Abstract
Study design: Single case studies.
Objectives: To describe the technique of intensive locomotor training on an electromechanical gait trainer (GT) combined with functional electrical stimulation (FES).
Setting: Neurological Rehabilitation Clinic, Berlin, Germany.
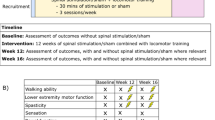
Methods: Four spinal cord-injured (SCI) patients, one tetraparetic, two paraparetic, and one patient with an incomplete cauda syndrome, more than 3 months postinjury, who were unable to walk at all, or with two therapists. They received 25 min of locomotor training on the GT plus FES daily for 5 weeks in addition to the regular therapy.
Results: The patients tolerated the programme well, and therapists rated the programme less strenuous compared to manually assisted treadmill training. Gait ability improved in all four patients; three patients could walk independently on the floor with the help of technical aids, and one required the help of one therapist after therapy; gait speed and endurance more than doubled, and the gastrocnemius activity increased in the patients with a central paresis.
Conclusion: This combined technique allows intensive locomotor therapy in SCI subjects with reduced effort from the therapists. The patients' improved walking ability confirmed the potential of locomotor therapy in SCI subjects.
Similar content being viewed by others
Introduction
Following the first description of a viable clinical system in 1987,1 goal-oriented treadmill training with partial body weight support (BWS) has evolved as a promising treatment option in spinal cord-injured (SCI) subjects. Several open clinical studies showed successful gait restoration in para- and tetraparetic subjects.2,3,4,5,6,7,8,9,10,11 Even paraplegic patients who were unable to walk on the floor exhibited a locomotor-like EMG activity of their leg muscles on the treadmill.4,5
Treadmill training with BWS enabled SCI patients to practise numerous gait cycles on the motor-driven belt. The enforced locomotion presumably activated spinal gait pattern generators, as in laboratory animals.12,13 Loading and unloading in the correct rhythm and hip extension during terminal stance phase were the major peripheral drives.14,15,16
One of the disadvantages of treadmill training was the effort for up to three therapists in lifting the paretic limbs, promoting hip extension, and assisting lateral weight transfer; this limits its use in routine clinical practice. To reduce the physical effort required of therapists, Hesse and Uhlenbrock designed an electromechanical gait trainer. Subject's feet are placed on two plates, whose movements simulated stance and swing phases,17 and the vertical and horizontal movements of the pelvis were controlled in a phase-dependent manner by ropes attached to the harness. Nonambulatory hemiparetic patients have shown improved walking ability and more normal patterns of muscle activation on the gait trainer, and the treatment requires less effort from the therapists compared to gait training on the treadmill.18,19
Colombo et al20,21 have chosen another solution to the problem of therapists' overexertion: their subjects wore a powered gait orthosis on the treadmill, which flexed the subjects' hip and knee joints during swing phase. Lower limb muscle activity of tetraparetic subjects on the treadmill was comparable during the manually assisted and the automated training with the driven gait orthosis.20,21
The present case studies describe the potential of the gait trainer therapy in SCI subjects who were non-ambulatory or ambulatory with technical aids and personal assistance. FES of the thigh muscles22 was additionally applied to stabilise the knees during the stance phase.
Methods
Gait trainer therapy
On the gait trainer, the harness-secured patients were positioned on two foot plates, whose movements simulated stance and swing phases with a ratio of 60–40% between the two phases (Figure 1). Cadence, stride length, and thus velocity could be set individually from 0 to 2.5 km/h. A servo-controlled motor assisted the gait movement at constant speed. The vertical and horizontal movements of the centre of mass (CoM) were controlled in a phase-dependent manner by ropes attached to the harness and connected to the gear system. The lateral movement over the stance limb helped to unload the swinging limb. Despite this lateral movement, patients tended to take advantage of the ongoing plate support, and put approximately 10–15% of their body weight onto the ‘swing’ limb.
Partial BWS was provided via an overhead pulley, and the actual amount was indicated on the display. The support was not kept constant but could vary, according to the controlled movement of the CoM. Two programmable dual-channel stimulators (biphasic constant current pulses, 20 Hz, 0.2 ms, 80 mA max, adjusted for a strong but tolerable muscle contraction) stimulated the quadriceps and biceps femoris muscles of both sides via 5 × 5 cm2 self-adhesive surface electrodes during the stance phase. The rotation of the gear system, detected with the help of a light cell, controlled the stimulator. In case of insufficient hip extension, an adjustable rear bar acting on the pelvis pushed the patients into extension.
BWS compensated for the weakness of the affected lower limbs, and was reduced as soon as possible to enable full limb loading. This was achieved when the patients could extend their hips and carry the weight sufficiently, that is, not swing in the harness. The training velocity was set individually, between 1 and 2 km/h. We aimed for each patient to take 800–1250 steps per session, which required a net treatment duration of approximately 20–25 min. Breaks were optional after each 5 min of therapy. Physical help, example, for additional control of the paretic knees, was administered according to individual needs.
The patients practised without any orthoses each workday for 5 weeks, that is, 25 treatment sessions. In addition, they participated in a conventional comprehensive in-patient rehabilitation programme. Minimal clinical criteria for inclusion into the programme were successful wheelchair mobilisation, no fixed contractures of the lower limb joints, no skin ulcers, and a stable cardiovascular system.
When possible, comprehensive gait analysis (Infotronic) was performed on the floor. This system consisted of overshoe-slippers, with the option to record the dynamic electromyogram of up to eight muscles. A portable data logger stored the data, and on being transferred to a PC, commercial software calculated the limb cycle parameters including the relative single stance duration (% cycle), the derived symmetry ratio (left divided by right if less than 1, or vice versa), the vertical forces (% body weight) including the displacement of the centre of pressure, and the rectified and averaged electromyogram normalised with respect to the gait cycle. The 10 m-time and 6 min walking distance were recorded to assess gait velocity and endurance.
Results
Subject #1
Male, 50 years old, with a spastic tetraparesis, 11 months after C5/C6 injury, ASIA D. His MRC scores (0–5) were 2 for hip flexion (L&R), 4 for knee extension (L&R), and 2 (L) and 3(R) for ankle dorsiflexion, totalling a motricity index (MI, 0–100) of 75 (L) and 82 (R). The modified Ashworth spasticity scores (0–5) were 1 (ankle dorsiflexion), 2 and 3 (left/right knee extension), and 4 (hip extension). Within the clinic, he used a wheelchair, and during the physiotherapy he could walk with the assistance of two therapists helping with balance and placing the paretic limbs a distance of 34 m at a velocity of 0.32 m/s. He needed a walker and a left ankle-foot orthosis (AFO). His gait was highly symmetrical (ratio 0.98), and he loaded each lower limb with approximately 80% body weight (BW) during a shortened single stance phase of 26%. The EMG of the shank muscles showed very little, rather tonic activity of both the tibialis anterior and gastrocnemius muscles (Figure 2).
Initially, he put on the harness in the wheelchair positioned in front of the gait trainer, and was transferred with the help of a crane and two therapists into the machine. While seated on a foldable chair, the feet were attached on the adjustable plates with Velcro, and pairs of self-adhesive surface electrodes were put on the quadriceps and the hamstring muscles of both sides. Then, the patient stood up with the help of the pulley, and the training started at a velocity of 1.2 km/h, a step length of 45 cm, and 20% body weight support. He tolerated the electrical stimulation of the thigh muscles well, but due to fatigue, the amplitude had to be increased every 7–8 min to elicit a visible muscle twitch. One therapist sat in front of the patient to further stabilise both knees. The adjustable rear bar assisted hip extension. The net walking time was 20 min with a break every 5 min. At the end, he was transferred back to his wheelchair with the help of the crane. After seven sessions, he could stand in front of the machine holding to a bar, put on the harness, and step into the machine with the help of one therapist. With FES, he could then practise independently for 25 min with one break after 10 min. The step length (velocity) was increased to 49 cm (1.8 km/h) and BWS was reduced to 10%. After 5 weeks, he could walk within the clinic independently while using a walker and a left AFO. He managed to climb one stair but preferred the elevator. Outside the clinic, he continued to use a wheelchair. The maximum walking distance (gait speed) on the floor was 296 m (0.81 m/s). The motor power and the spasticity scores did not change to a relevant extent. Gait analysis revealed an ongoing highly symmetric gait, a longer relative single stance duration (34%), and the ability to carry his entire BW on each lower limb. The EMG revealed a pronounced, phasic, and timely correct activation pattern of the tibialis and gastrocnemius muscles bilaterally (Figure 2).
Subject #2
A 45-year-old woman with a spastic paraparesis 8 months after a D7/8 SCI, ASIA D. Her muscle power, tested for ankle dorsiflexion, knee extension, and hip flexion ranged from 2 to 4, totalling an MI of 76 (left) and 80 (right). The spasticity was moderate with modified Ashworth (0–5) scores of either 2 or 3. She could walk with the help of two therapists a maximum distance of 14 m at a velocity of 0.12 m/s. Her gait was asymmetrical (swing ratio of 0.65), with a short relative single stance phase (16%, left, 25%, right), and each lower limb carried approximately 50% body weight (BW). EMG showed a timely correct activation of both tibialis anterior muscles, whereas the activity of the gastrocnemius, vastus medialis, and rectus femoris muscles was rather small and not well modulated (Figure 3). Right from the beginning, the patient could step into the machine with the help of one therapist, and she could practise independently with the FES after 10 sessions. Training velocities ranged from 1.5 to 2.0 km/h, and the BWS from 15 to 10%. After the programme, she could walk independently on the floor using two AFOs and a walker for 99 m at 0.26 m/s. Within the clinic, she continued to use a wheelchair. Her lower limb motor power and muscle tone did not change considerably. She walked more symmetrically, and almost carried 75% BW on each limb. The EMG (Figure 3) revealed the following improvements: an increased and timely correct activation of the gastrocnemius and vastus medialis muscles, and a monophasic activation of the rectus femoris muscles with an onset during midstance (right) and preswing (left). On the other hand, the left tibialis anterior pattern tended to be more tonic.
Rectified, averaged, and normalised EMG of the tibialis anterior, gastrocnemius, rectus, and vastus femoris muscles of both sides of a paraparetic subject (#2), level TH7/TH8, ASIA D, before and after therapy. Note the increased amplitude of the gastrocnemius muscles and the more physiological pattern of the thigh muscles after locomotor therapy
Subject #3
A 62-year-old male with a paraparesis 18 months after a D1/2 SCI, ASIA C. His body weight was 120 kg. He could not walk at all, although a KAFO had been prescribed 4 months before admission. His MRC scores were 1 (ankle dorsiflexion), 1 and 2 (left and right knee extension), and 2 and 3 (left and right hip flexion) totalling an MI of 42 (left) and 61 (right). The muscle tone was mildly increased with a modified Ashworth score of either 0, 1, or 2. Throughout the treatment, he was transferred with the crane into the machine and he required the help of two therapists sitting in front to assist knee extension, as FES only elicited a weak muscle twitch. The initial BWS was 35%, the step length 43 cm, and the velocity 1 km/h. for a total of 14 min. After 16 sessions, he could practise a net treatment duration of 25 min at a velocity of 1.5 km/h and a step length of 47 cm. Two therapists still had to assist knee extension, but with less effort. After 5 weeks of daily therapy, he could walk with the help of one therapist, a walker and bilateral KAFO a maximum distance of 17 m at 0.15 m/s. The isometric muscle strength and the muscle tone had not changed.
Subject #4
A 44-year-old man, with a flaccid paraparesis 3 months after an incomplete conus/cauda syndrome, level L1/L2, ASIA D. His left lower limb was weaker with an MRC score of 1 (ankle dorsiflexion, hip flexion) and 2 when tested for knee extension (MI 42), the corresponding MRC scores for the right lower limb were 4 (MI 79). Wearing an AFO on both sides, he could walk with the help of two therapists and a walker a maximum distance of 13 m at 0.16 m/s. The gait was highly asymmetric (see Figure 4), due to an extremely short left relative single stance duration (12 versus 31%), and he only carried 24% BW on his left and 52% on his right limb. The electromyogram of the shank muscles revealed small amplitudes particularly on the left side while the pattern was preserved.
During therapy, he required the ongoing help of one therapist to assist left knee extension, as he tolerated FES only on the right side. The BWS ranged from 10 to 15%, the velocity ranged from 1.2 to 1.8 km/h, and the step length was 46 cm. After 5 weeks, he could walk independently with AFOs and the walker a maximum distance of 112 m at 0.65 m/s. Within the clinic he continued to use a wheelchair. The muscle strength of his left dorsiflexor and knee extensor muscles mereased considerably (MRC 4), while the strength of the left hip flexor remained unchanged (MRC 1). The strength of the right limb improved less. Gait analysis revealed a more symmetrical gait (ratio of 0.75 versus 0.39) due to a prolongation, particularly of the left relative single stance duration (Figure 4). The only change in the shank muscles EMG was increased amplitude of the left dorsiflexor muscle.
All patients enjoyed the repetitive walking on the machine, as it reminded them of their walking pattern before their accident, and they could fully recommend it for other patients. The therapists appreciated the reduced effort on the machine as compared to the manually guided treadmill training or gait practise on the floor. They rated it as a meaningful adjunctive tool in gait rehabilitation; for further improvement, they suggested the individual adjustment of the foot trajectories and the possibility to deload fully the swinging limb.
Discussion
Automated gait training in combination with FES followed the principles of locomotor therapy in SCI subjects. The repetitive practice of 800–1200 steps per session over a period of 5 weeks resulted in a functionally useful improvement of gait ability of all four subjects who did not walk at all (one subject, ASIA C) or had required the assistance of two therapists in addition to orthotic devices (ASIA D) during floor walking before therapy. After therapy, one subject remained wheelchair-independent in the clinic all day long, two subjects could walk with aids for 99 and 112 m, and the most severely gait-impaired subject (ASIA C) managed to walk 7 m with the help of one person after therapy. Gait analysis revealed a more consistent, symmetric, and dynamic gait pattern, with the patients carrying more load on their lower limbs.
The machine was designed to reduce the therapeutic effort during the locomotor therapy. Instead of placing the limbs and controlling the trunk movements on the treadmill, the therapists sitting in front of the patients assisted the knee extension in combination with the FES. Less and less assistance was required during the course of the treatment and the therapists rated the work less strenuous as compared to the manually assisted treadmill training. The Lokomat, by Colombo et al,20,21 also reduced the therapeutic effort in SCI subjects; probably the applied exoskeleton provided more external guidance as compared to the gait trainer, which does not mechanically support the knees. Instead, the authors have chosen FES of the thigh muscles to stabilise additionally the knees in the stance phase. FES, however, excludes patients with a complete peripheral paresis of the thigh muscles and may provide less support than a mechanical joint, particularly in the beginning of the therapy when the muscles are atrophic. On the other hand, FES is actively therapeutic, promoting muscle strength, lower limb circulation, and bone mineralisation.22
The observed improvement of gait ability of the SCI subjects corresponds with the literature on treadmill training with BWS.2,3,4,5,6,7,8,9,10,11 For instance, Wernig et al8 studied 25 chronic patients, 5.5 months after injury. They were nonambulatory at all or required the help of two persons on the floor. After 12 weeks of daily locomotor therapy on the treadmill, 20 out of 25 could walk with a walker; eight subjects could even climb stairs. Voluntary muscle strength tested at rest only slightly improved.
Field-Fote10 reported on 19 subjects at least 12 months after an ASIA C injury. After 36 sessions of locomotor therapy in combination with FES, four of the six subjects, who had required manual assistance in addition to their orthotic devices before therapy, could walk without external help. For the whole group of patients, the mean overground speed improved from 0.12 m/s to 0.21 m/s. The mean treadmill distance per session increased from 93 to 243 m.
Our four cases improved to a similar degree after a much shorter period of training. Less therapeutic effort and a lower perceived exertion on the gait trainer probably resulted in a higher therapy intensity with the continuous practice of 800–1200 steps/session right from the beginning of therapy. On the other hand, a lesion interval of less than 12 months in three of the four subjects was lower than in most treadmill studies, so that spontaneous recovery, particularly in subject #4, may also explain this difference.
With respect to gait kinematics, Field-Fote and Tepavac23 also reported a more consistent gait pattern after locomotor therapy, and the present study additionally showed a more dynamic and symmetric gait with the patients carrying more weight on their lower limbs.
The results of the dynamic electromyography of the centrally paretic SCI subjects are confirming the results of Dietz et al4,5 on treadmill training with BWS: the amplitude of the gastrocnemius muscle increased in the centrally paretic subjects, and one patient showed a more physiologic pattern of the tibialis anterior and thigh muscles after therapy.
These case studies do not prove the efficacy of the device. Further, clinical studies will include a controlled trial and examining the feasibility of using the gait trainer with wheelchair-dependent ASIA B patients. Future technical developments will include programmable footplates and a force control to adjust the foot trajectories individually and fully unload the swinging limb.
References
Barbeau H, Wainberg M, Finch L . Description and application of a system for locomotor rehabilitation. Med Biol Eng Comput 1987; 25: 341–344.
Visintin M, Barbeau H . The effects of body weight support on the locomotor pattern of spastic paraparetic patients. Can J Neurol Sci 1989; 16: 315–325.
Wernig A, Müller S . Laufband locomotion with body weight support improved walking in persons with severe spinal cord injuries. Paraplegia 1992; 30: 229–238.
Dietz V, Colombo G, Jensen L . Locomotor activity in spinal man. Lancet 1994; 344: 1260–1263.
Dietz V, Colombo G, Jensen L, Baumgartner L . Locomotor capacity of spinal cord in paraplegic patients. Ann Neurol 1995; 37: 574–582.
Wernig A, Müller S, Nanassy A, Cagol E . Laufband therapy based on ‘rules of spinal locomotion’ is effective in spinal cord injured persons. Eur J Neurosci 1995; 7: 823–829.
Dietz V, Wirz M, Curt A, Colombo G . Locomotor pattern in paraplegic patients: training effects and recovery of spinal cord function. Spinal Cord 1998; 36: 380–390.
Wernig A, Nanassy A, Müller S . Maintenance of locomotor abilities follwoing Laufband (treadmill) therapy in para- and tetraplegic persons: follow-up studies. Spinal Cord 1998; 36: 744–749.
Behrman AL, Harkema SJ . Locomotor training after human spinal cord injury: a series of case studies. Phys Ther 2000; 80: 688–700.
Field-Fote EC . Combined use of body weight support, functional electric stimulation, and treadmill training to improve walking ability in individuals with chronic incomplete spinal cord injury. Arch Phys Med Rehabil 2001; 82: 818–824.
Protas EJ, Holmes SA, Qureshy H, Johnson A, Lee D . Supported treadmill ambulation training after spinal cord injury: a pilot study. Arch Phys Med Rehabil 2001; 82: 825–831.
Lovely RG, Gregor RJ, Roy RR, Edgerton VR . Effects of training on the recovery of full-weight bearing stepping in the adult spinal cat. Exp Neurol 1986; 92: 421–435.
Barbeau H, Rossignol S . Recovery of locomotion after chronic spinalization in the adult cat. Brain Res 1987; 412: 84–95.
Harkema SJ, Hurley SL, Patel UK, Requejo PS, Dobkin BH, Edgerton VR . Human lumbosacral spinal cord interprets loading during stepping. J Neurophysiol 1997; 77: 797–811.
Hesse S, Helm B, Krajnik J, Gregoric M, Mauritz KH . Treadmill training with partial body weight support: influence of body weight release on the gait of hemiparetic patients. J Neuro Rehab 1997; 11: 15–20.
Dietz V, Müller R, Colombo G . Locomotor activity in spinal man: significance of afferent input from joint and load receptors. Brain 2002; 125: 2626–2634.
Hesse S, Sarkodie-Gyan T, Uhlenbrock D . Development of an advanced mechanised gait trainer, controlling the movement of the centre of mass, for restoring gait in non-ambulant subjects. Biomed Tech 1999; 44: 194–201.
Hesse S, Werner C, Uhlenbrock D, v. Frankenberg S, Bardeleben A, Brandl-Hesse B . An electromechanical gait trainer for restoration of gait in hemiparetic patients: preliminary results. Neurorehabilitation and Neural Repair 2001; 15: 37–48.
Werner C, von Frankenberg S, Treig T, Konrad M, Hesse S . Treadmill training with partial body weight support and an electromechanical gait trainer for restoration of gait in subacute stroke patients: a randomized crossover study. Stroke 2002; 33: 2895–2901.
Colombo G, Joerg M, Schreier R, Dietz V . Treadmill training of paraplegic patients using a robotic orthosis. J Rehabil Res Dev 2000; 37: 693–700.
Colombo G, Wirz M, Dietz V . Driven gait orthosis for improvement of locomotor training in paraplegic patients. Spinal Cord 2001; 39: 252–255.
Kralj A, Bajd T . Functional Electrical Stimulation: Standing and Walking After Spinal Cord Injury. CRC Press: Boca Raton, FL, 1989.
Field-Fote EC, Tepavac D . Improved intralimb coordination in people with incomplete spinal injury following training with body weight support and electrical stimulation. Phys Ther 2002; 82: 707–715.
Acknowledgements
The work was supported by a BioFuture grant (BEO11) of the Bundesministerium für Bildung und Forschung, BMBF. We acknowledge the help of Stephen Kirker, Cambridge, in writing this paper.
Author information
Authors and Affiliations
Additional information
Disclosure statement: REHA-STIM company holds the patent for the electromechanical gait trainer used in this study. The company is owned and operated by Dr Beate Brandl-Hesse, spouse of the co-author, Dr Stefan Hesse
Suppliers
a. Reha-Stim, Dr. Beate Brandl-Hesse, Berlin, Germany.
b. Bentronic GmbH, Munich, Germany.
c. Infotronic, Tubbergen, Netherlands.
Rights and permissions
About this article
Cite this article
Hesse, S., Werner, C. & Bardeleben, A. Electromechanical gait training with functional electrical stimulation: case studies in spinal cord injury. Spinal Cord 42, 346–352 (2004). https://doi.org/10.1038/sj.sc.3101595
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101595
Keywords
This article is cited by
-
Robotic gait rehabilitation and substitution devices in neurological disorders: where are we now?
Neurological Sciences (2016)
-
Strategies and lessons in spinal cord injury rehabilitation
Current Physical Medicine and Rehabilitation Reports (2015)
-
Neurorobotic and hybrid management of lower limb motor disorders: a review
Medical & Biological Engineering & Computing (2011)