Abstract
Study design:
A case report.
Setting:
Urodynamic laboratory in a university hospital, Chiba, Japan.
Case report:
A young woman who suffered from urinary retention following a skiing accident. A sacral X-ray (lateral view) revealed an S2–3 sacral fracture. The patient gradually regained the ability to urinate. At 3 months after the accident, she still suffered difficult urination, although her neurological findings were normal. A urodynamic study showed an acontractile detrusor and a neurogenic sphincter electromyogram (EMG), together indicative of isolated sacral nerve injury.
Conclusions:
It was postulated that the S2–3 sacral fracture had led to bilateral traction of the S2–3 nerve roots, producing transient bladder paralysis (parasympathetic fibers) and incomplete sphincter paresis (somatic fibers). Sacral fracture is also of high clinical suspicion for urinary retention in frail elderly people, because it can result from simple falls.
Similar content being viewed by others
Introduction
The bladder and sphincter are innervated by the spinal conus, which is located at the L1 vertebra. The sacral and lumbar roots bundle together, forming the cauda equina, and the S2–3 sacral roots then separate and run through the sacral foramina. Isolated sacral root injury is thought to be rare. It may occur in the vertebral canal due to central lumbar disc prolapse1 and lumbar spondylosis,2 or at the sacral foramina due to sacral fracture.3, 4 We recently examined a patient who suffered from urinary retention due to isolated sacral root injury after a skiing accident.
Case report
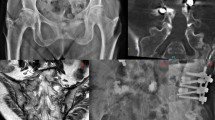
A healthy 29-year-old woman bumped another person, fell and collided with a hedge while skiing. She developed severe buttock pain and was admitted to a local orthopedic surgery hospital where she was diagnosed, based on X-ray examination, with an isolated S2–3 sacral fracture (Figure 1). Closed reduction was performed and an indwelling urinary catheter was inserted. The patient’s buttock pain ameliorated gradually. However, on day 16, after the catheter was removed, she was in a state of urinary retention; she also reported numbness in the perineal area (sensation of traction around the anus) and constipation. She was taught to perform clean intermittent self-catheterization (CISC) and was given 30 mg/day of urapidil, an α-adrenergic antagonist. The patient gradually regained the ability to urinate, and on day 45, CISC was stopped. On day 90, she was referred to our urodynamic laboratory because she still suffered difficult urination and slight urinary incontinence.
Upon referral, the patient had normal muscle power and deep tendon reflexes in the lower extremities, as well as normal perineal sensation. A pelvic autonomic questionnaire5 showed high frequency in daytime urination (9 times), urinary incontinence (unwittingly, monthly), prolongation (weekly), intermittency (daily), and straining (daily), as well as normal bowel frequency (once a day, but laxatives always necessary), difficult defecation (daily), fecal incontinence (monthly), and decreased sexual intercourse (mildly) and decreased orgasm (mildly), indicating neurogenic bladder, bowel, and sexual dysfunction. A urodynamic study6 (Urovision, Lifetec, Inc., Houston, TX, USA; Neuropack Sigma, Nihon Kohden, Inc., Tokyo, Japan) was performed under urapidil administration to measure post-void residual volume and medium-fill (50 ml/min) water cystometry. Simultaneously, sphincter electromyography (EMG) was carried out using a concentric needle electrode in the external anal sphincter muscles. The patient had a post-void residual volume of 70 ml (normal <30). Normal volumes were observed at the first sensation of the bladder filling, that is, a volume of 256 ml (100<normal<300), but the patient had an increased bladder capacity of more than 600 ml (200<normal<600) during the storage phase. Water infusion was stopped in order to avoid an overdistention bladder injury. There was no evidence of low-compliance detrusor. During the voiding phase, the patient showed an acontractile detrusor without urinary flow, whereas the sphincter EMG sound disappeared completely; this was followed by considerable straining during the voiding phase. Analysis of motor unit potentials (MUPs) in the sphincter muscles showed a neurogenic change (normal mean duration, 9.34 ms; but 50% of MUP with a duration of more than 10 ms, normal <20%).7 Two months after the urodynamic assessment, although still under urapidil treatment, her difficult urination continued to ameliorate gradually.
Discussion
Neurological deficits associated with sacral fractures are a rare but well-documented condition.4, 8, 9, 10, 11 Sacral fractures typically present with cauda equina syndrome, for example, numbness and loss of pain sensation in the saddle region, decreased Achilles tendon reflexes, together with pelvic autonomic dysfunction such as bladder, bowel, and sexual dysfunction. Bladder dysfunction presents with bladder paralysis.11 Our patient suffered from urinary retention after a skiing accident. Her neurological symptoms in the acute phase, plain X-ray examination, a urodynamic study, and sphincter EMG indicated an isolated sacral root injury due to an S2–3 sacral fracture. After reduction of the fracture and urapidil administration, the patient’s urinary retention gradually ameliorated over a period of 3 months. This condition is thought to be rare, because the estimated incidence of isolated sacral fracture is 0.16–2%.12, 13 However, the incidence can be higher in older people, with most cases experiencing local pain alone.14, 15 Even if neurological manifestations are present, they may be overlooked due to various degrees of pain.15
To the best of our knowledge, there have been few previous reports on urodynamic studies in sacral fracture.3, 4 Fountain et al3 report six cases of sacral fracture; in two of these, cystometry was performed, revealing acontractile detrusor (details not known). Both patients underwent sacral laminectomy, and urinary retention ameliorated after 5 weeks in one case and after 5 months in the other. Additionally, Reynier et al4 report two cases of sacral fractures; however, one of these patients also had a lumbar compression fracture at the L2 level and the other had fractures of the ilium and ischiopubic rami. Sphincter EMG showed neurogenic change in both patients. Cystometry was performed on the former, showing bladder sensation only at 800 ml (details not known). The patient underwent sacral laminectomy, and urinary retention gradually ameliorated.
The results of the present study (acontractile detrusor and neurogenic sphincter EMG) are consistent with those in the previous reports.3, 4 All of the present findings can be regarded as the results of the patient's S2–3 sacral fracture, which is believed to have led to bilateral traction of the S2–3 nerve roots, producing transient bladder paralysis (parasympathetic fibers) and incomplete sphincter paresis (somatic fibers). Sacral fracture may also occur after simple falls.14, 15 Therefore, sacral fracture should be considered with high clinical suspicion when we see frail elderly women with urinary retention.16
Conclusions
We have reported the case of a young woman with urinary retention due to an isolated sacral root injury caused by an S2–3 sacral fracture. Sacral fracture is also of high clinical suspicion for urinary retention in frail elderly people, because it can result from simple falls.
References
Yamanishi T et al. The urodynamic evaluation of surgical outcome in patients with urinary retention due to central lumbar disc prolapse. Neurourol Urodynam 2002; 21: 425.
Sakakibara R et al. Is lumbar spondylosis a cause of urinary retention in elderly women? J Neurol 2005; 252: 953–957.
Fountain SS, Hamilton RD, Jameson RM . Transverse fractures of the sacrum. A report of six cases. J Bone Joint Surg Am 1977; 59: 486–489.
Reynier Y, Grisoli F, Delarque A, Vigouroux RP . Fracture dislocation of the sacral spine with cauda equina lesion. Report of two cases. Neurochirurgie 1982; 28: 25–32 (in French with English abstract).
Sakakibara R et al. Questionnaire-based assessment of pelvic organ dysfunction in Parkinson’s disease. Auton Neurosci Basic Clin 2001; 92: 76–85.
Abrams P et al. The standardization of terminology of lower urinary tract function: report from the standardization sub-committee of the international continence society. Neurourol Urodynam 2002; 21: 167–178.
Podner S, Fowler CJ . Sphincter electromyography in diagnosis of multiple system atrophy: technical issues. Muscle Nerve 2004; 29: 151–156.
Goodell CL . Neurological deficit associated to pelvic fractures. J Neurosurg 1966; 24: 837–842.
Dewey P, Browne PSH . Fractures and dislocation of the lumbosacral spine with cauda equine lesion. J Bone Joint Surg Br 1968; 50: 635–638.
Fardon DF . Displaced fractures of the lumbosacral spine with delayed cauda equine deficit. Clin Orthop 1976; 120: 155–158.
Pavlakis AJ . Cauda equine and pelvic plexus injury. In: Krane RJ, Siroky MB (eds). Clinical Neuro-urology. Boston: Little Browon 1991, pp 333–334.
Hart DJ, Wang MY, Griffith P, Gordon McComb JG . Pediatric sacral fractures. Spine 2004; 29: 667–670.
Gibbons KJ, Soloniuk DS, Razack N . Neurological injury and patterns of sacral fractures. J Neurosurg 1990; 72: 889–893.
Weber M, Hasler P, Gerber H . Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine 1993; 18: 2507–2512.
Finiels PJ, Finiels H, Strubel D, Jacquot JM . Spontaneous osteoporotic fractures of the sacrum causing neurological damage. Report of three cases. J Neurosurg 2002; 97 (3 Suppl): 380–385.
Taillandier J, Langue F, Alemanni M, Taillandier-Heriche E . Mortality and functional outcomes of pelvic insufficiency fractures in older patients. Joint Bone Spine 2003; 70: 287–289.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sakakibara, R., Uchiyama, T., Yamaguchi, C. et al. Urinary retention due to an isolated sacral root injury caused by sacral fracture. Spinal Cord 45, 790–792 (2007). https://doi.org/10.1038/sj.sc.3102058
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102058