Abstract
Study design: Case series of a consecutive sample. Retrospective audit.
Objective: To analyze the long-term safety and efficacy of intrathecal baclofen (ITB), and technical incidents.
Setting: Neurosurgical and Physical Medicine Departments of two university hospitals in western France.
Methods: The medical records of 40 patients who underwent ITB pump placement for the treatment of severe chronic spasticity were reviewed. Patients were eligible independently of the origin of the spasticity (spinal cord origin 33, brain damage 8). They underwent a final assessment with clinical examination and questionnaire in 2001. Ashworth scale scores were assessed, patient satisfaction was rated on a visual analog scale (VAS), functional independence before and after treatment was classified as bed-ridden, wheelchair dependant or ambulant, and the frequency and nature of complications were noted.
Results: The average follow-up period was of 4 years. The average Ashworth score at the final assessment was 1.8±0.6. Average patients satisfaction was 7.4/10±2.21 on VAS. In all, 85% would have undergone the procedure again if they had to make the decision. In 85% of the cases the ambulation status was unchanged. Technical incidents occured at least once in 37% of the patients (due to the catheter in 58% and to the pump in 42%). They included catheter disconnections (4), migration (4), kinks (3), obstruction (3), development of fibrosis (3), disconnection of pump reservoir (2), porosity of pump membrane (2), unexplained pump dysfunction (4) leakage, and subcutaneous collection (5). Severe pharmacological side effects requiring transfer to intensive care unit occured in 12% of cases, 80% of which were directly related to pump refill procedures.
Conclusion: ITB remained effective in the long term and patients were satisfied. Nevertheless, complications were frequent, involving mainly the catheters, which would require further technical improvements.
Similar content being viewed by others
Introduction
Intrathecal baclofen (ITB) was first proposed in the treatment of spasticity by Penn and Kroin in 1984. Its first indication was chronic, medically intractable spasticity of spinal origin.1, 2 Indications have been extended to spasticity of other origins,3, 4 to dystonia,5 and more recently to the treatment of early vegetative dysfunction in traumatic brain injury.6, 7 Spasticity is defined by Lance as a velocity-dependent increase in muscle tone with exaggerated tendon jerk resulting from hyperexcitability of the stretch reflex. Several mechanisms are involved, among which are changes in the physical properties of the muscle,8, 9 collateral sprouting from dorsal root afferents, and enhancement of the spinal reflex deprived of supra-segmental inhibitory control.10 The latter mechanism is itself the result of several different abnormalities. The hyperexcitability of the alpha motoneuron and the decrease of presynaptic inhibition of Ia fibers have been established.11 More recent data point to the role of group II fibers and give some insight into the fact that the mechanisms may be different in spasticity of cerebral or spinal origin.12 The main effect of baclofen is to enhance presynaptic inhibition and thus inhibit monosynaptic and polysynaptic reflexes.13 Baclofen, 4-amino-3 (p-chlorophenyl) butyric acid is structurally similar to gamma aminobutyric acid (GABA) and binds mainly to pre- and post-synaptic GABA b receptors within the brainstem, the dorsal horn of the spinal cord, and other central nervous system sites. Intrathecally administrated baclofen acts directly and selectively at the spinal level.14, 15 Indeed, after lumbar administration, baclofen migrates upwards but the concentrations decline along the neuraxis so that the lumbar/cisternal ratio is approximately 4/1.16 The systemic passage is less than 1%.17
Finally, the development of reliable implanted pumps allowing precise drug delivery has allowed for the safe treatment of large populations. Nevertheless, questions remain.
What are the very long-term effects of ITB? The average follow-up of our serie is 4 years. In our departments, the first pumps were implanted in 1988. Thus, some patients have been followed for more than 10 years.
What is the long-term cumulated incidence of side effects? Catheter and pump malfunctions as well as severe overdoses have been reported with notable incidence.2, 18, 19, 20, 21
Methods
Subjects
The population was a consecutive sample of 41 patients (34 males, 7 females) implanted in the Neurosurgical departments between 1988 and 2001 and followed up in the Physical Medicine departments of two hospitals in the west of France. The average age at implantation was 37.3±13.7 years. Table 1 gives details of etiology. All patients had severe and intractable spasticity (Ashworth score ⩾3); they were either not relieved by maximal doses of oral medications or experienced unacceptable side effects.
Pre-implantation status
The functional status was classified into three stages of independence for ambulation. Patients were at stage I if they could stand with or without support though their walk was disturbed by spasticity. Wheelchair-dependent patients were classified at stage II. Bed-ridden patients were classified at stage III.
The Ashworth scores in the lower extremities, the presence of pain, oral antispasmodic drug intake, and side effects were noted.
Other data were grouped into a number of different goals: better ease of nursing care, specially concerning perineal hygiene, improvement of sitting and transfer abilities, and improvement of gait.
Procedure
All patients underwent test injections. The technique used for these injections (percutaneous lumbar puncture, continuous or bolus injection through a temporary catheter or an implanted subcutaneous port), the required dose, the clinical response, and the adverse effects were documented. The pumps were of three different types: manually operated pumps (MP), constant infusion systems (CIP), and programmable pumps (PP). The date of implantation, the location of the intraspinal catheter, and the use of a peri-operative antibiotic prophylaxis were recorded. For each patient, we noted the doses delivered at 1, 3, 6, 9, 12 months, and then every year. To analyze the evolution of the doses despite considerable interindividual variations, all doses were expressed as a multiple of the initial dose administered to that patient. When tolerance was suspected, the dose, the delay of occurrence, and the medical management were noted. In all cases where ITB was withdrawn, the cause was defined.
Complications
Pharmacological incidents were classified as serious if they required admission to an intensive care unit. The time of the last manipulation of the pump, the circumstances, and the treatment were noted, as well as the technical malfunctions of the pump or catheter, the infections and the skin breakdowns. The delay since the pump implantation or replacement was also considered. In order to account for the variation in the follow-up duration, the number of technical incidents was calculated per year of treatment.
Clinical examinations and interviews
All clinical examinations and interviews were conducted in 2001 by the first author. Three patients had died. In all, 29 were examined. Seven patients were interviewed by telephone. If they were unable to answer the questionnaire because of cognitive deficits, information was obtained from relatives or caregivers. One patient was unable to answer the questionnaire and could not be examined. The follow-up duration was defined as the period of time between implantation and assessment, or pump withdrawal, or death.
All patients assessed were questioned on the achievement of the objectives set before implantation. The objectives were established both by the physician and the patient. They were asked to rate the control of pain due to spasticity and their satisfaction on a 10-point visual analogic scale (VAS). They had to give a ‘Yes’ or ‘No’ answer to the improvement of sleep and to the question ‘would you choose to have baclofen intrathecal treatment again?’ The intake of oral antispastic and antalgic medications was recorded. The patients who came for the assessment were tested for tone in the lower extremities using the five-point Ashworth scale. The functional independence measure and the range of motion of lower limb joints were rated. The performance of orthopaedic surgical procedures since the onset of ITB was noted. Although nonparametric tests were used, average data and standard deviations are presented to facilitate the interpretation of the magnitude and of the clinical significance of the results. For clarity of presentation, the Ashworth scores of all muscles tested for lower limb were averaged.
Results
Functional status and goal achievement
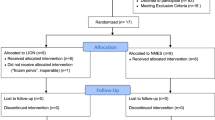
Table 2 demonstrates the settled objectives according to the independence stages of ambulation. The follow-up records show that the patients who are the most satisfied are those who were the most dependent: the goal of improving comfort was considered to be ‘completely achieved’ by 10/11 patients stage I and 14/16 patients stage II. The results are less pronounced on improving ambulation: 4/7 stage I patients were satisfied, the three other patients finally preferred wheelchair ambulation, which gave them more independence and required less energy. In three stage II patients, achievement of gait had been an original objective, it was achieved in one. Concerning changes in locomotion independence, 85% of the patients are classified as being in the same ambulation class as before implantation (Figure 1).
In all, 25 patients suffered from pain before implantation. The improvement through ITB was rated in 25% at more than 80%, in 40% at 30–50% on the VAS. Pain was unchanged in 20%. Some of the patients suffered from neuropathic pain, and were administered morphine or clonidine in association to ITB with success.22 Spasticity interfered with the quality of sleep for 18 patients before implantation: 75% of them reported marked improvement with ITB.
The answer to the question ‘would you undergo the procedure again if you had to make the decision?’ was positive in 85% of cases with an average VAS satisfaction of 7.4. Four subjects were dissatisfied. Grievances included the constraints of regular refills, the occurrence of complications, and the inability to ambulate in spite of better motor control. Two women complained about the size of the pump.
The assessment at follow-up confirmed the effect of baclofen in controlling spasticity. The original Ashworth score before implantation was always ⩾3, and the average Ashworth score at final assessment was 1.8±0.6 (27 patients evaluated). Oral Baclofen was permanently interrupted in 82% of cases and Diazepam in 36%.
Three neuro-orthopaedic operations were performed for fixed equinous on patients without surgical case history: two tendon lengthening and one neurotomy. None of the four patients with orthopaedic surgery history required further operation after implantation.
Procedure
All patients responded to the test dose injections before pump implantation. The average effective test dose of baclofen was 100.5±84.34 μg for spinal diseases and 143.5±197.32 μg for spasticity of cerebral origin. Test doses were administrated by lumbar puncture in 48.5% (18 cases of 37), by temporary intrathecal catheter in 38%, and using an implanted subcutaneous port in 13.5%. Two patients experienced headaches, one patient a drug overinfusion (somnolence and respiratory depression with 75 μg of baclofen), and three patients developed biologic meningitis (one test injection was performed via an intrathecal catheter and two via an access port). Meningitis was treated without any sequelae by removing the access port or catheter and antibiotic administration.
The first manual pump was implanted in 1988 and half of the pumps were implanted since 1997. In all, 57.5% of the first implanted pumps were programmable, 22.5% were constant infusion pumps and 20% were manually operated. Pump replacement was performed 1.4 times per patient, due to a complication in two-thirds of the cases.
In one hospital, antibioprophylaxis was systematically performed, whereas it was performed case by case in the other hospital. The catheter was introduced in the lumbar thoracic subarachnoid space and then placed at the thoracolumbar or midthoracic level depending on the injury level. Scopic control was not performed. In two cases, the catheter had to be replaced:
-
from cervical to midthoracic position because of central nervous system side effects (paraplegic patient T9 ASIA D);
-
from thoracic to lumbar position because of insufficient effectiveness in lower limb (tetraplegic patient C6 ASIA C).
Follow-up period, evolution of the required doses
Patients were followed for an average duration of 4 years after pump implantation. In 65% of cases, the follow-up period lasted more than 2 years, and in three cases it lasted more than 10 years (Figure 2). The average maximal dose used was 476±260.5 μg.
During the first year, the required doses increased by an average factor of 2.8. From the second year onwards, an increasing proportion of patients reached a stable dosage with the proportion rising to include 86% of patients at the end of the fifth year. Four patients developed an episode of possible tolerance, the diagnosis was confirmed in only one case. In each case, technical malfunction was excluded. X-ray films were taken to check the catheter, ITB bolus test were made to check the reliability of the pump, the permeability of the catheter, and patient's sensibility to the drug. This one patient suffered from multiple sclerosis with pressure sores. His spasticity was uncontrolled 18 months after pump implantation with a daily dose of 900 μg baclofen. There was no device malfunction and the bolus test was negative. The patient was given low doses of morphine and ITB was withdrawn. After 2 months ITB was resumed at 600 μg/day with successful management of spasticity. The dosage was not increased for 4 years in spite of the recurrence of pressure sores.
Pharmacological incidents
Common side effects occurred in 54% (20 patients). The most frequent were drowsiness, somnolence, nausea, and vomiting. Muscle weakness or epileptic seizures never occurred (the two epileptic patients remained well controlled by anticonvulsant medications). Five patients suffered from symptomatic trunk hypotonia, requiring in one case adjustments of the wheelchair and in the other moderate decrease of ITB doses.
In all, 12% of patients experienced severe side effects which were directly related to pump refill procedure in 80%. We recorded:
-
Two cases of respiratory arrest due to accidental overinfusion after pump refill.
-
One case of overinfusion (profound flaccidity, sedation and vomiting) due to manual pump malfunction.
-
One case of mild respiratory depression after a morphine test because of baclofen tolerance.
-
One case of malignant hyperthermia with multivisceral failure and death a few hours after pump refill.
Device incidents
One half of patients experienced at least one malfunction which required surgical management in 90%. In total, 62.5% of the patients experienced one episode of malfunction, 90% of them required surgical intervention, 47.5% required more than one intervention. The total rate of device malfunctions was 0.2 per year (31 device malfunctions/153 years of treatment). Table 3 gives details of complications: catheters were involved in 58% and pumps in 42% of cases. Pump complications were confined to manual pumps, except in one case where the malfunction of a constant infusion pump was probably caused by unusually warm outside temperature.
Clinical infections occurred in five patients. A biologic meningitis and an infected hematomae occurred postoperatively. Six deep pump pocket infections were treated with antibiotics and removal of the implanted equipment. Only three pumps were replaced. The number of clinical infections was equivalent in the two hospitals, independently of a peri-operative antibioprophylaxis. Since the addition of a bacteria-retentive filter to the refill kit in 2000, no infection has occurred to date in either hospital. Skin breakdown (erosion or pressure sore at the site of the pump) was noted in four patients and required removal of the pump in one case.
The pump was withdrawn and ITB definitively interrupted in seven patients (17.5% of cases). The cause was sepsis in three cases, baclofen overinfusion in one, intolerable side effects in one, and lack of use of manual pumps in two. In three stage II patients, achievement of gait had been an objective when the decision of using ITB was taken. It was achieved in one.
Discussion
Selection of patients
As exemplified in our experience, the main indication for ITB is chronic severe spasticity of spinal origin, after insufficient response to oral treatment. More recently, the effect of ITB has been demonstrated in dystonia whether associated or not to spasticity,5 in neuro-vegetative disorders following traumatic brain injury7 and in the prevention of orthopaedic complications in cerebral palsy.23 Rode et al24 have reported another effect of ITB on vasomotor disorders and cyanosis in a spastic paraplegic patient probably consecutive to the selective action of baclofen on autonomic innervation.
Goal setting and clinical assessment
The functional objectives of ITB depended on the initial functional status. In severely dependent patients, goals were focused on comfort, nursing, and prevention of cutaneous and orthopaedic complications; for wheelchair-dependent patients, they were focused on sitting and transfer abilities, and in ambulating patients they pointed on gait, endurance, and decreasing energy expenditure. Interviews revealed that ITB has improved markedly the ease of nursing care as well as the sitting and transfer abilities. Few patients progressed from one ambulation stage to the next but their quality of life was dramatically improved by therapy.
Did clinical assessments corroborate these overall evaluations by the patient?
Our evaluation using the Ashworth scale and the measure of the range of motion confirmed that ITB remains effective on the long term. This has also been the conclusion of the study by Lazorthes, with comparable follow-up periods.25
Pain control was based on the patient's comments via VAS. Painful muscle spasm and neuropathic pain were distinguished. The VAS is a valid and reliable instrument to document pain. It appears that the analgesic properties of ITB are directly correlated to the control level of spasms. The control of both pain and spasms contributes to better sleep.26 Some authors27 have found that ITB provides persistent analgesia in some patients with nociceptive, neuropathic or central pain, independently of the presence of spasticity. These patients received ITB after they had become tolerant to intrathecal morphine. These data suggest a specific antinociceptive property of ITB – which could be in competition in the presence of spasticity. The association of ITB and intrathecal morphine is possible.
Bolus test procedure
In our series, lumbar puncture has been used the more often. The occurrence of three cases of meningitis where the test had been performed via an access port or directly in the temporary catheter led us to abandon these administration techniques. This has also been reported by other authors.3 For our patients, the average dose at which the test was considered to be effective was higher when the spasticity was of cerebral origin. This has not been previously reported, probably because most tests used 100 μg as maximal dose. Albright28 considers that 85% of the patients respond to doses between 50 and 100 μg. Test doses above 100 μg have been considered to be dangerous and useless because response to such doses would imply treatment doses superior to 1000 μg.6 This has not been our experience. We never observed side effects in the patients tested with doses superior to 100 μg and follow-up doses never exceeded 1000 μg/day. Saltuari29 also comes to similar conclusions with test doses as high as 300 μg. Considering the high inter-individual variability in the response to baclofen, progressive increase of the test doses with careful monitoring seems safe and probably avoids false ‘nonrespondents’ who could in fact have benefited from the treatment at higher doses.
Implantation procedure
When the pump is implanted, one of the questions is the optimal placement of the tip of the intrathecal catheter. In SCI patients, positioning below the level of spinal injury seems to be more efficient and better tolerated.30 Some studies have evaluated the effect of ITB on upper limb spasticity: midthoracic catheter placement seems to offer better control than the rostral position on upper limb spasticity of both spinal and cerebral origin.31, 32 The cervical positioning is questioned because of the potential risk of central side effects.33 Thus, the choice for the treatment of upper limb spasticity depends on the function of lower limbs. If there is no remaining lower limb function, the safest choice is to increase the doses and keep to a lumbar position. If the lower limbs are functional, the choice will be between lower thoracic and mid-thoracic positioning depending on the distribution of the spastic pattern.
Follow-up period
The average follow-up period of our series was 4 years, longer than 2 years in 65% of patients and longer than 11 years in three cases. Most studies34 have an average follow-up period of less than 2 years, with the exception of the work by Lazorthes25 with a mean follow-up of 4 years in a series of 40 patients. This long follow-up was necessary to evaluate the cumulated rate of incidents and side effects that a patient offered life-long ITB would probably encounter. As reported by others,25, 35 we documented 10-fold variations in the average daily dose for SCI patients which were independent of the spinal level, the complete or incomplete nature of the lesion, the severity of spasticity, and the age and weight.36 In spasticity of cerebral origin, required doses appear to be higher,29, 37 although this does not achieve statistical significance in our sample. This is thought to be in particular the case of upper limb spasticity and/or association with dystonia.
The changes in required doses in two phases has also been described in long-term studies and is independent of pathology.2, 25 It can have an influence on the choice of the type of pump. If programmable pumps are fully justified as first implanted pumps, the period when frequent changes in the doses will be necessary, constant infusion pumps can be proposed at the steady-state period or for complete spinal lesions and nonambulant brain injured patients in which precise adjustments are less necessary. The software presently available calculates the required dilution so as to minimize the risk of errors.
Tolerance is defined by an increase in the required doses that does not result in any technical problem. Cases have been reported2, 37 mainly in the first two years of treatment and independently of the doses. Diagnosis relies on the exclusion of other causes of ineffectiveness and then to exclude possible device malfunction. Fibrosis impeding the diffusion of ITB and evolution of the neurological status is also possible. The treatment consists in a period of drug holiday of some weeks to some months usually with intrathecal morphine (because of its antispastic effect22 to provide a respite from baclofen). Then, opioids can be discontinued and the baclofen resumed at lower dose. The re-introduction of ITB is usually successful but most cases reported in the literature do not include long-term follow-up period and the effect could only be transitory.34, 38 In our one patient, the efficiency of ITB was observed for at least 4 years after re-introduction.
Pharmacological side effects
Minor side effects were observed in more than half of the patients. This was similar to the results by Penn in a series of 62 SCI.2 Our survey and other data2, 25 showed that ITB did not provoke muscle weakness, but it could have unmasked it by reducing spasticity. Test procedures allowed precise evaluation of the remaining motor function after treatment of spasticity and could have predicted the necessity of fine adjustments of ITB through programmable pumps, mainly in incomplete SCI patients.
We never observed epileptic fits, even in two epileptic patients on treatment. Two-thirds of cerebral palsy children are epileptic and it has been shown that ITB does not modify the occurrence of fits.3, 36, 39 Recently,40 EEG data were obtained in a patient with multiple sclerosis and major overinfusion. Generalized discharges were noted until the 20th hour and then decreased in parallel with clinical improvement. Nevertheless, the anticonvulsant effect of low-dose baclofen can be insufficient in hyperactivated areas and previous anticonvulsant treatments must be maintained during ITB.
Serious accidents occurred in 12% of the patients and were related to an operator-dependant error during a manipulation of the pump (mainly the refill procedure) in 80%. This significant frequency of operator-dependant errors was noted despite the fact that most refill procedures were performed by trained neurosurgeons or physical medicine specialists. The increasing number of patients on ITB imposes the development of very standardized procedures for follow-up with specific clinics. Overdosage of ITB can cause rostral progression of hypotonia, respiratory depression, coma, and occasionally seizures. Treatment is symptomatic with ventilatory support until baclofen is eliminated. Cerebrospinal fluid subtraction of 30–50 ml can help decrease ITB concentrations. Phystostigmine is no longer used as it interferes with other symptomatic intensive care procedures.41
One of the patient of our series died in unclear circumstances after refill of the pump and the most probable hypothesis is that of an abrupt withdrawal syndrome. Coffey19 proposed a review of this complication. Within 24–48 h, the patient presents with an exaggerated rebound spasticity, generalized seizures, hallucinations, hyperthermia, labile blood pressure or hypotension, and coma. In the absence of prompt and adequate treatment, rhabdomyolysis, hepatic and renal failure, coagulation disorders with disseminated intravascular coagulation and sometimes death may occur. Treatment includes oral baclofen at maximal doses (120 mg), intravenous diazepam, and intensive care symptomatic treatment. Benzodiazepines restore central gabaergic inhibition. Dantrolene sodium has a peripheral effect and is not indicated.42 Baclofen bolus injection in the lateral access of the pump is possible. Prevention of such accidents is of major importance and relies on the education of patients and caregivers. Patients could be provided with emergency kits including oral baclofen and injectable diazepam.
Superficial or deep infections were more frequent in manual pumps or when the test preceding the implantation has been performed through temporary catheter or access port.3, 43 The use of refill kits, including bacteria filters, has decreased their incidence.37, 44 The peri-operative antibioprophylaxis, suggested by some authors,28, 29 is not yet established. Besides classical treatment (antibiotics, removal, and then replacement of the pump), some authors have reported new approaches with instillation of appropriate antibiotics into the reservoir44 and intrathecal perfusion of antibiotics while continuing ITB,45 with success. This avoids the risks of baclofen withdrawal syndrome and of surgery. Further studies concerning the compatibility of baclofen and antibiotic drugs should be performed.
Technical incidents, specially with the catheter, are a well-known complication.21 The most difficult is to delineate the cause of catheter malfunction. An abdominal X-ray can localize a kink, a disconnection or a dislodgment. When the catheter is in place, radioisotopic control seems to be a reliable technique specially in cases of obstruction.46
Currently, marketed pumps are reliable,2, 43 but the alarm systems could be improved, in particular the reservoir alarm which relies on a computation of the theoretical remaining volume and not on an actual measure.
Conclusion
ITB therapy is an effective treatment therapy for intractable spasticity, especially for comfort and quality of life improvement. However, complications remain frequent. These data should be kept in mind in the indication of ITB. The benefit/risk discussion is a priority. The broadening of the indications of ITB and thus the increase in the number of patients receiving implanted pumps call for the development of standardized procedures for the follow-up of these patients. Standardized evaluations must be developed, routinely used, and should in our opinion include the measurement of the achievement of functional goals. The modalities of the refill procedure must also be standardized, with the development of specific clinics run by trained physicians and nurses.
References
Ochs G, Naumann C, Dimitreejevic M, Sindou M . Intrathecal baclofen therapy for spinal origin spasticity: spinal cord injury, spinal cord disease, and multiple sclerosis. Neuromodulation 1999; 2: 108–119.
Penn RD . Intrathecal baclofen for spasticity of spinal origin: seven years of experience. J Neurosurg 1992; 77: 236–240.
Gilmartin R et al. Intrathecal baclofen for management of spastic cerebral palsy: multicenter trial. J Child Neurol 2000; 15: 71–77.
Van Schaeybroeck P, Nuttin B, Lagae L, Schrijvers E, Borghgraef C, Feys P . Intrathecal baclofen for intractable cerebral spasticity: a prospective placebo-controlled, double-blind study. Neurosurgery 2000; 46: 603–609; discussion 609–612.
Albright AL, Barry MJ, Painter MJ, Shultz B . Infusion of intrathecal baclofen for generalized dystonia in cerebral palsy. J Neurosurg 1998; 88: 73–76.
Becker R, Alberti O, Bauer BL . Continuous intrathecal baclofen infusion in severe spasticity after traumatic or hypoxic brain injury. J Neurol 1997; 244: 160–166.
Becker R, Benes L, Sure U, Hellwig D, Bertalanffy H . Intrathecal baclofen alleviates autonomic dysfunction in severe brain injury. J Clin Neurosci 2000; 7: 316–319.
Detrembleur C, Plaghki L . Quantitative assessment of intrathecally administered baclofen in spasticity. Arch Phys Med Rehabil 2000; 81: 279–284.
O'Dwyer N, Adal L, Neilson P . Spasticity and muscle contracture following stroke. Brain 1996; 119: 1737–1749.
Mayer H . Clinicophysiologic concepts of spasticity and motor dysfunction in adults with an upper motoneuron lesion. Muscle Nerve 1997; 6: 1–13.
Katz RT . Réévaluation des mécanismes physiopathologiques qui génèrent le réflexe d'étirement: de nouvelles hypothèses sur la physiopathologie de la spasticité. Ann Readapt Med Phys 2001; 44: 268–272.
Aymar C, Katz RT, Lafitte C . Presynaptic inhibition and homosynaptic depression: a comparison between lower and upper limbs in normal subjects and patients with hemoplegia. Brain 2000; 123: 1668–1702.
Albright AL . Spastic cerebral palsy, approaches to drug treatment. CNS drugs 1995; 4: 17–27.
Albright AL . Intrathecal baclofen in cerebral palsy movement disorders. J Child Neurol 1996; 11(Suppl 1): S29–S35.
Gracies JM, Nance P, Elovic E, McGuire J, Simpson DM . Traditional pharmacological treatments for spasticity. Part II: General and regional treatments. Muscle Nerve Suppl 1997; 6: S92–S120.
Kroin JS, Ali A, York M, Penn RD . The distribution of medication along the spinal canal after chronic intrathecal administration. Neurosurgery 1993; 33: 226–230; discussion 230.
Albright AL, Shultz BL . Plasma baclofen levels in children receiving continuous intrathecal baclofen infusion. J Child Neurol 1999; 14: 408–409.
Rawicki B . Treatment of cerebral origin spasticity with continuous intrathecal baclofen delivered via an implantable pump: long-term follow-up review of 18 patients. J Neurosurg 1999; 91: 733–736.
Coffey RJ et al. Abrupt withdrawal from intrathecal baclofen: recognition and management of a potentially life-threatening syndrome. Arch Phys Med Rehabil 2002; 83: 735–741.
Reeves RK, Stolp-Smith KA, Christopherson MW . Hyperthermia, rhabdomyolysis, and disseminated intravascular coagulation associated with baclofen pump catheter failure. Arch Phys Med Rehabil 1998; 79: 353–356.
Penn RD, York MM, Paice JA . Catheter systems for intrathecal drug delivery. J Neurosurg 1995; 83: 215–217.
Chabal C, Jacobson L, Terman G . Intrathecal fentanyl alleviates spasticity in the presence of tolerance to intrathecal baclofen. Anesthesiology 1992; 76: 312–314.
Gerszten PC, Albright AL, Johnstone GF . Intrathecal baclofen infusion and subsequent orthopedic surgery in patients with spastic cerebral palsy. J Neurosurg 1998; 88: 1009–1013.
Rode G, Mertens P, Beneton C, Schmitt M, Boisson D . Regression of vasomotor disorders under intrathecal baclofen in a case of spastic paraplegia. Spinal Cord 1999; 37: 370–372.
Lazorthes Y, Sallerin B, Verdie JC, Casaux J, Caraoue F, Sol JC . Treatment of spasticity with the intrathecal administration of baclofen. Neurosurgery 1998; 44: 201–208.
Becker WJ, Harris CJ, Long ML, Ablett DP, Klein GM, DeForge DA . Long-term intrathecal baclofen therapy in patients with intractable spasticity. Can J Neurol Sci 1995; 22: 208–217.
Zuniga RE, Schlicht CR, Abram SE . Intrathecal baclofen is analgesic in patients with chronic pain. Anesthesiology 2000; 92: 876–880.
Albright AL . Baclofen in the treatment of cerebral palsy. J Child Neurol 1996; 11: 77–83.
Saltuari L et al. Long-term intrathecal baclofen treatment in supraspinal spasticity. Acta Neurol (Napoli) 1992; 14: 195–207.
Loubser PG, Narayan RK . Effect of subarachnoid catheter position on the efficacy of intrathecal baclofen for spinal spasticity. Anesthesiology 1993; 79: 611–614.
Grabb PA, Guin-Renfroe S, Meythaler JM . Midthoracic catheter tip placement for intrathecal baclofen administration in children with quadriparetic spasticity. Neurosurgery 1999; 45: 833–836; discussion 836–837.
Burns AS, Meythaler JM . Intrathecal baclofen in tetraplegia of spinal origin: efficacy for upper extremity hypertonia. Spinal Cord 2001; 39: 413–419.
Concalves J, Garcia-March G, Sanchez-Ledesma MJ, Onzain I, Broseta J . Management of intractable spasticity of supraspinal origin by chronic cervical intrathecal infusion of baclofen. Stereotact Funct Neurosurg 1994; 62: 108–112.
Creedon SD, Dijkers MP, Hinderer SR . Intrathecal for severe spasticity: a meta-analysis. Int J Rehabil Health 1997; 3: 171–185.
Azouvi P, Mane M, Thiebaut JB, Denys P, Remy-Neris O, Bussel B . Intrathecal baclofen administration for control of severe spinal spasticity: functional improvement and long-term follow-up. Arch Phys Med Rehabil 1996; 77: 35–39.
Albright AL, Barron WB, Fasick MP, Polinko P, Janosky J . Continuous intrathecal baclofen infusion for spasticity of cerebral origin. Jama 1993; 270: 2475–2477.
Armstrong RW, Steinbok P, Cochrane DD, Kube SD, Fife SE, Farrell K . Intrathecally administered baclofen for treatment of children with spasticity of cerebral origin. J Neurosurg 1997; 87: 409–414.
Coffey J et al. Intrathecal baclofen for intractable spasticity of spinal origin: results of a long-term multicenter study. J Neurosurg 1993; 78: 226–232.
Butler C, Campbell S . Evidence of the effects of intrathecal baclofen for spastic and dystonic cerebral palsy. AACPDM Treatment Outcomes Committee Review Panel. Dev Med Child Neurol 2000; 42: 634–645.
Fakhoury T, Abou-Khalil B, Blumenkopf B . EEG changes in intrathecal baclofen overdose: a case report and review of the literature. Electroencephalogr Clin Neurophysiol 1998; 107: 339–342.
Saltuari L et al. Failure of physostigmine in treatment of acute severe intrathecal baclofen intoxication. N Engl J Med 1990; 322: 1533–1534.
Green LB, Nelson VS . Death after acute withdrawal of intrathecal baclofen: case report and literature review. Arch Phys Med Rehabil 1999; 80: 1600–1604.
Gardner B et al. Intrathecal baclofen – a multicentre clinical comparison of the Medtronics Programmable, Cordis Secor and Constant Infusion Infusaid drug delivery systems. Paraplegia 1995; 33: 551–554.
Galloway A, Falope FZ . Pseudomonas aeruginosa infection in an intrathecal baclofen pump: successful treatment with adjunct intra-reservoir gentamicin. Spinal Cord 2000; 38: 126–128.
Zed PJ, Stiver HG, Devonshire V, Jewesson PJ, Marra F . Continuous intrathecal pump infusion of baclofen with antibiotic drugs for treatment of pump-associated meningitis. Case report. J Neurosurg 2000; 92: 347–349.
Le Breton F et al. Radioisotopic control for baclofen pump catheter failure. Spinal Cord 2001; 39: 283–285.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Plassat, R., Perrouin Verbe, B., Menei, P. et al. Treatment of spasticity with intrathecal Baclofen administration: long-term follow-up, review of 40 patients. Spinal Cord 42, 686–693 (2004). https://doi.org/10.1038/sj.sc.3101647
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101647
Keywords
This article is cited by
-
Cervical catheter placement leads to improved rostral distribution of a radiolabeled 18F-baclofen analog in cynomolgus monkeys
Translational Medicine Communications (2023)
-
The dosage and administration of long-term intrathecal baclofen therapy for severe spasticity of spinal origin
Spinal Cord (2018)
-
Permanent mechanical deformation of an intrathecal baclofen pump secondary to scuba diving: a case report
Spinal Cord (2013)