Abstract
Study Design:
Cross-sectional comparison.
Objective:
The mortality rate is higher in individuals with spinal cord injury (SCI), and one major cause is cardiovascular disease (CVD). In the general population, the metabolic syndrome (MetS) is associated with an increased risk of CVD, and abdominal obesity is a major feature. Adipokines, secreted by adipose tissue, contribute to obesity-linked metabolic diseases. The aim of this study is to evaluate the prevalence of MetS, the components of this syndrome, especially body composition, and the relations between adipokines and body composition, in SCI individuals.
Setting:
Kanagawa Rehabilitation Hospital, Kanagawa, Japan.
Methods:
Forty-four male SCI individuals (57±13 years and 28 paraplegia) and age-matched able-bodied controls were studied. Body composition was assessed by dual-energy X-ray absorptiometry (DXA) and anthropometry (waist circumference). The visceral fat area (VFA) was measured by computed tomography (CT). Plasma adipokine levels, including that of leptin, adiponectin and plasminogen activator inhibitor-1 (PAI-1), were measured.
Results:
Overall, 43% of SCI individuals met the criteria for MetS. Total and regional fat mass (FM), as well as VFA, were higher, whereas total and regional lean mass, except for arm, were lower than able-bodied controls. In the SCI, leptin and PAI-1 levels were positively associated and adiponectin levels were negatively associated with waist circumference, VFA and trunk FM. In multiple regression models, only leptin level was independently associated with waist circumference, VFA and trunk FM.
Conclusion:
SCI individuals were predisposed to excessive abdominal obesity, and higher leptin levels were strongly associated with higher prevalence of abdominal obesity in this population.
Similar content being viewed by others
Introduction
The longevity of individuals with spinal cord injury (SCI) has improved, but the mortality rate is still higher than that of the general population.1 The most common underlying and contributing cause of death is cardiovascular disease (CVD),1 and the SCI population has a higher incidence of ischemic heart disease than able-bodied population.2 Recently, the presence of metabolic syndrome (MetS) has been used to identify individuals at high risk for CVD in the general population.3 MetS is characterized by low levels of high-density lipoprotein cholesterol (HDL-C), elevated fasting glucose and triglyceride (TG), abdominal obesity and high blood pressure (BP).4
Abdominal obesity is a major characteristic of MetS; it is defined as an excess accumulation of body fat. Since measurement of body fat accurately is not conventional in a clinical setting, body mass index (BMI) has been used as a surrogate marker. Increased BMI is associated with an increased risk of chronic heart disease in the general population.5 However, BMI measurements of the SCI individuals may not be sensitive indicators, since individuals with chronic SCI have a greater fat mass (FM) and a lower fat-free mass per unit BMI than able-bodied controls.6
Fat mass, measured by magnetic resonance imaging (MRI), computed tomography (CT) or dual-energy X-ray absorptiometry (DXA), is more accurate compared with measurement of BMI. Furthermore, simple anthropometric measurements, such as waist circumference, can also be used. On the basis of these specific markers, several studies have shown that SCI individuals have a lower total body and regional lean mass (LM), especially in lower limb, and a higher FM than controls.7, 8, 9
Adipose tissue is an important secretory organ that produces various bioactive substances known as adipokines, which include leptin, tumor necrosis factor-α, adiponectin and plasminogen activator inhibitor-1 (PAI-1); they contribute to obesity-linked metabolic and vascular diseases, as well as MetS.10 In the SCI population, correlation between adipokine levels and body composition is assumed to be different from that in general population because of differences in location of adipose tissue. Additionally, it is still unknown as to which types of the adipokine levels can reflect abdominal obesity in this population.
The primary aims of this study were to evaluate the prevalence of MetS, the components of this syndrome, especially body composition, and the relations between adipokine levels and body composition, in SCI individuals. We hypothesized that the prevalence of MetS, especially abdominal obesity, is high, and the strong relationship between adipokine levels and the markers of abdominal obesity in this population.
Materials and methods
Patients
Forty-four male SCI individuals (an average age of 57±13 years; range, 26–82 years) were studied at the Kanagawa Rehabilitation Hospital (Kanagawa, Japan). The SCI group consisted of 16 tetraplegics and 28 paraplegics with 64% complete and 36% incomplete injury, respectively. SCI was due to traumatic injury in 34 individuals (77%), vascular disease in 3 (7%), infection in 2 (5%), disc disease in 1 (2%), tumor in 1 (2%) and other causes in 3 individuals (7%). Duration of injury was 26±15 years (range, 0.5–57 years). Thirteen (30%) and eight (18%) individuals were on antihypertensive medication and on medication for hypertriglyceridemia, respectively. None of the individuals had signs of acute infection and none were treated with insulin. Two different control groups were enrolled: group A (n=125) served as controls primarily for BP and laboratory data, and group B (n=50) served as controls primarily for body composition. We extracted the data of control individuals from two different health examination databases. The Ethics Committee of Kanagawa Rehabilitation Hospital approved the study protocol, and written informed consent was obtained from all SCI individuals.
Body composition measurements
In the SCI group, body weight, height and waist circumference at the umbilical level were measured in the supine position. For individuals who could not extend all joints fully, the distance from the top of head to the bottom of the heel was measured. In contrast, in the control group, these parameters were measured in the standing position. BMI was defined as the body weight in kilograms divided by the square of the height in meters. Total and regional body composition, including LM and body FM, were evaluated by DXA (DPX-IQ; Lunar Corp., Madison, WI, USA) using Lunar software version 4.6b. Visceral fat area (VFA) was measured by CT at the umbilical level, using a software program (FatScan; N2system, Osaka, Japan). Waist circumference, VFA and trunk FM were used as markers of abdominal obesity.
Blood sampling and laboratory analysis
Blood samples were drawn after an overnight fast. The whole blood samples were centrifuged at 3000 g for 10 min. Levels of TG, HDL-C and fasting plasma glucose (FPG) were measured by an automatic analyzer in a clinical laboratory. Serum insulin was measured using an immunoradiometric assay (SRL Inc., Tokyo, Japan). An estimate of insulin resistance was calculated on the basis of the homeostasis model assessment of insulin resistance using the following formula: FPG (mg dl−1) × fasting serum insulin (μU ml−1)/405.11 Plasma leptin levels were measured using a radioimmunoassay kit (Linco Research Inc., St Charles, MO, USA), plasma adiponectin levels were measured using an enzyme-linked immunosorbent assay kit (Otsuka Pharmaceutical Co. Ltd., Tokyo, Japan) and plasma PAI-1 levels were measured using an enzyme-linked immunosorbent assay kit (Sysmex International Reagents Co. Ltd., Hyogo, Japan).
Definition of the MetS
Definition of the MetS was based on the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III),4 and we modified the definition of visceral fat obesity. The Japanese Society for the Study of Obesity defined visceral fat obesity in Japanese as a VFA >100 cm2, which corresponds to a waist circumference >85 cm for men and >90 cm for women.12 In this study, MetS was defined as the presence of at least three of the following criteria: VFA >100 cm2, TG ⩾150 mg dl−1 or on medication for hypertriglyceridemia; HDL-C <40 mg dl−1 in men and 50 mg dl−1 in women; BP ⩾130/85 mm Hg or on antihypertensive medication and FPG ⩾110 mg dl−1 or on medication for diabetes. BP was measured in the sitting position.
Statistical analysis
Data are presented as mean±s.d. or median and range as appropriate. A P-value of less than 0.05 was considered statistically significant. For continuous variables, the distribution was tested by the Shapiro–Wilk W-test. Then, Student's t-test was used for normally distributed variables, and the Wilcoxon's rank-sum test was used for skewed variables. The Spearman correlation coefficient (ρ) was used to determine the relationships between clinical parameters. Nominal variables were tested using the χ2-test or Fisher's exact test when appropriate. Multiple regression models, including age, TG, plasma leptin, plasma adiponectin and plasma PAI-1 level, were used to identify the independent predictors of the body composition markers. Statistical analyses were performed using JMP, version 5.1.1 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
The clinical characteristics of the male SCI individuals are shown in Table 1; 43% of SCI individuals met the criteria for MetS. Mean waist circumference, VFA and trunk FM were 88.1±12.1 cm, 191±79 cm2 and 12 000±5200 g, respectively. Prevalence of MetS, BMI, waist circumference, VFA, total and trunk FM, TG, HDL-C and adipokines level were similar between tetraplegic and paraplegic individuals, whereas tetraplegic individuals had lower systolic BP (107±15 versus 129±16 mm Hg, P<0.01) and diastolic BP (67±12 versus 76±9 mm Hg, P<0.01) than paraplegic individuals. Furthermore, 12 paraplegics received antihypertensive, whereas only one tetraplegic received antihypertensive.
Table 2 shows comparisons of clinical data between the SCI and able-bodied control individuals. Age was similar between three groups. The SCI individuals had lesser height as compared with individuals in the two different control groups (P<0.01). Although body weight tended to be lower and BMI tended to be higher among the SCI, these did not achieve statistical significance (P=0.06). The SCI individuals had lower systolic BP (P=0.02), diastolic BP (P<0.01) and HDL-C (P<0.01) as compared with individuals in control group A. TG and FPG were similar between the individuals of the SCI group and control group A. Regarding the other markers of body composition, waist circumference and arm LM were similar between the individuals of the SCI group and control group B. Leg LM (P<0.01), trunk LM (P<0.01) and total LM (P<0.01) were lower, whereas VFA (P<0.01), arm FM (P<0.01), leg FM (P<0.01), trunk FM (P<0.01) and total FM (P<0.01) were higher in the individuals SCI group than those in control group B.
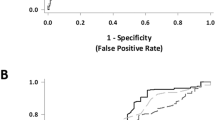
Figure 1 shows comparisons of the markers of abdominal obesity. The individuals with SCI had higher VFA (191±79 versus 135±70 cm2, P<0.01) and higher trunk FM (12 000±5200 versus 9120±3960 g, P<0.01). However, there was no significant difference in waist circumference (88.1±12.1 versus 85.7±7.8 cm, P=0.33) between the two groups.
The results of the Spearman correlation tests are summarized in Table 3. All markers of body composition, including BMI, waist circumference, VFA and trunk FM, were closely interrelated (P<0.01). Plasma leptin levels, plasma PAI-1 levels and homeostasis model assessment of insulin resistance were positively associated with these parameters of body composition (P<0.05). In contrast, plasma adiponectin levels were associated only with VFA (ρ=−0.38, P<0.01). TG levels were positively associated with all of these markers, except for VFA, whereas HDL-C levels were not associated with any marker.
Table 4 shows the results of the multiple regression models that included age, TG, plasma leptin, plasma adiponectin and plasma PAI-1. Most of these variables showed relationship to the markers of abdominal obesity in univariate analyses. Only plasma leptin levels were independently associated with waist circumference (total adjusted R2=0.475, P<0.01), VFA (total adjusted R2=0.379, P<0.01) and trunk FM (total adjusted R2=0.554, P<0.01).
Discussion
One of the chief purposes of this study is to evaluate the prevalence of MetS and the components of this syndrome, especially body composition in SCI. In the present study, 43% of male SCI individuals met the criteria for MetS as defined by the modified NCEP definition. The original NCEP ATP III definition includes a cut-off for abdominal obesity (waist circumference, >102 cm for men and >89 cm for women) that has been shown to be inappropriate for Asian populations;13 therefore, Japanese Society for the Study of Obesity defined the cut-off point of visceral fat obesity in Japanese as a VFA >100 cm2, which corresponds to a waist circumference >85 cm for men and >90 cm for women.12 Although we did not have age-matched controls who met the criteria for MetS in the control group, the prevalence of MetS, especially in SCI men, appeared to be higher than that reported in general Japanese workers (19.5% in men and 7.9% in women).14 Further studies with a greater number of individuals are needed to confirm the higher prevalence of MetS in SCI individuals.
Abdominal obesity per se is a risk factor for CVD. In the general population, as reflected in the 5881 participants of the Framingham Heart Study, Kenchaiah et al.5 reported that the risk of heart failure increased by 5% in men and 7% in women for each unit increment in the BMI. Since body weight does not distinguish between FM and fat-free mass, the BMI would appear to be a poor surrogate marker of obesity in SCI individuals. Buchholz et al.15 found that the 30 kg m−2 BMI cut-off level had a 100% specificity and only a 20% sensitivity in distinguishing obese from non-obese individuals with paraplegia. Indeed, in the present study, the BMI was not significantly different between the SCI group and able-bodied controls.
Thus, more accurate ways to measure visceral fat in the SCI population are needed. In this study, waist circumference, VFA determined by CT and trunk FM determined by DXA were used as markers of abdominal obesity. As expected, these three parameters were closely interrelated. Leg LM, trunk LM and total LM were lower, whereas arm FM, leg FM, trunk FM and total FM, as well as VFA and waist circumference, were higher in the SCI group. These results are consistent with previous reports. Spungen et al.7 reported that total body and regional LM were lower and FM was higher in male SCI individuals using DXA. Modlesky et al.8 reported that the skeletal muscle mass of the mid-thigh determined by MRI and the fat-free soft tissue mass of the mid-thigh determined by DXA were lower in the male SCI population. However, to the best of our knowledge, this is the first report to demonstrate abdominal obesity in the SCI population based on the VFA on CT.
The other chief finding of the present study was that, on multiple regression analyses, plasma leptin level was an independent determinant of the markers of abdominal obesity, including waist circumference, VFA and trunk FM. A range of soluble products, the so-called adipokines, secreted by adipose tissue, which is a highly active endocrine organ, plays an important role in the creation of abdominal fat. Leptin, the product of the adipose-specific ob gene, regulates food intake and energy expenditure. Furthermore, leptin induces high BP and tachycardia via increased adrenergic activity; this suggests that leptin may be an important link between obesity, increased sympathetic activity and hypertension.16 Among SCI individuals, several univariate analyses have shown that leptin levels are positively associated with BMI and FM.17 Additionally, Mamoun et al.17 reported that the leptin levels increased gradually from week 24 after injury. Although in the present study, plasma adiponectin, plasma PAI-1 and homeostasis model assessment of insulin resistance were related to abdominal obesity, only the plasma leptin level was an independent determinant of abdominal obesity in multiple regression models.
There are several limitations of this study. First, the number of the SCI individuals was relatively small. Additionally, we used two separate control groups for different comparisons. We obtained the data of control individuals from two different health examination databases; one was mainly for laboratory data and the other was mainly for body composition, including CT, DXA and anthropometry. Hence, we could not compare all measures against the same control group, and could not assess the prevalence of MetS among able-bodied controls. Second, selection bias was inevitable. All SCI individuals were hospital-based, while most of the laboratory data of the able-bodied controls were obtained during routine physical examination. Third, we did not monitor physical activity, which was reported to attribute an increased FM in the SCI.18 Fourth, we used the same criteria of MetS as for general population. The criteria of abdominal obesity might be different, because of differences in location of adipose tissue in the SCI.
In conclusion, SCI individuals were predisposed to excessive abdominal obesity represented by waist circumference, VFA and trunk FM. The strong relationship between serum leptin and abdominal obesity suggests that this hormone can be used as a surrogate marker of the MetS in SCI individuals. Since the effects of the MetS on CVD in SCI are still unknown, further studies, particularly longitudinal studies with more individuals, are needed.
References
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
Yekutiel M, Brooks ME, Ohry A, Yarom J, Carel R . The prevalence of hypertension, ischaemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Paraplegia 1989; 27: 58–62.
Malik S, Wong ND, Franklin SS, Kamath TV, L'Italien GJ, Pio JR et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation 2004; 110: 1245–1250.
Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG et al. Obesity and the risk of heart failure. N Engl J Med 2002; 347: 305–313.
Jones LM, Legge M, Goulding A . Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil 2003; 84: 1068–1071.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson Jr RN, Waters RL et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol 2003; 95: 2398–2407.
Modlesky CM, Bickel CS, Slade JM, Meyer RA, Cureton KJ, Dudley GA . Assessment of skeletal muscle mass in men with spinal cord injury using dual-energy X-ray absorptiometry and magnetic resonance imaging. J Appl Physiol 2004; 96: 561–565.
Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G . Body composition assessment in spinal cord injury subjects. Acta Diabetol 2003; 40 (Suppl 1): S183–S186.
Prins JB . Adipose tissue as an endocrine organ. Best Pract Res Clin Endocrinol Metab 2002; 16: 639–651.
Haffner SM, Miettinen H, Stern MP . The homeostasis model in the San Antonio Heart Study. Diabetes Care 1997; 20: 1087–1092.
Examination Committee of Criteria for ‘Obesity Disease’ in Japan; Japan Society for the Study of Obesity. New criteria for ‘obesity disease’ in Japan. Circ J 2002; 66: 987–992.
Tan CE, Ma S, Wai D, Chew SK, Tai ES . Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care 2004; 27: 1182–1186.
Anuurad E, Shiwaku K, Nogi A, Kitajima K, Enkhmaa B, Shimono K et al. The new BMI criteria for Asians by the regional office for the western pacific region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health 2003; 45: 335–343.
Buchholz AC, McGillivray CF, Pencharz PB . The use of bioelectric impedance analysis to measure fluid compartments in subjects with chronic paraplegia. Arch Phys Med Rehabil 2003; 84: 854–861.
Carlyle M, Jones OB, Kuo JJ, Hall JE . Chronic cardiovascular and renal actions of leptin: role of adrenergic activity. Hypertension 2002; 39: 496–501.
Mamoun L, Puech AM, Manetta J, Badiou S, Paris F, Ohanna F et al. Circulating leptin concentrations can be used as a surrogate marker of fat mass in acute spinal cord injury patients. Metabolism 2004; 53: 989–994.
Phillips WT, Kiratli BJ, Sarkarati M, Weraarchakul G, Myers J, Franklin BA et al. Effect of spinal cord injury on the heart and cardiovascular fitness. Curr Probl Cardiol 1998; 23: 641–716.
Acknowledgements
We thank Dr Taichi Sekine (Mitsubishi Kagaku Bio-Clinical Laboratories Inc., Kanagawa, Japan) for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maruyama, Y., Mizuguchi, M., Yaginuma, T. et al. Serum leptin, abdominal obesity and the metabolic syndrome in individuals with chronic spinal cord injury. Spinal Cord 46, 494–499 (2008). https://doi.org/10.1038/sj.sc.3102171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102171
Keywords
This article is cited by
-
A comprehensive look at the psychoneuroimmunoendocrinology of spinal cord injury and its progression: mechanisms and clinical opportunities
Military Medical Research (2023)
-
Endocrinological and inflammatory markers in individuals with spinal cord injury: A systematic review and meta-analysis
Reviews in Endocrine and Metabolic Disorders (2022)
-
Evaluation of cardiovascular disease risk in individuals with chronic spinal cord injury
Spinal Cord (2021)
-
Role of exercise on visceral adiposity after spinal cord injury: a cardiometabolic risk factor
European Journal of Applied Physiology (2021)
-
Skeletal muscle hypertrophy and attenuation of cardio-metabolic risk factors (SHARC) using functional electrical stimulation-lower extremity cycling in persons with spinal cord injury: study protocol for a randomized clinical trial
Trials (2019)