxidase-labeled Fab-fragments against BrdU (Boehringer, Mannheim, Germany); polyclonal rabbit anti-p21CIP1and anti-p27KIP1 antibodies (Santa Cruz Biotechnology, Heidelberg, Germany);8 mouse monoclonal antibody against the total p70S6 kinase as well as the phosphorylated p-p70S6 kinase (Santa Cruz).14 Negative controls for immunostaining included either deleting the primary antibody or substitution of the primary antibody with equivalent concentrations of an irrelevant murine mAb or preimmune rabbit IgG.
Immunohistochemical Double Staining
To determine the migratory response of the labeled, BrdU-positive MC during glomerular repopulation, double immunostaining for BrdU and OX-7, an MC-specific marker for MC was performed as previously described.4
The first primary antibody (OX-7) was incubated overnight at 4°C, followed sequentially by biotinylated rabbit anti-mouse IgG1 serum (Zymed, San Francisco, CA, USA), peroxidase conjugated Avidin D (Vector, Burlingame, CA, USA), color development with DAB without Nickel Chloride. Incubation in 3% H2O2/methanol for 20 min prevented any remaining peroxidase activity. Subsequently, the second primary antibody (Peroxidase labeled anti-BrdU Fab-fragments, Boehringer, Mannheim, Germany) was applied overnight at 4°C, followed by DAB with nickel as the second color reagent. Controls included omitting either the primary antibodies or replacing them by mouse serum, as well as omitting either the secondary antibodies.
Morphometric Analysis of MC Migration
Migration of labeled MC was quantitated using a computerized morphometry system (Visitron Systems GmbH, Puchheim, Germany). The shortest distance from the border between extra- and intraglomerular mesangium (OX-7 staining) to any labeled OX-7 positive MC was measured. For each biopsy, more than 10 cross sections with an identifiable extraglomerular mesangium out of more than 100 cortical glomeruli were examined.
Western Blot Analysis
Protein was extracted either from isolated rat glomeruli by our standard sieving technique15 or from MMC cultures using 50 mM Tris, 1% (v/v) Nonidet P-40, 0.25 (w/v) sodium deoxycholate, 150 mM NaCl, 1 mM EGTA, 1 mM Na3VO4, 1 mM NaF, and proteinase inhibitor cocktail (Complete, Boehringer, Mannheim, Germany) as extraction buffer. To optimize solubilization, extracts were sonified for 30 s at 50% power and 50% duty cycle using a Sonoplus HD70 (Bandelin, Berlin, Germany). A measure of 30 μg of protein was resolved in sodium dodecyl sulfate-polyacrylamide gel electrophoresis, and proteins were transferred semidry to a nitrocellulose membrane for detection of p21CIP1, p27KIP1, P70S6 kinase or phosphorylated P70S6 kinase protein by using specific antibodies (Santa Cruz). β-actin was detected simultaneously as loading control using an antibody from Abcam, Cambridge, UK. For evaluation of densitometry AIDA 2.1 software (Raytest Isotopenmeßgeräte GmbH, Straubenhard, Germany) was used.
Statistical Analysis
All values are expressed as mean s.d. Statistical significance (defined as a P of less than 0.05) was evaluated using the Student's t-test or one-way analysis of variance with modified t-test using the Bonferroni method.
Results
In Vitro Studies
RAD inhibits MC migration in vitro
We used a 48-well modified Boyden chamber in vitro migration assay to determine the effects of RAD on migration. Pretreatment with RAD for 16 h inhibited fibronectin-induced chemotaxis in a dose-dependent matter in wt mouse MC (wt-MMC). Our results showed that RAD reduced wt-MMC migration by 20% at 1 nM, 50% at 10 nM, and 75% at 50 nM concentration, respectively, compared to placebo (P<0.05) (Figure 1). Similar results were obtained in a minimum of three experiments. Significant inhibition of wt-MMC migration was also seen when no RAD pretreatment occurred and RAD was given only in the Boyden chamber during the migration time of 5 h (30% at 50 nM). Nevertheless, since RAD induced inhibition of cell migration was much stronger after preincubation of MMC for 16 h, all following experiments were done with RAD pretreatment.
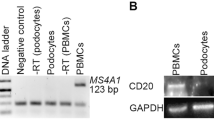
RAD regulates p27KIP1, but not p21CIP1 protein in MC in vitro
We next determined, if RAD alters the levels of specific CDK-inhibitors. Exposing MMC to RAD differentially affected the protein levels of the CDK-inhibitors p21CIP1 and p27KIP1 measured by Western blot analysis in wt-MMC. As we showed previously, p27KIP1 was very abundant in growth-arrested wt-MMC. In contrast, p27 levels were reduced following stimulation with 10% FCS, a source of growth factors (Figure 2). Our results showed that 10 and 20 nM of RAD significantly prevented the decrease in p27KIP1 induced by growth factor stimulation (10% FCS) (Figure 2). RAD at a 100 nM concentration was less effective in preventing the FCS-induced decrease of p27KIP1 (Figure 2). In contrast to p27KIP1, protein levels of p21CIP1 were not altered by FCS or RAD treatment (Figure 2). Taken together, these results show that RAD has a differential effect on CDK-inhibitor expression.
RAD regulates p27KIP1, but not p21CIP1 protein in MC in vitro. Regulation of the CDK-inhibitors p21CIP1 and p27KIP1 by RAD treatment was investigated in growth arrested (0.5% FCS) or growth factor stimulated (20% FCS) wt MMC using Western blot analysis. While p27KIP1 was highly expressed in growth-arrested wt-MMC, it was completely suppressed after stimulation with 20% FCS (Figure 2). RAD at a 10 and 20 nM, but hardly at a 100 nM concentration markedly prevented the p27KIP1 suppression by 20% FCS. In contrast, protein levels of p21CIP1 appeared to be independent on FCS or RAD treatment.
RAD-induced inhibition of MC migration is p27KIP1, but not p21CIP1 dependent
The role of p21CIP1 and p27KIP1, alone and together, in RAD-induced inhibition of MC migration was assessed utilizing p21CIP1-null, p27KIP1-null, and p21CIP1/p27KIP1 double-null MMC. The inhibitory effects of 1–10 nM RAD on MC migration were similar in p21CIP1-null and wt-MMC (Figure 3a). However, at a 50 nM RAD concentration, the migratory response was significantly less inhibited in p21CIP1-null compared to wt-MMC (P<0.005) (Figure 3a). In contrast, the antimigratory effect of RAD in wt-MMC was substantially more dependent on p27KIP1 than on p21CIP1 as investigated via MMC from p27KIP1- and p21CIP1/p27KIP1-double-null mice. In p27KIP1-null MMC, 1 nM RAD had no effect and 10 and 50 nM RAD reduced the number of migrating MMC only by 12 and 30%, respectively, compared to inhibition of 47 and 72% in wt-MMC with similar concentrations (P<0.001) (Figure 3a). In contrast, p21CIP1-null MMC exhibited a 40% (not significant compared to wt-MMC) and 46% (P<0.005 compared to wt-MMC) decrease in the number of migrating cells when exposed to 10 and 50 nM RAD, respectively (Figure 3a). In addition, when p21CIP1/p27KIP1 double-null MMC were compared to p27KIP1 -null MMC, the migratory response under RAD therapy was similar (P>0.05) (Figure 3b) suggesting that the additional lack of p21CIP1 is not critical for migration of MMC.
RAD-induced inhibition of MC migration is p27KIP1, but not p21CIP1 dependent. RAD-induced inhibition of MC migration was assessed in p21CIP1-and p27KIP1-null MMC by a Boyden chamber assay using fibronectin as the chemoattractants. MMC were pretreated with different concentrations (1, 10, 50 nM) RAD for 19 h. The asterisk (*) indicates significant changes vs wt-MMC (P<0.005). Since the antimigratory effect of RAD in wt-MC was substantially more dependent on p27KIP1 than on p21CIP1, the RAD dependency at different concentrations (1, 10, 50 nM) of the migratory response was also compared in cultured MMC from p27KIP1-null vs p21CIP1/p27KIP1 double-null mice (Figure 4b) and no significant change was found (P>0.05).
In Vivo Studies
RAD therapy inhibited MC migration in vivo
We used the previously established in vivo migration assay to determine the effects of RAD on MC migration in the anti-Thy1 model of experimental mesangial proliferative glomerulonephritis. Figure 5 shows that RAD therapy reduced the migratory response of BrdU labeled MC by 75% compared to placebo-treated rats (P<0.0005) (Figure 4). In placebo-treated nephritic rats, labeled MC typically migrated 42.8±10.4 μm (Figure 4b) from the hilus to the periphery of the glomerulus. In contrast, RAD significantly reduced migration of labeled MC in nephritic rats to 10.2±11.8 μm (Figure 4c) within 4 days (P<0.0005 vs control). Therefore, this progressive migration of MCs towards the glomerular periphery occurs at a rate of 10.7±2.6 μm per day in placebo-treated nephritic rats and only of 2.7±3.0 μm per day during RAD treatment (P<0.05) (Figure 4d). Taken together, these results show that RAD treatment markedly inhibits MC migration in the anti-Thy 1 model in vivo.
RAD therapy did not alter p27KIP1 protein, but phosphorylation of the p70S6 kinase in vivo (immunostaining). The glomerular percentage of nuclei that stained positive for p27KIP1 in RAD or placebo-treated anti-Thy1 rats was assessed on days 4 and 7 (a). The expression and phosphorylation of the p70S6 kinase, a well-known RAD/rapamycin target protein, was further investigated in the same tissues. The glomerular percentage of positive cells for the phosphorylated (b) and total (c) form of the p70S6 kinase was evaluated. The asterisk (*) indicates significant changes vs placebo-treated rats (P<0.05).
RAD therapy inhibited MC migration in the anti-Thy1 model in vivo. Using the in vivo migration system as described in Materials and methods, the distance of BrdU labeled MC from the hilus to the periphery of the glomerulus on day 7 of anti-Thy1 disease was compared to their distance at the starting point on day 3. Double staining for OX-7 (marker for MC, brown) and BrdU (black) demonstrates the labeling of DNA synthesizing MC at the starting point of this assay (on day 3) close to the hilus (a). As shown before, many BrdU-labeled MC could be detected out in the glomerular periphery in placebo-treated anti-Thy1 diseased animals on day 7 (b). In RAD-treated anti-Thy1 rats, labeled MC stayed much closer to the hilar region indicating a defect in the migratory response (c). Quantitation of this assay by computerized morphometry demonstrates that on average, labeled MC in placebo treated rats migrated 42.8±10.4 μm (d), while labeled MC in RAD-treated diseased rats only traveled 10.2±11.8 μm (d) within 4 days. The asterisk (*) indicates significant changes vs placebo-treated rats (P<0.05).
In anti-Thy1 nephritis, RAD therapy did not induce p27KIP1 protein expression, but prevented phosphorylation of the p70S6 kinase
Since RAD prevented MC migration in vitro via p27KIP1, we examined, whether RAD treatment would also upregulate p27KIP1 in anti-Thy1 nephritis. To investigate the regulation of the CDK inhibitor p27KIP1 by RAD therapy in the anti-Thy1 model in vivo, total glomerular cell number and the number of nuclei per glomerulus that stained positive for p27KIP1 was assessed in a blinded manner. The percentage of p27KIP1-positive cells per total glomerular cell number was calculated in placebo- and RAD-treated nephritic rats. Despite regulation of p27KIP1 by RAD in MC in culture, Figure 6a shows that RAD therapy did not change the percentage of p27KIP1-positive glomerular cells (Figure 5a) on day 4 or 7 in anti-Thy1 nephritis in vivo. This result was confirmed by Western blot analysis for p27KIP1 using glomerular extracts from anti-Thy1 diseased rats on day 4 with/without RAD treatment (Figure 6).
RAD therapy did not alter p27KIP1 protein, but phosphorylation of the p70S6 kinase in vivo (Western blot analysis). Independently, glomerular extracts anti-Thy1 diseased rats on day 4 with/without RAD treatment starting on day 3 were evaluated regarding p27KIP1 and the expression and phosphorylation of the p70S6 kinase by Western blot analysis. The asterisk (*) indicates significant changes vs placebo-treated rats (P<0.05).
To demonstrate that RAD was nevertheless acting via its usual known signal transduction molecules in vivo in our model, the expression and phosphorylation of the p70S6 kinase were investigated by immunostaining and Western blot analysis. In anti-Thy1 nephritis, RAD therapy selectively reduced the percentage of positive cells for the phosphorylated form of p70S6 kinase per total glomerular cell number (Figure 5b), but did not affect the percentage of glomerular p70S6 kinase-positive cells (Figure 5c). This result was also confirmed, when expression and phosphorylation of p70S6 kinase were examined on day 4 using Western blot analysis (Figure 6).
Discussion
The antiproliferative and immunosuppressive RAD used in kidney transplantation, inflammatory renal disease, and vasculitis9 has recently been studied in experimental mesangial proliferative glomerulonephritis (anti-Thy1 model). 10 However, despite being antiproliferative, which one would expect to be beneficial as it is with other antiproliferative agents,15, 16, 17, 18 RAD prevents glomerular repair in anti-Thy1 nephritis, leading to worsening renal function.
Repair of mesangiolysis requires both MC migration and proliferation.3, 4 The novel results of the current study demonstrate that just in addition to inhibiting proliferation of MC in vitro and in vivo,10, 19 RAD also dramatically prevents the migratory response of MC in vitro and in vivo. Previous studies have shown that following MC injury in the anti-Thy1 model, the surviving ‘reserve MC’ in the extraglomerular mesangium and hilar region are attracted to migrate to the periphery of the glomerulus in a coordinated way to repopulate the glomeruli.3, 4 Therefore, by inhibiting this repairative response to injury, RAD prevents the healing phase of mesangiolysis. A similar effect has been observed, when conventional16 and nonanticoagulant20 heparin treatment was applied in the anti-Thy1 model in vivo. While no in vivo data regarding MC migration are available, the antiproliferative agent heparin also induces inhibition of MC migration in vitro.21 In contrast to the adverse RAD effects seen in the anti-Thy1 model, the transient prolongation of the mesangiolytic phase during heparin treatment did completely resolve within 40 days and even led to long-term beneficial consequences regarding renal functional and structural parameters after 120 days.16, 20 It also has to be considered that the degree of cellular effects regarding proliferation/migration may be very different with RAD vs heparin treatment.
If migration and proliferation of the repopulating MC is markedly prevented, the mesangium is limited to the perihilar area of the glomerular tuft and an important counterpart for stabilizing the forces of the glomerular tuft22 in the periphery may be completely missing. This suggests that the early postmesangiolytic phase is vulnerable, for the later outcome critical phase, where the decision between a successful glomerular healing reaction or a chronic progressive time course is made.
Previous studies in experimental mesangioproliferative glomerulonephritis models have demonstrated that MC proliferation and migration can be dissociated.5, 7 Blocking of FGF-2 in the anti-Thy1 model resulted in inhibition of mesangial cell proliferation without significant effects on cell migration.7 In the Habu snake venom glomerulonephritis model, MC migrated during the first 24 h after disease induction without significant proliferation.5 Therefore, inhibition of cell proliferation is not linked with simultaneous inhibition of migration in a general fashion.7 Nevertheless, many growth factors have the potential to act as both mitogens and chemoattractants.23 The apparent link of cellular proliferation and migration during glomerular repopulation in the anti-Thy1 model suggests that cell cycle regulation and cell migration may be regulated by similar pathways. In this study, we focused on the CDK-inhibitors p21CIP1 and p27KIP1, because these have been previously shown to be regulated during glomerular repopulation.8, 24 Utilizing cultured MC from wt, p21CIP1-null, p27KIP1-null, and p21CIP1/p27KIP1-double-null mice, we demonstrated that the CDK-inhibitor p27KIP1, but not p21CIP1 plays a critical role in mediating the antimigratory properties of RAD in vitro. The lack of p27KIP1 in MMC prevented the antimigratory effect of RAD up to a concentration of 10 nM, while higher RAD concentrations were able to inhibit MMC migration in Boyden chamber assays, but to a much lesser extent than in wt-MMC. These data are consistent with previous reports regarding vascular smooth muscle cell migration25, 26 and suggest that at higher doses, p27KIP1-independent actions of RAD can inhibit MC migration.
The role and RAD-dependent regulation of p27KIP1 in MC migration may be clinically relevant, since p27KIP1 is tightly regulated in glomerular disease. Therefore, we further investigated, whether p27KIP1 levels are changed during RAD therapy in anti-Thy1 nephritis in vivo. Neither by determination of the percentage of p27KIP1-positive cells per glomerular cross section nor by Western blot analysis of glomerular extracts, any RAD-dependent regulation of p27KIP1 was found in anti-Thy1 nephritis, despite a marked effect on MC migration and on the phosphorylation of the p70S6 kinase as another RAD signaling target. Nevertheless, this lack of p27KIP1 regulation in glomeruli from anti-Thy1 nephritic rats does not completely rule out a role for p27KIP1 in MC migration nor in RAD-induced prevention of MC migration. For the interpretation of the unchanged p27KIP1 in vivo, it has to be considered that our ‘glomerular’ data reflect regulation of p27KIP1 in all different cell populations (inflammatory cells, endothelial cells, podocytes and MC), while only regulation for the repopulating mesangial fraction of glomerular cells is relevant. Alternatively, it is interesting that in cultured wt-MMC, higher RAD doses (50–100 nM) were much less potent to prevent growth factor stimulated suppression of p27KIP1 compared to lower doses around 10–20 nM (Figure 2) and its effects on MC migration became partially p27KIP1 independent. This phenomenon in MC has also been found in vascular smooth muscle cells.26 Although in vivo and in vitro doses are difficult to compare, the in vivo dose of 3 mg/kg bw (and loading doses) RAD is certainly considered to be high. Nevertheless, in this specific in vivo experiment, p70S6k phosphorylation, but not expression as a classical RAD-signal transduction target was inhibited suggesting p27KIP1-independent pathways in this model.
In conclusion, our results demonstrate that the immunosuppressant RAD dramatically inhibits MC migration in vitro and in vivo, which may be highly relevant for the inhibition of the glomerular healing process after severe mesangiolysis. Our in vitro results demonstrate that RAD-induced inhibition of MC migration is partially mediated by the CDK-inhibitor p27KIP1, but not p21CIP1. Further specific blocking and overexpressing studies have to still define the role for p27KIP1 in MC migration and in RAD-induced prevention of MC migration.
References
Morita T, Yamamoto T, Churg J . Mesangiolysis: an update. Am J Kidney Dis 1998;31:559–573.
Johnson RJ . The glomerular response to injury: progression or resolution? Kidney Int 1994;45:1769–1782.
Hugo C, Pichler R, Gordon K, et al. The cytoskeletal linking proteins, moesin and radixin, are upregulated by platelet-derived growth factor, but not basic fibroblast growth factor in experimental mesangial proliferative glomerulonephritis. J Clin Invest 1996;97:2499–2508.
Hugo C, Shankland SJ, Bowen-Pope DF, et al. Extraglomerular origin of the mesangial cell after injury. A new role of the juxtaglomerular apparatus. J Clin Invest 1997;100:786–794.
Barnes JL, Hevey KA, Hastings RR, et al. Mesangial cell migration precedes proliferation in Habu snake venom-induced glomerular injury. Lab Invest 1994;70:460–467.
Ito T, Suzuki A, Imai E, et al. Bone marrow is a reservoir of repopulating mesangial cells during glomerular remodeling. J Am Soc Nephrol 2001;12:2625–2635.
Haseley LA, Hugo C, Reidy MA, et al. Dissociation of mesangial cell migration and proliferation in experimental glomerulonephritis. Kidney Int 1999;56:964–972.
Shankland SJ, Hugo C, Coats SR, et al. Changes in cell-cycle protein expression during experimental mesangial proliferative glomerulonephritis. Kidney Int 1996;50:1230–1239.
Schuler W, Sendrani R, Cottens S, et al. SDZ RAD, a new rapamycin derivative: pharmacological properties in vitro and in vivo. Transplantation 1997;64:36–42.
Daniel C, Ziswiler R, Frey B, et al. Proinflammatory effects in experimental mesangial proliferative glomerulonephritis of the immunosuppressive agent SDZ RAD, a rapamycin derivative. Exp Nephrol 2000;8:52–62.
Monkawa T, Hiromura K, Wolf G, et al. The hypertrophic effect of transforming growth factor-beta is reduced in the absence of cyclin-dependent kinase-inhibitors p21 and p27. J Am Soc Nephrol 2002;13:1172–1178.
Hiromura K, Pippin JW, Fero ML, et al. Modulation of apoptosis by the cyclin-dependent kinase inhibitor p27(Kip1). J Clin Invest 1999;103:597–604.
Rost S, Daniel C, Schulze-Lohoff E, et al. P2 receptor antagonist PPADS inhibits mesangial cell proliferation in experimental mesangial proliferative glomerulonephritis. Kidney Int 2002;62:1659–1671.
Lieberthal W, Fuhro R, Andry CC, et al. Rapamycin impairs recovery from acute renal failure: role of cell-cycle arrest and apoptosis of tubular cells. Am J Physiol Renal Physiol 2001;281:F693–F706.
Johnson RJ, Raines EW, Floege J, et al. Inhibition of mesangial cell proliferation and matrix expansion in glomerulonephritis in the rat by antibody to platelet-derived growth factor. J Exp Med 1992;175:1413–1416.
Floege J, Eng E, Young BA, et al. Heparin suppresses mesangial cell proliferation and matrix expansion in experimental mesangioproliferative glomerulonephritis. Kidney Int 1993;43:369–380.
Floege J, Ostendorf T, Janssen U, et al. Novel approach to specific growth factor inhibition in vivo: antagonism of platelet-derived growth factor in glomerulonephritis by aptamers. Am J Pathol 1999;154:169–179.
Ziswiler R, Steinmann-Niggli K, Kappeler A, et al. Mycophenolic acid: a new approach to the therapy of experimental mesangial proliferative glomerulonephritis. J Am Soc Nephrol 1998;9:2055–2066.
Wang W, Chan YH, Lee W, et al. Effect of rapamycin and FK506 on mesangial cell proliferation. Transplant Proc 2001;33:1036–1037.
Burg M, Ostendorf T, Mooney A, et al. Treatment of experimental mesangioproliferative glomerulonephritis with non-anticoagulant heparin: therapeutic efficacy and safety. Lab Invest 1997;76:505–516.
Person JM, Lovett DH, Raugi GJ . Modulation of mesangial cell migration by extracellular matrix components. Inhibition by heparin like glycosaminoglycans. Am J Pathol 1988;133:609–614.
Kriz W, Elger M, Mundel P, et al. Structure-stabilizing forces in the glomerular tuft. J Am Soc Nephrol 1995;5:1731–1739.
Chicoine MR, Silbergeld DL, et al. Mitogens as motogens. J Neurooncol 1997;35:249–257.
Shankland SJ, Wolf G, et al. Cell cycle regulatory proteins in renal disease: role in hypertrophy, proliferation, and apoptosis. Am J Physiol Renal Physiol 2000;278:F515–F529.
Poon M, Marx SO, Gallo R, et al. Rapamycin inhibits vascular smooth muscle cell migration. J Clin Invest 1996;98:2277–2283.
Sun J, Marx SS, Chen HJ, et al. Role for p27(Kip1) in vascular smooth muscle cell migration. Circulation 2001;103:2967–2972.
Acknowledgements
We would like to acknowledge Novartis Pharma AG Basel for providing RAD solution and RAD vehicle solution. This work was supported by the Deutsche Forschungsgemeinschaft, the SFB 423 ‘Nierenschäden: Pathogenese und regenerative Mechanismen’ (TP B6) and the Interdisciplinary Center of Clinical Research (IZKF)-TP B30. The authors are indebted to Andrea Lüdke, Susanne Weber, Ulrike Goller, and Ossama Mohamed for their excellent technical help during these studies. Portions of this work was presented at the International Society of Nephrology annual meeting, Berlin, June 8–12, 2003 (NDT, 2003, Vol.18, Suppl. 4) and American Society of Nephrology annual meeting, San Diego, October 14–17, 2003 (J Am Soc Nephrol, 2003).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Daniel, C., Pippin, J., Shankland, S. et al. The Rapamycin derivative RAD inhibits mesangial cell migration through the CDK-inhibitor p27KIP1. Lab Invest 84, 588–596 (2004). https://doi.org/10.1038/labinvest.3700078
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700078
Keywords
This article is cited by
-
Stathmin mediates neuroblastoma metastasis in a tubulin-independent manner via RhoA/ROCK signaling and enhanced transendothelial migration
Oncogene (2017)
-
Transgelin is a marker of repopulating mesangial cells after injury and promotes their proliferation and migration
Laboratory Investigation (2012)
-
Fibrillin-1 regulates mesangial cell attachment, spreading, migration and proliferation
Kidney International (2006)