Abstract
Objectives:
The objective of this article is to probe the surgical procedures of treatment for Chiari I malformation (CMI) associated with syringomyelia and evaluate their efficacy based on clinical and neuroradiological results.
Study design:
Retrospective study.
Setting:
Department of Neurosurgery in Qilu Hospital of Shandong University in China.
Methods:
We retrospectively reviewed 316 surgically treated patients with CMI. We classified our patients after surgery in four global outcome categories as follows: very good (complete remission or marked improvement), good (slight improvement), fair (stability), poor (slight or marked deterioration). We simply describe the postoperative diameter of the syrinx (collapse, decreased, unchanged or increased).
Results:
At the time of discharge, the result was very good in 163 cases (51.58%), good in 92 cases (29.11%), fair in 49 cases (15.51%) and poor in 12 cases (3.80%). In the follow-up period, neurological status improved and was then sustained in 94.49% of patients (206/218). At more than 2 years after surgery, we were able to compare pre- and postoperative MR images in 218 patients. A collapse of the syrinx was seen in 34.86% (76/218) of patients. The size of the syrinx was decreased in 31.65% (69/218) of patients, remained unchanged in 26.15% (57/218) of patients and increased in 7.34%(16/218) of patients.
Conclusion:
Patients with CMI should be treated using various surgical procedures according to different magnetic resonance imaging types; surgical treatments may fully decompress the medulla oblongata and ameliorate the clinical syndromes.
Similar content being viewed by others
Introduction
Chiari I malformation (CMI), defined as herniation of cerebellar tonsils below the level of foramen of magnum to the upper cervical canal is commonly associated with syringomyelia as a result of deranged cerebrospinal fluid (CSF) dynamics at the craniovertebral junction and upper cervical canal. It has been treated using a variety of surgical procedures. Surgical outcomes have been reported with varying results throughout the literature. The objective of this article is to probe the surgical procedures of treatment for CMI associated with syringomyelia and evaluate their efficacy on the basis of clinical and neuroradiological results.
Materials and methods
Patients
A total of 316 symptomatic patients with CMI were treated surgically in the Department of Neurosurgery at Qilu Hospital of Shandong University between January 1990 and August 2006. We analyze retrospectively the surgical results.
Clinical presentations
The clinical features of these 316 patients are detailed in Table 1.
Radiological examination
Magnetic resonance imaging (MRI) was performed in all patients and X-rays, in 150 patients. The X-ray findings of 150 patients are listed in Table 2. CMI was defined as tonsillar herniation extending at least 5 mm below the foramen magnum without a descent of the vermis and the fourth ventricle,1 as determined by a sagittal MRI scan. A total of 316 cases of CMI were classified into A, B, C and D types on the basis of their MRI properties, which are summarized in Table 3.
Surgical operations
Surgical intervention is indicated in symptomatic patients with neuroradiological abnormalities. A total of 316 patients with CMI were surgically treated and divided into four groups according to the main surgical procedure. The main surgical procedures of 316 patients with CMI are summarized in Table 4.
Each of the 316 patients underwent suboccipital decompression using the standard approach. An occipital craniectomy was performed (approximately 4 × 3 cm), which included removal of the posterior rim of the foramen magnum following a laminectomy of C1 and C2 (2 cm). The posterior atlanto-occipital membrane, that is, the dural band, was separated completely from the dura mater and removed. If syringomyelia is present and needs to be drained, the laminectomy includes C3 and possibly the upper part of C4 to prepare for drainage of the cavity at the C3 level. The level of the cervical laminectomy also depends on the level of tonsillar herniation so that the level below the herniated tonsils is reached.
The cerebellar tonsillectomy was performed in 149 patients with Chiari I (tonsils to C2–C3), following the same procedures described above plus dural opening in Y format, dissection of arachnoid adhesion between the cerebellar tonsils, medulla oblongata and spinal cord, incision of arachnoid adherences at regional vasculature, tonsillectomy, large opening of the fourth ventricle and dural grafting with the use of autologous cervical fascia. After completion of the dural grafting, the dura was hooked up by a stitch through the graft at the level of the foramen magnum and fixed to the cervical fascia.
The syringosubarachnoid shunt was conducted in 82 CMI patients with syringomyelia (above C3). After the Chiari malformation has been decompressed, the syrinx is drained into the subarachnoid space through a longitudinal incision, approximately 10 mm long, in the dorsal root entry zone at the C2 or C3 level on the side of greater deficit related to the cervical sensory nerves. The dorsal root entry zone between the lateral and posterior columns is selected for the myelotomy because it is consistently the thinnest area in patients with syringomyelia. A dural wick, approximately 0.5 × 2 cm, attached to the dura mater and anchored to a dentate ligament, is threaded downward into the hydromyelic cavity. The dural wick serves to maintain the patency of the incision so that fluid drains through the myelotomy around the dural wick into the enlarged CSF space around the myelotomy and Chiari malformation. The arachnoid membrane was closed over the myelotomy site. Other surgical manipulations were the same as described above.
As for 14 patients with atlanto-axial subluxation, the operation was completed with the help of an orthopedist.
Follow-up
Modes of follow-up consist of outpatient service, home visit, letters and phone calls.
Results
A total of 316 symptomatic patients with CMI were treated surgically in our department between January 1990 and August 2006, of whom 236 were with syringomyelia. Their age ranged from 7 to 65 years (mean of 37.8 years, 146 men and 170 women). The duration from onset of symptoms to diagnosis ranged from 0.5 to 40 years (mean of 4.51 years). The clinical features of these 316 patients are detailed in Table 1. The main surgical procedures and results of 316 patients with CMI are summarized in Table 4.
We classified our patients after surgery into four global outcome categories as follows: very good (complete remission or marked improvement), good (slight improvement), fair (stability), poor (slight or marked deterioration). For each individual patient, the classification in a particular outcome category was based on the evolution of the major symptoms and signs and their influence on disability and subjective discomfort.
At the time of discharge, the result was very good in 163 cases (51.58%), good in 92 cases (29.11%), fair in 49 cases (15.51%) and poor in 12 cases (3.80%).
Concerning postoperative complications, we have observed infection in five (1.58%) patients, respiratory failure in three (0.95%) patients, CSF fistulae in two (0.63%) patients and aseptic meningitis in 40 (12.60%) patients. Four deaths occurred among patients with poor results: two of respiratory complications (respiratory infection and respiratory failure, respectively), and another two due to intracranial infection.
A total of 218 patients were followed up. The follow-up varied from 5 to 108 months. In the follow-up period, neurological status improved and was then sustained in 94.49% of patients (206/218).
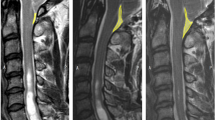
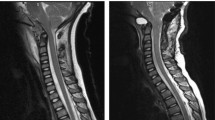
At more than 2 years after surgery, we were able to compare pre- and postoperative MR images in 218 patients (Figures 1 and 2). We simply describe the diameter of the syrinx (collapse, decreased, unchanged or increased). A collapse means that the diameter of the syrinx has become zero. A collapse of the syrinx was seen in 34.86% (76/218) of patients. The size of the syrinx was decreased in 31.65% (69/218) of patients, remained unchanged in 26.15% (57/218) of patients and increased in 7.34% (16/218) of patients.
The study result indicates that surgical treatment may fully decompress the Chiari malformation and syringomyelia and ameliorate the clinical syndromes.
Discussion
Chiari I malformation, defined as herniation of cerebellar tonsils below the level of foramen of magnum to the upper cervical canal, is commonly associated with syringomyelia as a result of deranged CSF dynamics at the craniovertebral junction and upper cervical canal. It has been treated using a variety of surgical procedures. Surgical outcomes have been reported with varying results throughout the literature.
It is widely believed that CMI results from the fact that the basiochondrocranium is smaller due to an underdevelopment of the basiooccipital.2 With a small posterior fossa, the ulterior development of the cerebellum will cause a herniation of the cerebellar tonsils and concomitant crowding at the level of the foramen magnum. Syringomyelia results from abnormalities at the craniocervical junction. The mechanisms leading to progression of syringomyelia associated with CMI are still debated. Gardner and Angel3 believe that the water-hammer effect brought about by pressure waves coming from the choroid plexuses is transmitted to the CSF causing an enlargement of the central canal of the spinal cord. Oldfield et al.4 proposed that the formation of syringomyelia might result from downward migration of the tonsils, producing a systolic pressure wave, which acts on the surface of the spinal cord like pistons. Williams5 takes the gradient that exists between the intracranial and the intraspinal pressure as the cause of syringomyelic cavitation. The perpetuation of phases of craniospinal pressure dissociation (the ‘suck’ effect) causes the formation and maintenance of syringomyelia.
In patients with syringomyelia associated with Chiari malformation, surgical intervention is indicated in symptomatic patients with neuroradiological abnormalities. Several different neurosurgical procedures are used for treatment,6 including suboccipital decompression, alone or combined with any of the following: syringe-subarachnoid shunt; tonsillectomy and so on.
Although many different surgical options are available, suboccipital decompression (D) has been widely accepted as a preferred procedure with or without additional manipulations.4, 7, 8, 9 It involves removing bone in the suboccipital area along with the posterior margin of the foramen magnum and usually the posterior ring of the C1 vertebra. In our study, each of the 316 patients with CMI underwent, alone or combined with other surgical procedures, suboccipital decompression; suboccipital decompression was alone performed in Chiari I (tonsils to C1) patients without syringomyelia or with syringomyelia (below C3). It may expand the posterior fossa and relieve the pressure of the cerebellar tonsils against the medulla oblongata so that CSF circulation around the foramen magnum is improved.
As to the cerebellar tonsils, some surgeons leave them intact, proceeding only with the opening of the fourth ventricle.10 Guyotat et al.6 found better results in terms of clinical outcome and syrinx reduction when the tonsils were resected in those patients with Chiari I malformation associated to syringomyelia.7 In our study, tonsillectomy was performed in Chiari I (tonsils to C2 or C3) patients. In our opinion, the dissection of the tonsils was stopped in all patients the moment a reasonable flow of CSF from the fourth ventricle was obtained, whether this required coagulation or resection of the tonsils or no manipulation at all. Partial resection of the tonsils and dissection of arachnoid adhesion between the cerebellar tonsils, medulla oblongata and spinal cord on the basis of bone decompression may keep the median aperture of the fourth ventricle unobstructive.
Some authors have suggested that syringostomy or syringosubarachnoid shunt is unnecessary because there is no significant relationship between clinical findings and the size of the syrinx.4, 11Direct treatments that eliminate the syrinx may not produce clinical improvement, presumably because of irreversible cord impairment resulting from the operation. Other authors have recommended the syringosubarachnoid shunt as a major surgical option for Chiari I malformation associated with syringomyelia in those patients with a large syrinx who had very mild or no disturbance of the cranial nerve and cerebellar function.12 They have reported that collapse of the syrinx occurred faster and that pain relief outcome was superior with this treatment than with foramen magnum decompression. Some authors believed that the most effective treatment for Chiari malformation and syringomyelia is suboccipital decompression and duraplasty in conjunction with drainage of syringomyelia cavity if there is significant distention of the spinal cord.13, 14 The syringosubarachnoid shunt was conducted in 82 CMI patients with syringomyelia (above C3) in the current study. After syringosubarachnoid shunt, the collapse of the syrinx cavity may make the previously enlarged spinal cord and spinal subarachnoid space gradually restore normalization, which may facilitate CSF and spinal blood circulation so that the function of spinal cord may recover faster.
Complications of decompression with intradural manipulations include infection, aseptic meningitis or arachnoiditis, CSF leakage, pseudomeningoceles, hydrocephalus, apnea and other systemic dysfunctions. Klekamp et al.'s8 results showed that a considerable number of patients developed complications after foramen magnum decompression. Aseptic meningitis and CSF leakage/pseudomeningoceles accounted for 20.3% (27/133) of complications.
The majority of our patients presenting with major signs and symptoms improved after surgical treatment. Some authors have concluded that surgical treatment results in the improvement or stabilization of the disease in the majority of patients.8, 15 José Dones and De Jesús16 found that the main benefit of surgical treatment in patients with Chiari I malformation is to arrest the progression of symptoms. This pattern is not so clearly recognizable in our results, probably due to the small number of patients. It has been described that headache and neck pain usually respond best to decompressive surgery, explained by the relief of the craniospinal pressure difference. Amyotrophy in the upper extremities responds very badly, suggesting irreversible destruction of anterior horn cells by the syrinx.17 Our study also found similar results.
Care should be taken during operation: (1) the operation was performed with the patients in the three-quarter prone position with the table tilted to place the head above the trunk.13, 14 Marked flexion of the neck during surgery for Chiari malformation has been reported to increase the neurologic deficit or cause respiratory problems;18 (2) when using a cranial drill, put the drill bit inside the ring of hemostat and take strict precautions during operation to prevent slipping of the cranial drill around the occiput; (3) as to bony decompression, an occipital craniectomy (approximately 4 × 3 cm) following craniectomy of C1–C3 should be considered suitable for patients with CMI. Overdecompression of the hindbrain has been implicated8 as the cause of ‘slumping’ of the cerebellum. This downward migration of the hindbrain is considered to be a major cause of postoperative deterioration and (4) the incidence of cervical instability varied depending on whether less or not less than four laminas were removed.19 If laminectomy includes not less than four laminas, the attachment of splenius capitis and semispinalis capitis will inevitably be destroyed. Long-term observations show that there is an adverse outcome in patients undergoing multilevel cervical laminectomy such as instability or deformity of the cervical column, raising head feebly and so on. (5) Drainage of hydromyelic cavity through the dorsal root entry zone into the subarachnoid space should be performed if there is significant distention of the cervical spinal cord. For drainage of syringomyelia, a vertical incision approximately 1 cm long is made into the thinnest area along the dorsal root entry zone. The myelotomy is long enough such that the fluid drains into the enlarged CSF space around the myelotomy and Chiari malformation. Fujii et al.20, among others, have proposed that foramen magnum decompression with syringosubarachnoid shunt is effective for patients with a large syrinx over 35% of the syringo-cord ratio because syringosubarachnoid shunt is difficult and aggravates the injury over the spinal cord if the syringo-cord ratio is less than 35%. (6) Care should be taken to avoid placing the dural incision and the myelotomy in such close approximation that healing results in scarring, which tethers the cord to the dura because repetitive movement of the spine may result in damage to the tethered cord.
In conclusion, patients with CMI associated with syringomyelia should be treated using various surgical procedures according to different MRI types; the surgical procedures include suboccipital decompression, alone or combined with any of the following: syringe-subarachnoid shunt; tonsillectomy and so on. Surgical treatments may fully decompress the medulla oblongata and ameliorate the clinical syndromes.
References
Barkovich AJ, Wippold JF, Sherman JL, Citrin CM . Significance of cerebellar tonsillar position on MR. AJNR Am J Neuroradiol 1986; 7: 795–799.
Marin-Padilla M, Marin-Padilla T . Morphogenesis of experimentally induced Arnold–Chiari malformation. J Neurol Sci 1981; 50: 29–55.
Gardner WJ, Angel J . The mechanism of syringomyelia and its surgical correction. Clin Neurosurg 1958; 6: 131–140.
Oldfield EH, Muraszko K, Shawker TH . Pathophysiology of syringomyelia associated with Chiari malformation of the cerebellar tonsils: implication for diagnosis and treatment. J Neurosurg 1994; 80: 3–15.
Williams B . Surgery for hindbrain related syringomyelia. In: Advances and Technical Standards in Neurosurgery, vol. 20 Springer Verlag: Berlin, 1993 pp 108–164.
Guyotat J, Bret P, Jouanneau E, Ricci AC, Lapras C . Syringomyelia associated with type I Chiari malformations. A 21-year retrospective study on 75 cases treated by foramen magnum decompression with a special emphasis on the value of tonsils resection. Acta Neurochir 1999; 140: 745–754.
Milhorat TH, Johnson WD, Miler JI, Bergland RM, Hollenberg-Sher J . Surgical treatment of syringomyelia based on magnetic resonance imaging criteria. Neurosurgery 1992; 31: 231–245.
Klekamp J, Batzdorf U, Samii M, Bothe HW . The surgical treatment of Chiari I malformation. Acta Neurochir (Wien) 1996; 138: 788–801.
Takigami I, Miyamoto K, Kodama H, Hosoe H, Tanimoto S, Shimizu K . Foramen magnum decompression for treatment of Arnold Chiari malformation type I with associated syringomyelia in an elderly patient. Spinal Cord 2005; 43: 249–251.
Sahuquillo J, Rubio E, Poca MA, Rovira A, Rodriguez-Baeza A, Cervera C . Posterior fossa reconstruction: a surgical technique for the treatment of Chiari I malformation and Chiari I/syringomyelia complex. Neurosurgery 1994; 35: 874–885.
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C et al. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 1999; 44: 1005–1017.
Iwasaki Y, Hida K, Koyanagi I, Abe H . Reevaluation of syringosubarachnoid shunts for syringomyelia with Chiari malformation. Neurosurgery 2000; 46: 407–413.
Rhoton Jr AL . Microsurgery of syringomyelia and syringomyelic cord syndrome. In: Schmidek HH, Sweet WH (eds). Operative Neurosurgical Techniques: Indications, Methods, and Results, vol. 2, 3rd edn. Grune & Stratton: New York, USA, 1995, pp 116–118.
Jacob RP, Rhoton Jr AL . The Chiari I malformation. In: Anson JA, Benzel EC, Award IA (eds). Neurosurgical Topics: Syringomyelia and the Chiari Malformations. The American Association of Neurological Surgeons: Park Ridge, IL, USA, 1996, pp 96–98.
Bindal AK, Dunsker SB, Tew Jr JM . Chiari malformation: classification and management. Neurosurgery 1995; 37: 1069–1074.
Dones J, De Jesús O . Clinical outcomes in patients with Chiari I malformation: a review of 27 cases. Surg Neurol 2003; 60: 142–148.
Di Lorenzo N, Palma L, Palatinsky E et al. ‘Conservative’ craniocervical decompression in the treatment of syringomyelia–Chiari I complex. Spine 1995; 20: 2479–2483.
Mullan S, Raimondi AJ . Respiratory hazards of the surgical treatment of the Arnold-Chiari malformation. J Neurosurg 1962; 19: 675.
Katsumi Y, Honma T, Nakamura T . Analysis of cervical instability resulting from laminectomies for removal of spinal cord tumor. Spine 1989; 14: 1171–1176.
Fujii K, Natori Y, Nakagaki H et al. Management of syringomyelia associated with Chiari malformation: comparative study of syrinx size and symptoms by magnetic resonance imaging. Surg Neurol 1991; 36: 281–285.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Chen, Y., Chen, Y. et al. Chiari I malformation associated with syringomyelia: a retrospective study of 316 surgically treated patients. Spinal Cord 46, 358–363 (2008). https://doi.org/10.1038/sj.sc.3102141
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102141
Keywords
This article is cited by
-
Chiari malformation type I and basilar invagination originating from atlantoaxial instability: a literature review and critical analysis
Acta Neurochirurgica (2020)
-
The impact of imposed delay in elective pediatric neurosurgery: an informed hierarchy of need in the time of mass casualty crisis
Child's Nervous System (2020)
-
Treatment failure of syringomyelia associated with Chiari I malformation following foramen magnum decompression: how should we proceed?
Neurosurgical Review (2019)
-
The effect of posterior fossa decompression in adult Chiari malformation and basilar invagination: a systematic review and meta-analysis
Neurosurgical Review (2018)
-
Patient-reported Chiari malformation type I symptoms and diagnostic experiences: a report from the national Conquer Chiari Patient Registry database
Neurological Sciences (2015)