Abstract
Study design:
Cross-sectional study.
Objectives:
To investigate the kinematic, kinetic and electromyographic (EMG) aspects of postural control during falling with rapid reach-and-grasp balance reaction in thoracic cord-injured individuals wearing knee-ankle-foot orthoses (KAFOs).
Setting:
Institutional Motion Analysis Laboratory.
Methods:
Seven T7–T12 cord-injured subjects with complete motor loss (ASIA classes A and B) participated in this study. Subjects with KAFOs first stood steady with a modified walker and then released their hold on the walker to maintain self-supported standing until falling with grasping. The center of pressure (COP), center of mass (COM) and joint angles were measured together with EMG of the triceps (TRI), T4 paraspinal and abdominal muscles.
Results:
After release of the walker, there was a rapid increase of COM–COP distance (that is, from 13.32±11.79 to 54.29±24.56 mm), with COM in front of COP during a forward fall, which was associated with the increases of T4 muscle activities. After the reach-and-grasp reaction, COM moved behind COP, which was associated with the increase of ankle dorsiflexion and the TRI and abdominal muscle activities.
Conclusion:
The increase of upper back extensor muscle activity might not be enough to correct postural instability during unsupported stance in thoracic spinal cord injury with complete motor loss. The rapid reach-and-grasp reaction is an alternative compensatory mechanism to prevent falling to the ground.
Similar content being viewed by others
Introduction
The physiological or psychological benefits from stance or ambulation in subjects with spinal cord injury (SCI) are well documented.1, 2 During the rehabilitation period, knee-ankle-foot orthoses (KAFOs) can be applied to SCI patients with lower-extremity paralysis to support the knees and ankles for stance and/or ambulation.3 Although most complete thoracic SCI patients with KAFOs abandon ambulation due to profound energy consumption and risk of falling,2, 4, 5 the standing balance training or balance recovery training during a fall should not be ignored if the standing abilities and physiological conditions of SCI patients are to be improved.
It has been mentioned that a complete thoracic SCI subject with KAFOs usually uses the arm, head and upper trunk to stabilize the hips with the pelvis forward so that the weight line falls posterior to the hip joint to prevent instability.2 However, there is a lack of quantitative analysis of the postural alignment and postural muscle activities during stable and unstable stance. The standing balance or postural stability can be quantified by the biomechanical approach (including kinematic and kinetic analysis).6 The stable stance involves keeping the center of pressure (COP) or center of mass (COM) within the base of support (BOS).7 Recently, the distance between the COM and COP (that is, COM–COP variable; COM minus COP with positive value being unstable) has been used to estimate the functional stability of postural control.8, 9 The present study investigates the COM–COP relation in thoracic SCI subjects with and without stable stance.
Unstable stance may result in an unexpected fall. A fall is often defined as a situation in which the subject drops to the ground, but it can also be defined as any unintended contact with a supporting surface, such as a chair.7 During falling, there is a sudden, unexpected change in upright position, and this often involves outstretched upper extremities as an unintentional compensatory rapid reach-and-grasp balance reaction with a ‘change-in-support’ strategy for balance recovery.4, 10, 11 The ability to reach-and-grasp (grip or touch) structures for support in reaction to instability is suggested to be an important component of the postural control.10, 11 Previous studies have focused more on the impact force12 or the fracture of upper extremities13 during a fall with a rapid reach-and-grasp balance reaction and less on muscular activation.
Some of the thoracic complete SCI subjects with KAFOs may lose balance without arm support,3 and a deficit in postural control might contribute to this unstable stance. The purposes of this study were to investigate the postural control in thoracic SCI subjects with stable stance (that is, arm support) and unstable stance (that is, without support) followed by a rapid reach-and-grasp balance reaction. The research hypotheses in this study were (1) there is a compensatory increase of postural muscle activity during unstable stance, (2) there is a compensatory change of trunk, pelvis, hip, ankle joint angles during unstable stance and (3) a compensatory rapid reach-and-grasp balance reaction during balance recovery brings the COM–COP relation into a stable condition.
Methods
Participants
Seven thoracic cord-injured subjects (T7–T12) with complete motor loss were recruited by chance from the outpatient clinic at National Taiwan University Hospital. All the participants were informed about the protocol and signed a consent form, which was reviewed and approved by the local ethics committee. The inclusion criteria were (1) thoracic SCI with American Spinal Injury Association (ASIA) class A (complete motor and sensory loss) or B (only preservation of sensation extending through the sacral segments S4–S5),14, 15 (2) using a walker with bilateral KAFOs for stance or ambulation in daily living, but losing balance within 5 s when trying to stand unsupported, (3) at least 3 months post-injury and (4) having a full passive range of motion with a modified Ashworth Scale.16 of less than 3 (that is, resistance over full range). The exclusion criteria were musculoskeletal impairments that would affect the experiment.
In ASIA evaluation,14, 15 the muscle strength is scored by manual muscle testing (0–5, with 5 being normal), and the total motor score is 100. A sensory score of a dermatome (C2–S4, 5) is scored (0–2 with 2 being normal) with the total score being 112. The subjects wore traditional typed KAFOs (∼3 kg per leg) with the knee locked in extension, 90° posterior stop of the ankle joint and without dorsiflexion restriction.
Experimental protocol
At the beginning, each subject, with bilateral KAFOs, stood still by holding on to the modified walker and looked straightforward for 5 s. The walker and each foot were on three separate force plates (AMTI OR6-7, Advanced Mechanical Technology Inc., Watertown, MA, USA). The inner borders of the feet were separated by 10–15 cm according to the body height. The subject then released his/her hold on the walker rapidly upon hearing a tone. The trial was ended when the subject regained balance from a fall with a rapid reach-and-grasp balance reaction to stop falling by grasping and pulling or pushing the walker. A safety belt was placed around the waist of the subject, and an assistant was standing by to protect the subject from falling to the ground. Each subject performed the protocols twice.
Equipment
For the kinetic data, three force plates (Advanced Mechanical Technology Inc.) (sampling rate 600 Hz) were used. For the kinematic data, a three-dimensional motion analysis system (3-D Motion Analysis System, VICON 250, Oxford Metrics Ltd, West Way, Oxford, UK) with five cameras (sampling rate 120 Hz) was used. Reflective markers were placed on body segments and the KAFOs for the measurement of joint angle and COM.6
The surface electromyographic (EMG) activities on the muscle bellies of the bilateral triceps (TRI), the right abdominal oblique muscles (ABD) and right T4 paraspinal muscles (T4) were recorded. The T4 paraspinal muscle was recorded because it was the residual muscle for all the T7–T12 participants. For EMG data, Ag-AgCl surface electrodes were used to record EMG, which was amplified by a universal amplifier of a Gould polygraph (Gould Instrument Systems Inc., Valley View, OH, USA) with a gain of 1000 and a common mode rejection ratio of 90 dB. The EMG sampling rate was 1200 Hz, and the band-pass filter was 30–500 Hz.
The modified walker was made of steel rods with the four legs within one force plate, and the handles were extended for grasping. A 60 kg weight was put on the bottom rod of the walker to prevent the tilting of the walker during the trial.
Data analysis
The temporal aspect of the falling event was quantified as follows (Figure 1a). The period from stable standing with holding (f1) to arm release (f2) was supported phase (phase 1). The period from f2 to grasping again (f3) was unsupported phase (phase 2). The period from f3 to peak arm loading on the walker (f4) was arm-loading phase (phase 3).
(a) One example of the COM (center of mass) and COP (center of pressure) curves in a T10 thoracic cord-injured subject during standing with and without arm support. The original zero point is the midpoint between the two lateral malleoli. A positive value of COM–COP difference indicates that the COM is anterior to the COP, and a negative value indicates the opposite. (b) Definitions of the angles of the trunk, pelvis and lower limb segments. +β indicates trunk forward bending, +α anterior pelvic tilt and +θ ankle dorsiflexion while α−θ gives the hip angle with positive values as flexion. ASIS, anterior superior iliac spine; GT, greater trochanter; PSIS, posterior superior iliac spine.
Without arm support, the COM, COP and BOS were measured from the standing body. With arm support, those measurements included the body and the walker. The present study defined the difference of COM and COP (COM−COP) beyond the baseline at a slope greater than 0.05 mm/frame (or 0.05 × 120 mm/s) as the margin of falling out of control (fm) (Figure 1a).
The joint angles were determined from the body segments in reference to the global coordinate system.6 As shown in Figure 1b, an axis joining the C7 and the midpoint between the two posterior superior iliac spines (PSIS's) was used to define the forward and backward bending of the trunk segment relative to the vertical. The pelvic axis was defined as the line connecting the anterior superior iliac spine and PSIS and used to describe the pelvic tilting relative to the horizontal. The axis of the lower limb was defined as the line joining the greater trochanter and lateral malleolus. Since the foot was placed on the ground, the lower limb angle between the lower limb axis and the vertical described the ankle joint motion, while the hip angle was calculated by subtracting the lower limb angle from the pelvic tilting angle. Definitions of the angles are also given in Figure 1b. The moments at the hip and ankle joints were also obtained and normalized by body weight (BW) and leg length.6
The raw EMG signals were integrated by a root mean square (RMS) with a rate of 60 samples/s via AcgKnowledge 3.70 software and a Matlab formula. The EMG data was normalized to the maximal voluntary isometric contraction (% MVC) of the relevant muscles to obtain the normalized average root mean square per unit time (NARMS). The onset time was determined as the time when the EMG magnitude was larger than the baseline mean value plus two standard deviations for 20 ms.
Statistical analysis
The nonparametric Friedman test was used to analyze the difference among three phases (α=0.05). Pairwise comparisons were performed using Wilcoxon's signed-rank test to determine differences between successive time intervals. A value of P<0.025 (that is, 0.05/2) was considered to be statistically significant between two groups.
Results
Six subjects with ASIA class A, and one with class B, were recruited (Table 1). The mean weight-bearing force on the frame during initial supported phase was 1.06±0.49 N (mean±s.e.). After releasing the hold on the walker, all subjects fell forward with a rapid reach-and-grasp balance reaction to stop falling by grasping and pushing the walker. The maximal weight-bearing force on the frame was 152.41±42.32 N after falling with the BW pushing downward.
The movement of the COM and COP of a typical subject during falling with rapid reach-and-grasp balance reaction is shown in Figure 1a. Those for all the subjects are described as follows. During phase 1, the peak COM–COP difference (at f1) was 10.98±9.65 mm. Right after the release of the walker (f2), there was a rapid and significant (P<0.025) increase of the COM–COP distance from 13.32±11.79 to 54.29±24.56 mm, with the COM moving in front of the COP during a forward fall in phase 2. In phase 3, the peak COM–COP difference was −54.86±36.94 mm (at f4), with the COP moving in front of the COM during arm-loading phase to recover balance.
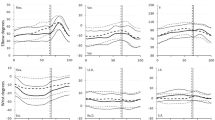
The mean time sequence of falling is shown in Figure 2a. Falling out of control (fm) occurred at 0.95 s post-arm release (that is, onset of perturbation 0 s), and it took another 0.6 s to accomplish the arm grasping. Grasp phase 3, with the greatest arm loading, is 0.43 s.
(a) The time events of fall and the onset time (mean±s.d.) of electromyographic (EMG) activities of left triceps (LTRI), right triceps (RTRI), abdominal muscle (ABD) and T4 paraspinal muscles in seven patients during standing pre- and post-arm release. (b) The EMG normalized average root mean square per unit time (NARMS) of focal muscles (LTRI, RTRI) and postural muscles (ABD and T4) in phase 1 (supported phase), phase 2 (unsupported phase) and phase 3 (arm-loading phase) in thoracic cord-injured subjects during standing. Data are expressed as mean±s.d. (a) P<0.025, if phase 2 vs phase 1; (b) P<0.025 if phase 3 vs phase 2.
The joint peak angles are trunk forward bending, pelvic posterior tilt, hip hyperextension and ankle dorsiflexion in subjects during stance with support in phase 1 (Table 2a). The Friedman test indicated that there was no significant difference (P>0.05) in maximal trunk, pelvis and hip angles among phases 1, 2 and 3. However, there was a significant difference (d.f.=2, F=12.07, P<0.05) in the ankle dorsiflexion angle among phases. The ankle dorsiflexion angle in phase 3 was significantly greater (P<0.025) than that in phase 2 (Table 2a). The normalized hip moment in phase 3 was significantly greater than that in phase 1, and the normalized hip moment was significantly larger than the ankle moment (Table 2b).
The EMG onset time during a fall response is shown in Figure 2a. The mean onset time of postural muscles (ABD and T4) occurs at or before the arm release (f2). The mean onset time of focal muscles (TRI) occurs mainly after arm release but before the point of falling out of control (fm).
The Friedman test and post hoc analysis indicated that there was no significant difference between phase 1 and phase 2 in the NARMS of TRI and ABD muscles (Figure 2b), but T4 in phase 2 (18.57±18.17% MVC) was significantly greater (P<0.025) than that in phase 1 (8.26±7.81% MVC) but not significantly different from that in phase 3 (25.85±28.50% MVC). Instead, there were significant increases (P<0.025) of right TRI and ABD muscle EMG during phase 3 as compared to phase 2 (Figure 2b).
Discussion
This is the first study to investigate natural falling with rapid reach-and-grasp balance reaction in SCI subjects with KAFOs. The present results indicate that the upper back extensor muscles are recruited early, with the rapid reach-and-grasp balance reaction subsequently initiated to bring the body into a stable condition, in thoracic SCI subjects with lower-extremity paralysis during stance without arm support.11 The possible factors causing the postural instability and the compensatory mechanisms of postural control are discussed as follows.
In this study, the seven thoracic SCI subjects with motor and sensory loss or impairment around the lower trunk and lower extremities had to use KAFOs and walkers to maintain stance. Their postural instability was mainly due to deficits in both sensory input and motor actions.7 During quiet stance with walker, the mean weight-bearing force on the frame was small (∼1 N), but the fingertip contact could provide somatosensory and proprioceptive feedback to the brain, and the walker could also provide significant mechanical stabilization to reduce the postural instability.17
The hip extensors and hip flexors were absent or very weak in our motor complete thoracic SCI (Table 1). The hip extension could be locked by Y (iliofemoral) ligaments, but the hip flexion was not restricted.2 Furthermore, the traditional KAFOs had posterior stop at the ankle joints without restriction on dorsiflexion. During unsupported stance with falling, the trunk would flex, or ‘jack-knife’, with the increase of ankle dorsiflexion angle and hip flexion moment (Table 2). A previous study by Matjacic and Bjad18 also found that the most important constraint for a paraplegic arm-free standing with hip-knee locked was the ankle stiffness (approximately 8 N-m/deg) to prevent further dorsiflexion. Therefore, the deficit in ankle stability in the traditional typed KAFOs could not prevent the forward fall. If the ankle joint of the traditional KAFO could be modified by a new type of ankle orthosis with two artificial pneumatic muscles controlled by EMG to produce proper plantar flexion torque,18, 19 or by the functional electric stimulation of the gastrocnemius,2, 20 ankle joint stability might be improved in stance.
The compensatory mechanisms of postural control might include (1) increase in residual postural muscle activity, (2) change in trunk, pelvis, hip, ankle alignment and (3) outreached rapid reach-and-grasp balance reaction.2, 7, 10 During unstable stance, it was found in the present study that there was a significant increase of upper back extensor (T4 paraspinal muscle) activity during a forward fall. The T4 surface EMG measured mainly the erector spinae activity, but the cross talk from the rhomboid would not be completely eliminated. The present study also found the early activation of T4 before or at arm release, which might partly be due to a central feedforward command to prepare the guarding of the back muscles before a forward fall.7
Immediately after the arm release from support, there was no significant change in trunk, pelvis, hip and ankle alignment to prevent the forward fall. Therefore, the compensatory mechanism of body mechanical alignment control was impaired in thoracic SCI subjects with complete motor loss and sensory impairment.
During unstable stance, the increase in T4 back extensor activity did not prevent falling, and the rapid reach-and-grasp balance reaction occurred later to bring the COM–COP into a stable condition (that is, a negative value in this study) in the thoracic SCI subjects with KAFOs (Figure 1, Figure 2). According to the biomechanical analysis, the COP must continuously move anterior and posterior to the COM projections on the ground; thus, the dynamic range of the COP must be somewhat greater than that of the COM to prevent a forward or backward fall.6, 9, 21 Therefore, the outreached rapid reach-and-grasp balance reaction increases the base of the COP. It has also been mentioned that during a rapid reach-and-grasp balance reaction with hands on the stable bars, the subject can throw the head backward and push the pelvis forward to prevent the forward fall.2Thus, the rapid reach-and-grasp balance reaction is an important compensatory mechanism.10
The clinical applications of this study are to understand postural control during unstable stance in SCI subjects for standing balance training. The strength of this study is that it used biomechanical and neuromuscular analysis on the issue of postural instability in SCI. The limitation of this study is the small sample size, but nonparametric analysis is used, and the result is acceptable. It is suggested that future studies can be related to the modification of KAFOs for the prevention of falls.
The conclusion of this study is that both back muscle recruitment and the rapid reach-and-grasp balance reaction are important compensatory mechanisms to prevent falling. These can provide therapists or caregivers guidelines for standing balance training in SCI subjects with KAFOs.
References
Lin KH, Lai JS, Kao MJ, Lien IN . Anaerobic threshold and maximal oxygen consumption during arm cranking exercise in paraplegia. Arch Phys Med Rehabil 1993; 74: 515–520.
Somers M . Spinal Cord Injury: Functional Rehabilitation, 2nd edn. Prentice Hall Inc.: New Jersey, 2001.
Middleton JW, Sinclair PJ, Smith RM, Davis GM . Postural control during stance in paraplegia: effects of medially linked versus unlinked knee-ankle-foot orthoses. Arch Phys Med Rehabil 1999; 80: 1558–1565.
Hsiao ET, Robinovitch SN . Common protective movements govern unexpected falls from standing height. J Biomech 1998; 31: 1–9.
Lin KH, Chuang CC, Kao MJ, Lien IN, Tsauo JY . Quality of life of spinal cord injured patients in Taiwan: a subgroup study. Spinal Cord 1997; 35: 841–849.
Winter D . Biomechanics and Motor Control of Human Movement, 3rd edn. John Wiley: New York, 2005.
Shumway-Cook A, Woollacott MH . Motor Control: Translating Research and Clinical Practice, 3rd edn. Lippincott Williams & Wilkins: Philadelphia, PA, 2007.
Horak FB, Dimitrova D, Nutt JG . Direction-specific postural instability in subjects with Parkinson's disease. Exp Neurol 2005; 193: 504–521.
Yang JF, Winter DA, Wells RP . Postural dynamics in the standing human. Biol Cybern 1990; 62: 309–320.
Maki BE, McIlroy WE . The role of limb movements in maintaining upright stance: the ‘change-in-support’ strategy. Phys Ther 1997; 77: 488–507.
Ghafouri M, McIlroy WE, Maki BE . Initiation of rapid reach-and-grasp balance reactions: is a pre-formed visuospatial map used in controlling the initial arm trajectory? Exp Brain Res 2004; 155: 532–536.
Chiu J, Robinovitch SN . Prediction of upper extremity impact forces during falls on the outstretched hand. J Biomech 1998; 31: 1169–1176.
Bengner U, Johnell O . Increasing incidence of forearm fractures. A comparison of epidemiologic patterns 25 years apart. Acta Orthop Scand 1985; 56: 158–160.
Kirshblum SC, Memmo P, Kim N, Campagnolo D, Millis S . Comparison of the revised 2000 American Spinal Injury Association classification standards with the 1996 guidelines. Am J Phys Med Rehabil 2002; 81: 502–505.
Maynard Jr FM, Bracken MB, Creasey G et al. International standards for neurological and functional classification of spinal cord injury. American spinal injury association. Spinal Cord 1997; 35: 266–274.
Gregson JM, Leathley M, Moore AP, Sharma AK, Smith TL, Watkins CL . Reliability of the tone assessment scale and the modified ashworth scale as clinical tools for assessing poststroke spasticity. Arch Phys Med Rehabil 1999; 80: 1013–1016.
Jeka JJ, Lackner JR . Fingertip contact influences human postural control. Exp Brain Res 1994; 100: 495–502.
Matjacic Z, Bajd T . Arm-free paraplegic standing—Part II: experimental results. IEEE Trans Rehabil Eng 1998; 6: 139–150.
Ferris DP, Czerniecki JM, Hannaford B . An ankle-foot orthosis powered by artificial pneumatic muscles. J Appl Biomech 2005; 21: 189–197.
Matjacic Z, Hunt K, Gollee H, Sinkjaer T . Control of posture with FES systems. Med Eng Phys 2003; 25: 51–62.
Winter DA, Patla AE, Prince F, Ishac M, Gielo-Perczak K . Stiffness control of balance in quiet standing. J Neurophysiol 1998; 80: 1211–1221.
Acknowledgements
We thank Mr Chia-Chieh Chang for the electromyographic data analysis. This study was funded by the National Science Council, Taipei, Taiwan, ROC (NSC 92-2314-B-002-113).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, KH., Lu, TW., Hsu, PP. et al. Postural responses during falling with rapid reach-and-grasp balance reaction in patients with motor complete paraplegia. Spinal Cord 46, 204–209 (2008). https://doi.org/10.1038/sj.sc.3102100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102100