Abstract
Study design:
Short communication.
Objectives:
To report a case with bilateral lower extremity complex regional pain syndrome (CRPS) in a patient with paraplegia occurring following spinal disc herniation surgery, who was treated successfully with pulse radiofrequency (PRF) lumbar sympatholysis.
Setting:
Departments of Physical Medicine and Rehabilitation, Algology Department of Anaesthesiology and Nuclear Medicine, Medical Faculty of Ege University, Izmir, Turkey.
Methods:
A 55-year-old woman had neuropathic pain in her lower extremities after T12–L1 disc herniation surgery. The pain decreased to a tolerable level with conservative treatment and her condition remained stable for the following 6 months; then she developed swelling, redness and severe burning pain in both feet. Physical examination showed edema and redness in the feet. On the basis of clinical findings and Tc-99m methylene diphosphonate (MDP) three-phase bone scintigraphy, she was diagnosed to have CRPS.
Results:
The patient underwent a diagnostic sympathetic ganglion blockade with bupivacaine, which resulted in a marked decrease in the pain and edema of the feet. Consequently, PRF lumbar sympatholysis was performed with a successful outcome in pain, edema and color changes in the feet.
Conclusion:
When treatment of CRPS fails with conventional modalities, PRF sympatholysis may be used for control of pain and other symptoms in such patients.
Similar content being viewed by others
Introduction
Although chronic pain is a common secondary complication of spinal cord injury (SCI), CRPS associated with SCI has been reported relatively rarely, mainly in the form of case reports.1, 2, 3, 4 Treatment of CRPS is both controversial and challenging. Pulsed radiofrequency (PRF) treatment is a relatively new technique that has been reported to be used for the treatment of CRPS in anecdotal cases 5.
Herein, we report a patient who developed clinical findings compatible with a diagnosis of CRPS, 6 months after a T12–L1 disc herniation surgery, which was complicated by SCI. The patient was treated successfully with PRF lumbar sympatholysis.
Case report
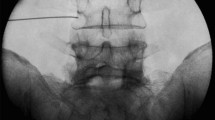
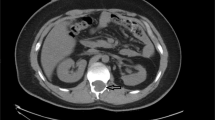
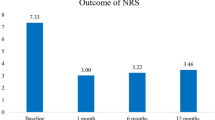
A 55-year-old woman had undergone T12–L1 disc herniation surgery, which was complicated by SCI. She was admitted to the Department of Physical Medicine and Rehabilitation for the treatment of paraplegia and severe neuropathic pain after this operation. Her condition remained stable with gabapentin (1200 mg/day) and tramadol (150 mg/day) for the next 6 months, and then she developed redness, swelling and severe burning and stabbing pain in both feet, more pronounced on the right side. X-rays of both ankles were obtained, which revealed diffuse osteopenia bilaterally. Tc-99m methylene diphosphonate (MDP) three-phase bone scintigraphy (TPBS) was performed, which showed increased regional blood flow and hyperactivity in both ankles with a more remarkable pattern on the right side (Figure 1). The doses of gabapentin and tramadol were increased. Despite this treatment pain could not be controlled adequately, and diagnostic lumbar sympathetic ganglion block was performed with bupivacaine, which led to clear improvement in pain intensity. Consequently, PRF lumbar sympatholysis was performed9, 10 unilaterally on the right side at L2, L3 and L4 levels under CT fluoroscopy guidance. PRF was applied at 42°C for 240 s using a 20-gauge, 150 mm radiofrequency (RF) needle with 10 mm active tip. Low-voltage sensory stimulation was performed up to 1 V at 50 Hz to ensure that stimulation reproduced concordant pain. Sensory stimulation ranged from 0.2 to 0.5 V at 50 Hz. The intensity and unpleasantness of pain were evaluated by visual analog scale (VAS). We used a brush to evaluate mechanical allodynia/hyperalgesia. Brush-evoked pain tested in the maximal pain area before and after this procedure. Pain on VAS (0–100; 0: no pain, 100: worst possible pain) decreased from 95 to 45 mm on the 5th day and to 25 mm on the 10th day, and edema and color changes in the feet disappeared within 3 days following the PRF-lumbar sympatholysis treatment. The changes in hyperalgesia and allodynia sensation were similar to the change in pain intensity. Clinical improvement remained stable over the follow-up of 4 months. Moreover, she did not require tramadol 4 months following PRF sympatholysis and pain measured according to VAS did not exceed 40 mm.
Discussion
The treatment of CRPS is more challenging than its diagnosis. Only a few randomized, placebo-controlled studies are available and individual response to different treatments may vary. However, experts agree that the most appropriate management should be based on a multidisciplinary approach.6, 7 Management of CRPS includes any combination of pharmacotherapy, physical and occupational therapy, regional anesthetic blocks, behavioral therapies, and surgery. Although the role of sympathectomy in the treatment of CRPS is controversial, it can be used in refractory cases. If conservative medical treatment does not provide adequate analgesia, regional anesthetic blockade may be necessary as a diagnostic and prognostic procedure7 and lumbar sympatholysis can be performed if patients have responded well to the initial sympathetic block.8 Use of RF treatment for the purpose of sympathetic blockade has the advantage over surgical resection, phenol or alcohol neurolysis because of being more selective and thus causing fewer complications.9 PRF is a relatively new technique where short bursts of RF energy are applied to nerve tissue. It is suggested to be a minimally neurodestructive alternative to RF heat lesions, because of a potentially better risk/benefit ratio5. However, clinical advantages and mechanisms of this treatment are still unclear.
In none of the published reports, neurological side effects or complications with PRF have been mentioned5, but it should certainly share some of the complications of conventional PRF such as epidural, subdural, or subarachnoid injection and trauma to the intervertebral disc, spinal cord and exiting nerve roots due to needle misplacement as well as infection.10 In our patient, PRF lumbar sympatholysis was performed after a good response to lumbar sympathetic ganglion block with bupivacaine, with significant reduction of pain and improvement of edema without any complication. The dramatic reduction in pain from 95 to 25 mm was not maintained and it increased from 25 to 40 mm during a follow-up of 4 months. It has been suggested that the acute effects of PRF are more reversible and less neurodestructive in nature than the classic continuous RF mode. Thus pain relief can last for several months and procedure needs to be repeated in most cases. However, the long-term efficacy in our patient still remains to be seen.
In conclusion, when adequate control of pain and other symptoms cannot be achieved with physical and pharmacologic therapy in patients with CRPS, a good clinical response may be obtained with PRF sympatholysis.
References
Gellman H, Eckert RR, Botte MJ, Sakimura I, Waters RL . Reflex sympathetic dystrophy in cervical spinal cord injury patients. Clin Orthop Relat Res 1988; 233: 126–131.
Gallien P, Nicolas B, Robineau S, Lebot MP, Brissot R . The reflex sympathetic dystrophy syndrome in patients who have had a spinal cord injury. Paraplegia 1995; 33: 715–720.
Lefkoe TP, Cardenas DD . Reflex sympathetic dystrophy of the lower extremity in tetraplegia: case report. Spinal Cord 1996; 34: 239–242.
Sutbeyaz ST, Koseoglu BF, Yesiltepe E . Simultaneous upper and lower extremity complex regional pain syndrome type I in tetraplegia. Spinal Cord 2005; 43: 568–572.
Cahana A, Van Zundert J, Macrea L, van Kleef M, Sluijter M . Pulsed radiofrequency: current clinical and biological literature available. Pain Med 2006; 7: 411–423.
Yung Chung O, Bruehl SP . Complex regional pain syndrome. Curr Treat Options Neurol 2003; 5: 499–511.
Rho RH, Brewer RP, Lamer TJ, Wilson PR . Complex regional pain syndrome. Mayo Clin Proc 2002; 77: 174–180.
Sharma A, Williams K, Raja SN . Advances in treatment of complex regional pain syndrome: recent insights on a perplexing disease. Curr Opin Anaesthesiol 2006; 19: 566–572.
Van Zundert J, Raj P, Erdine S, van Kleef M . Application of Radiofrequency Treatment in Practical Pain Management: State of the Art. Pain Pract 2002; 2: 269–278.
Waldman S . Lumbar sympathetic ganglion block: radiofrequency lesioning. In: Atlas of Interventional Pain Management. Saunders: Philadelphia, 2004, pp 313–315.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akkoc, Y., Uyar, M., Oncu, J. et al. Complex regional pain syndrome in a patient with spinal cord injury: management with pulsed radiofrequency lumbar sympatholysis. Spinal Cord 46, 82–84 (2008). https://doi.org/10.1038/sj.sc.3102074
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102074
Keywords
This article is cited by
-
Interventional Radiofrequency Treatment for the Sympathetic Nervous System: A Review Article
Pain and Therapy (2021)
-
Transferrin as a thermosensitizer in radiofrequency hyperthermia for cancer treatment
Scientific Reports (2018)
-
Association between extracellular signal-regulated kinase expression and the anti-allodynic effect in rats with spared nerve injury by applying immediate pulsed radiofrequency
BMC Anesthesiology (2015)
-
Is section of the sympathetic rami communicantes by laparoscopy in patients with refractory low back pain efficient?
European Spine Journal (2013)