Abstract
Study design:
Case report.
Objectives:
To describe a rare case of oncocytoma arising from the spinal cord in a 40-year old woman.
Setting:
Republic of Korea.
Methods:
The patient's history, physical examination, radiological and pathological findings were reviewed.
Results:
A 40-year-old woman presented with 3-month history of low back pain. Magnetic resonance imaging revealed an intradural extramedullary mass located between L1 and L4. She refused any surgical treatment and so was discharged. At 10 days after discharge, an emergency operation was performed because of sudden paralysis in both lower extremities. The confirmed diagnosis is oncocytoma. At 4 months after surgery, the patient failed to obtain neurological recovery from complete paraplegia.
Conclusions:
Since the progression of an intradural extramedullary mass that shows minor neurological symptoms can lead to complete paraplegia in a short time, close observation and early surgical decompression are necessary.
Similar content being viewed by others
Introduction
Oncocytoma is a tumor predominantly or exclusively composed of oncocytes, defined morphologically as plump polygonal cells with abundant eosinophilic granular cytoplasm, and these cells are believed to represent a degenerative or aging process of various cells.1, 2, 3, 4 Oncocytomas occur in many organs, including kidneys, salivary glands, pituitary gland, thyroid gland, parathyroid glands and breast tissue.4, 5 However, the incidence of the tumor in the spinal cord is extremely rare with only two similar cases having been reported to date.6, 7 Contrary to the favorable neurological prognosis those two cases experienced, the authors here report a case of oncocytoma of the spinal cord, which rapidly progressed to paraplegia within 10 days from the day of the diagnosis was made, following the mild clinical symptoms presented for about 3 months.
Case report
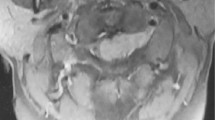
This was a 40-year old woman suffering from low back pain and bilateral sciatica, and had been treated with combination of medication and physical therapy at a local orthopedic clinic over the past 3 months prior to the admission. She stated the therapy only gave her some temporary relief of her symptoms. She came to our hospital because she had noticed some gait disturbance for the last 1 month. The physical examination of her lower extremities showed the following on the left/right side: straight leg-raising test, 70°/60°; motor power of key muscles in lower extremities, normal/normal; patellar tendon reflex, decreased/decreased; and ankle jerk, decreased/decreased. No changes were observed in the sensory nerve function. Plain radiograms did not reveal any specific finding, but the sagittal magnetic resonance (MR) image showed an intradural extramedullary mass extending from the lower portion of the L1 body to the upper portion of the L4 body. It showed low signal density on T1- and T2-weighted images, whereas the postcontrast T1-weighted sagittal MR image showed a slight enhancement (Figure 1). The axial MR image at the L2 body level showed an enlarged canal due to a space occupying mass. We recommended decompressive laminectomy with mass excision, but she adamantly refused any surgical treatment at that point. At 10 days after her discharge, she returned to the emergency room complaining of paralysis in her both lower extremities. On physical examination, there was complete motor paraplegia of both lower extremities, anesthesia under the L1 dermatome and no bladder and bowel function. She stated the night before she came to the ER, she suddenly found herself unable to move her lower limbs. We performed emergency operation of decompressive laminectomy, mass excision, L1-3 pedicle screw augmentation and posterolateral fusion using autogenous iliac cancellous and laminectomized bone. At the operation, a black-colored mass was found in the dural sac in the L1-4 area (Figure 2). Histological examination revealed tumor cells arranged in sheets or in thick cords, consisting of polygonal, well-demarcated cells with variation in nuclear size and number, inconspicuous nucleolus, and abundant, homogenously eosinophilic granular cytoplasm (Figure 3). Periodic acid–Schiff stain and Fontana Masson stain were negative in all cells. The immunohistochemical stains for vimentin, epithelial membrane antigen (EMA), glial fibrillary acidic protein (GFAP), CK7, CK20 and CD68 were all positive, while the stains for myoglobin, desmin, actin, S-100 protein and chromogranin were all negative. Notably, the immunohistochemical stain for HMB-45 was positive (Figure 4). Ultrastructurally, the cytoplasm of the tumor cells showed densely packed mitochondria, a number of which possessed stacked lamellar cristae (Figure 5). Melanosomes were not identified. On the basis of these clinical and pathological findings, we diagnosed this case as an oncocytoma arising from the spinal cord.
After 4 months post-operatively, a repeated physical examination was performed and revealed no signs of recovery of motor or sensory function of the extremities.
Discussion
Oncocytes are plump polygonal cells characterized histologically by abundant eosinophilic granular cytoplasm and are found in a variety of normal and pathological conditions including neoplasms.4, 5, 8, 9 Their identity can be confirmed by the immunohistochemical demonstration of increased cytoplasmic mitochondrial antigens using an antimitochondrial antibody,10 as well as by the electron microscopic feature of innumerable mitochondria packed within the abundant cytoplasm.
The pathogenesis of oncocytic changes or oncocytoma is thought to be the result of aberrant metaplastic change that occurs in the situations of cellular stress.1, 2, 3, 4 As mitochondria are the most important organelle in cellular metabolism, injury to the mitochondria may result in the compensatory proliferation of mitochondria and cellular swelling. Ultrastructural studies have shown that those abundant mitochondria are often abnormal, that is, many of them are swollen with abnormally shaped and disrupted cristae.11, 12
Oncocytoma has to be differentiated from oncocytic meningioma, granular cell tumor and paraganglioma because these tumors may also show polygonal cells with abundant eosinophilic cytoplasm. Roncaroli et al13 reported six cases of oncocytic meningioma that showed clear-cut meningothelial features such as whorls, hyalinized vessels and occasional psammomatous bodies as well as other features of meningothelial differentiation such as cytoplasmic interdigitations and desmosomes on ultrastructural study. However, our case did not display the microscopic or ultrastructural features of meningothelial differentiation. For the granular cell tumors, they would typically reveal positive granules on periodic acid-Schiff stain and show lysosome-rich cytoplasm on ultrastructural study,14 but our case did not. Paraganglioma can be differentiated by its distinctive trabecular or organoid pattern, the immunoreactivity for S-100 protein and chromogranin, and neurosecretory granules noted in the ultrastructural study.15, 16
As shown in the report of Gelman et al,6 our case also showed positive reaction to the immunostaining for HMB-45, suggesting its melanocytic differentiation. But the diagnosis of melanocytoma was ruled out by using several other differential criteria including negative staining for Fontana Masson and immunostaining for S-100 protein, a marker that is present in melanocytes, absence of prominent nucleolus as well as brown pigments in H&E stain and no melanosomes in EM. A further accumulation of studies on similar cases will be necessary to clarify the nature of this tumor more.
There are very few studies or reports made in the medical literature on oncocytomas occurring in the spinal cord, and to date, only two cases have been reported in the English literature.6, 7 As shown in those previous reports,6, 7 both cases showed complete neurological recoveries without recurrence of symptoms after surgical treatment, and emergency surgery was not necessary since the postoperative outcome was relatively satisfactory. Furthermore, in one case,6 a surgical treatment was performed after 25 years of observation, showing an example of how slow the natural course of the tumor can be. In our case, however, from the day when the tumor was discovered by the spinal stenosis and radiculopathy on the radiological study, following the initial symptoms, and to the development of the complete paraplegia, it took only 10 days. We postulated that such rapid neurological progress might have been caused by complete damage of the spinal cord when the blood circulation of the anterior spinal artery was completely cut off by the mass, which was compressing the spinal cord against the canal wall.
In conclusion, it is important to recognize the fact that oncocytoma may occur in the spinal cord, despite the general belief that it is an extremely rare location, and this tumor can present with rapid progression into overt neurological manifestations. Therefore, however, minimal or negligible symptoms an intradural extramedullary mass may present initially, a close observation of these tumors is necessary in readiness for an early intervention or a measure of decompression when it is needed.
References
Stump DJ . Onkocytic adenoma of the salivary gland. Arch Pathol 1949; 48: 287–296.
Hamperl H . Beiträge zur normalen und pathologischen histologie menschlicher speicheldrüsen. Ztschr Mikrosk Anat Forsch 1931; 21: 1–55.
Hamperl H . Onkocyten und onkocytome. Virch Arch A Pathol Anat Histopathol 1962; 335: 452–483.
Hamperl H . Benign and malignant oncocytoma. Cancer 1962; 15: 1019–1027.
Cotton DW . Oncocytomas. Histopathology 1990; 16: 507–509.
Gelman BB et al. Oncocytoma in melanocytoma of the spinal cord: case report. Neurosurgery 2000; 47: 756–759.
Kim SH et al. Oncocytoma of the spinal cord. Case report. J Neurosurg 2001; 94: 310–312.
Hübner G, Paulussen F, Kleinssasser O . Zur Feinstruktur und Genese der Onkocyten. Virchows Arch A 1967; 343: 34–50.
Chang A, Harawi SJ . Oncocytes, oncocytosis, and oncocytic tumors. Pathol Annu 1992; 27: 263–304.
Papotti M et al. Immunohistochemical identification of oxyphilic mitochondria-rich cells. Appl Immunohistochem 1994; 2: 261–267.
Kobayashi H, Hosino M, Tauchi H . Ultrastructural study of cytochrome oxidase in oncocytoma. Nagoya J Med Sci 1972; 35: 25–32.
Goebel HH, Schulz F, Rama B . Ultrastructurally abnormal mitochondria in the pituitary oncocytoma. Acta Neurochir 1980; 51: 195–201.
Roncaroli F et al. Oncocytic meningioma. Am J Surg Pathol 1997; 21: 375–382.
Liwnicz BH et al. Ciant granular cell tumor of the suprasellar area: immunohistochemical and electron microscopic studies. Neurosurgery 1984; 15: 246–251.
Lack EE . Paragangliomas. In: Sternberg SS, Antoniolli DA, Carter D, Mills SE, Oberman HA (eds). Diagnostic Surgical Pathology, 3rd edn. LWW 1999, pp 625–648.
Moran CA, Rush W, Mena H . Primary spinal paragangliomas: a clinicopathological and immunohistochemical study of 30 cases. Histopathology 1997; 31: 167–173.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Park, H., Jang, K., Kang, M. et al. Oncocytoma of the spinal cord causing paraplegia – a case report. Spinal Cord 45, 183–186 (2007). https://doi.org/10.1038/sj.sc.3101905
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101905
Keywords
This article is cited by
-
Spinal adrenal cortical adenoma associated with Beckwith-Wiedemann syndrome: case report and review of the literature
Child's Nervous System (2017)
-
Symptomatic Intraspinal Oncocytic Adrenocortical Adenoma
Endocrine Pathology (2009)