Abstract
Study design:
A case report of primary osteosarcoma of the spine in an elderly patient.
Objective:
The histopathological features of osteosarcoma vary widely, often leading to diagnostic difficulties particularly when there is little evidence of osteoid formation. The report describes the difficulty in the diagnosis of osteosarcoma of the thoracic vertebra.
Setting:
Department of Orthopaedics and Rehabilitation Medicine, Fukui University Faculty of Medicine, Fukui, Japan.
Method:
A 78-year-old man presented with paraparesis and underwent urgent anterior excision of a primary spinal tumor emanating from the T10 vertebra followed by artificial vertebral replacement. The patient eventually died of disseminated disease of vertebral osteosarcoma.
Results:
Samples from the T10 vertebral tumor showed neoplastic growth of atypical spindle-shaped cells, with foci of storiform-like proliferation. The tissue also demonstrated positive immunohistochemical staining for vimentin and α-smooth muscle actin and a tentative diagnosis of leiomyosarcoma was made. However, a metastatic nodule of the chest wall at autopsy showed focal osteoid formation, a finding not seen in the primary tumor.
Conclusion:
Early detection and accurate diagnosis is important for improving not only patient prognosis but also the quality of life. We should always consider this rare entity, particularly in elderly patients who present with back pain and vertebral collapse.
Similar content being viewed by others
Introduction
Primary osteosarcoma of the spine is a rare condition accounting for 3.7–14.5% of primary spinal tumors1, 2 and 0.4–2.7% of all osteosarcomas.3, 4, 5, 6 Osteosarcoma is a malignant bone tumor that frequently affects patients in their second and third decades of life, however, it is reported there exists two peaks in the incidence of osteosarcoma, one is in the second decade and another in the seventh decade of life.7 Huvos8 reported three cases of osteosarcoma of the spine among 117 patients with osteosarcoma older than 60 years. Histopathologically, the diagnosis of osteosarcoma may be difficult especially when the tumor presents with an extensive fibrohistiocytic storiform pattern, infiltration of atypical spindle cells, and minimal or scarce osteoid formation.9
This short communication describes an elderly man with paraparesis caused by a solitary primary vertebral tumor at T10 vertebral level, which was finally diagnosed as osteosarcoma at autopsy. Histopathological examination of the tumor at surgery, 5 months prior to death showed histological features suggestive of leiomyosarcoma.
Case report
The patient, a 78-year-old previously healthy man, initially complained of intractable back pain following a minor fall 4 months prior to admission. The pain gradually worsened and the patient had difficulty in walking for 1 week prior to referral to our hospital.
On admission, the patient was noted to have paraparesis (Frankel-ASIA grade B scale) below the level of T9, with sensory deficit in the lower extremities and bladder dysfunction. Blood tests were normal. Radiographs demonstrated a collapsed T10 vertebra with evidence of decreased radiolucency, suggestive of a vertebral malignancy (Figure 1a). The lesion showed a decreased intensity signal on a T1-weighted magnetic resonance image and an irregular high-intensity signal on a T2-weighted image (Figure 1b). Skeletal surveys, which included 99mTc bone scintigraphy, were normal apart from the T10 vertebral body lesion. Furthermore, regional surveys, including brain, chest, and abdominal CT and gastrointestinal endoscopy, were also normal.
The patient underwent an anterior resection of the T10 vertebra (through a left-sided transthoracic approach) with replacement by an artificial vertebra (LIFT vertebral body®; Sofamore-Danek, Paris, France) in conjunction with LD instrumentation® (Sofamore-Danek), consisting of screws and plate system for stabilizing the vertebrae after complete resection of the tumor as well as excellent spinal cord resection. At surgery, the tumor had a yellowish or gray-brown appearance. There was no evidence of excessive hemorrhage during resection of the tumor. Histopathological examination of a frozen section obtained intraoperatively from the resected tumor showed features suggestive of a high-grade sarcoma, probable leiomyosarcoma.
Postoperatively, the patient became ambulatory with use of a single cane (Frankel-ASIA grade D scale), even though the spasticity of the legs did not show any improvement. The patient refused chemotherapy consisting of a high-dose methotrexate and cis-platinum as well as radiotherapy. The patient died 8 months after the surgery due to disseminated pulmonary disease.
Histopathological, immunohistochemical, and autopsy findings
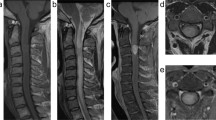
Histological examination of the tumor samples obtained from both surgery and autopsy showed that they consisted of infiltrates of atypical pleomorphic spindle-shaped cells with eosinophilic cytoplasm. Foci of storiform-like cellular proliferation and abnormal mitoses were seen in the samples obtained at surgery (Figure 2a). The majority of tumor cells stained positive for vimentin and α-smooth muscle actin (Figure 2b) by immunohistochemistry. Some tumor cells were immunohistochemically positive for HHF35 and desmin but all cells were negative for S-100 protein, keratin, epithelial membrane, and CD-34 antigens.
Histopathological and immunohistochemical examinations. (a) The primary tumor (T10 vertebral body) consists of spindle-shaped cells in a storiform pattern. No osteoid formation is seen. (b) Cells of the primary tumor stain diffusely positive for α-SMA (arrows). (c) Chest wall dissemination at autopsy. Osteoid formation is evident, with calcification of some areas (arrows) (Magnification × 120 (a, c), × 240 (b))
At autopsy, the tumor surrounded the seated artificial vertebra and involved the adjacent pleura. Multiple disseminated and/or metastatic lesions were observed in the left chest wall and in the vicinity of the descending aorta. Multiple metastatic masses were also present in the lung bilaterally and in the liver. There was no macroscopic evidence of tumor in the remaining viscera including the musculo-skeletal system.
Although osteoid formation was not evident in the vertebral tumor resected 5 months earlier, a nodule excised from the left chest wall at autopsy demonstrated areas of osteoid formation both with and without calcification (Figure 2c). Both the tumor cells surrounding and those within the osteoid areas stained positive for vimentin, α-smooth muscle actin, and HHF35, indicating that the tumor was an osteosarcoma, with fibroblastic features.
Discussion
Immediate surgical decompression is a crucial therapy in acute paraplegia caused by tumor-related spinal cord compression, as it may restore or preserve gait function and improve the quality of life. During adulthood, neural tissue has less capacity for neuronal plasticity, although plastic changes may be found at any age,10 in which spinal cord morphological plasticity correlates with neurological function.11 In the presence of complete paralysis before the operation, surgical treatment does not produce any essential improvement apart from pain relief, however, neurological improvement tends to be provided by immediate decompression in case of paresis.12, 13 Accordingly, in our case, the patient showed improvement of neurological deficits, although he underwent operation 1 week after the onset of paresis. Thus, these results confirm that early diagnosis is important for better neurological improvement in patients with paresis caused by tumor-related spinal cord compression.
Local recurrence of the spinal tumor causes paralysis, and influences mortality. Talac et al14 described in their study of spinal sarcomas that residual tumor at the surgical margin, and resection in a piecemeal fashion, resulted in a high recurrence rate that was associated with early mortality. Similarly, a recent review of 1702 patients with high-grade osteosarcoma5 indicated that failure to achieve a surgical remission of osteosarcoma was associated with increased age, axial site, long history, delayed start of therapy, intralesional surgical resection, and poor response to chemotherapy. However, Gore et al15 reported a case with long-term survival after intralesional resection of thoracic spine osteosarcoma with multidisciplinary, multimodal approach, using aggressive chemoradiotherapy with surgical resection. They applied chemotherapy preoperatively, which consisted of high-dose methotrexate, cisplatin, doxorubicine, ifosfamide, and muramyl tripeptide phosphatidyl ethanolamine. Subsequently, during the planned intralesional tumor resection, a total of 47 125I-impregnated seeds were placed along the area of residual tumor. Postoperatively, they performed external beam radiation and provided additional chemotherapy. The response rate of fibroblastic osteosarcoma to chemotherapy was reported to be more than 40%.16, 17 In addition, Ozaki et al6 reported that postoperative radiotherapy improved the survival rate in patients with osteosarcoma. In our case with a final diagnosis of fibroblastic osteosarcoma, the prognosis might have improved had the patient agreed on chemotherapy and/or radiotherapy. In addition, there was a problem with respect to establishing a definitive postoperative diagnosis.
Histopathologically, osteosarcoma usually rests on the presence of malignant tumor; osteoid and/or bone production within the tumor. However, in elderly patients, the diagnosis of osteosarcoma may be difficult because of its histological features. Huvos8 indicated that osteosarcoma of elderly patients may often present with fibrohistiocytic and fibrous variants. One variant may show little osteoid formation, as suggested by Campanacci and Enneking,9 indicating that the tumor specimen should be carefully examined if this diagnosis is suspected. In such instances, they indicated that it might be difficult and subjective to decide whether the coarse pink-stained and homogenous intercellular matrix is actually hyaline collagen or osteoid tissue, and that special stains for osteonectine, alkaline phosphatase, and electron microscopy (matrix extracellular vesicles) might help to distinguish osteoid from collagen.9 The diagnosis of fibrohistiocytic osteosarcoma has been made only by confirmation of direct tumor osteoid formation by the sarcoma growing in a storiform pattern, even if this only appeared in one microscopic field.8, 18 The histopathological features of the T10 vertebral tumor in our patient included atypical spindle cells arranged in a storiform pattern, immunoreactivity to vimentin α-smooth muscle actin, HHF35, and desmin, and absence of osteoid formation suggesting smooth muscle differentiation. The diagnosis therefore at the time of surgery was high-grade sarcoma, probable leiomyosarcoma. However, osteoid formation with calcification was subsequently observed in a chest wall nodule at autopsy, indicating that the correct diagnosis was in fact osteosarcoma. One cause of the inaccurate postoperative diagnosis might be related to the failure in examining the entire specimen, which was resected at surgery. However, osteoid formation was found only in the specimen of metastases at autopsy.9
Osteosarcoma may demonstrate immunoreactivity for α-smooth muscle actin. Devaney et al19 reported that one of the 16 cases of small cell osteosarcomas were positive for anti-α-smooth muscle antibody. Hasegawa et al20 found positive immunoreactivity for α-smooth muscle actin in 15 of 30 osteosarcomas, and proposed that tumor cell expression of α-smooth muscle actin be regarded as myofibroblastic differentiation. Povýšil et al,21 however, proposed that the presence of these antigens is due to aberrant actin microfilament expression. It remains unclear whether the presence of muscle tissue antigens in the case presented here is indicative of myofibroblastic differentiation of the tumor, or due to aberrant actin microfilament expression. Malignant bone tumors with features suggestive of myofibroblastic differentiation, however, require careful histopathological examination to distinguish them from the fibroblastic variant of osteosarcoma.
Based on the current case of T10 vertebral osteosarcoma, early detection and accurate diagnosis is important for improving not only patient prognosis but also the quality of life. We should always consider this rare entity, particularly in elderly patients presenting with back pain and vertebral collapse.
References
Dreghorn CR, Newman RJ, Hardy GJ, Dickson RA . Primary tumors of the axial skeleton. Experience of the Leeds Regional Bone Tumor Registry. Spine 1990; 15: 137–140.
Weinstein JN, McLain RF . Primary tumors of the spine. Spine 1987; 12: 843–851.
Barwick KW, Huvos AG, Smith J . Primary osteogenic sarcoma of the vertebral column. A clinicopathologic correlation of ten patients. Cancer 1980; 46: 595–604.
Shives TC, Dahlin DC, Sim FH, Pritchard DJ, Earle JD . Osteosarcoma of the spine. J Bone Joint Surg Am 1986; 68: 660–668.
Bielack SS et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on Neoadjuvant Cooperative Osteosarcoma Study Group Protocols. J Clin Oncol 2002; 20: 776–790.
Ozaki T et al. Osteosarcoma of the spine. Experience of the cooperative osteosarcoma study group. Cancer 2002; 94: 1069–1077.
Brooks S, Starkie CM, Clarke NMP . Osteosarcoma after the fourth decade. A clinico-pathological review. Arch Orthop Trauma Surg 1985; 104: 100–105.
Huvos AG . Osteogenic sarcoma of bone and soft tissues in older persons. A clinicopathologic analysis of 117 patients older than 60 years. Cancer 1986; 57: 1442–1449.
Campanacci M, Enneking WF . High grade osteosarcomas. In: Enneking WF (ed). Bone and Soft Tissue Tumors. Clinical Features, Imaging, Pathology and Treatment, 2nd edn. Piccin Nuova Libraria: Padova, and Springer-Verlag: Wien, New York 1999, pp 463–515.
Gambardella G, Gervasio O, Zaccone C . Does the neuronal plasticity exist in elderly patients? report of an unusual clinical case. Spinal Cord 2004; 42: 47–49.
Baba H, Maezawa Y, Uchida K, Furusawa N, Wada M, Imura S . Plasticity of the spinal cord contributes to neurological improvement after treatment by cervical decompression. A magnetic resonance imaging study. J Neurol 1997; 244: 455–460.
Nanassis K, Alesiadou-Rudolf C, Rudolf J, Frowein RA . Surgical indications and prognosis in spinal metastases. Neurosurg Rev 1997; 20: 99–103.
Bötel U, Gläser E, Niedeggen A . The surgical treatment of acute spinal paralysed patients. Spinal Cord 1997; 35: 420–428.
Talac R et al. Relationship between surgical margins and local recurrence in sarcomas of the spine. Clin Orthop 2002; 397: 127–132.
Gore L, Greffe BS, Rothenberg SS, Erickson M, Schreiber DP, Handler MH . Long-term survival after intralesional resection and multi-modal therapy of thoracic spine osteosarcoma. Med Pediatr Oncol 2003; 40: 400–402.
Bacci G et al. Histologic response of high-grade nonmetastatic osteosarcoma of the extremity to chemotherapy. Clin Orthop 2001; 386: 186–196.
Hauben EI, Weeden S, Pringle J, Van Marck EA, Hogendoorn PCW . Does the histological subtype of high-grade central osteosarcoma influence the response to treatment with chemotherapy and does it affect overall survival? A study on 570 patients of two consecutive trials of the European Osteosarcoma Intergroup. Eur J Cancer 2002; 38: 1218–1225.
Naka T, Fukuda T, Shinohara N, Iwamoto Y, Sugioka Y, Tsuneyoshi M . Osteosarcoma versus malignant fibrous histiocytoma of bone in patients older than 40 years. A clinicopathologic and immunohistochemical analysis with special reference to malignant fibrous histiocytoma-like osteosarcoma. Cancer 1995; 76: 972–984.
Devaney K, Vinh TN, Sweet DE . Small cell osteosarcoma of bone: an immunohistochemical study with differential diagnostic consideration. Hum Pathol 1993; 24: 1211–1225.
Hasegawa T, Hirose T, Seki K, Hizawa K, Ishii S, Wakabayashi J . Histological and immunohistochemical diversities, and proliferative activity and grading in osteosarcomas. Cancer Detect Prev 1997; 21: 280–287.
Povýšil C, Tomanová R, Matějovský Z . Muscle-specific actin expression in chondroblastomas. Hum Pathol 1997; 28: 316–320.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kokubo, Y., Uchida, K., Kobayashi, S. et al. Primary osteosarcoma of the thoracic spine: report of an unusual elderly patient with autopsy findings. Spinal Cord 43, 508–511 (2005). https://doi.org/10.1038/sj.sc.3101731
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101731