Abstract
Study design: A case report of the complications of a spinal cord injury (SCI) patient alternating between indwelling urethral catheter and a condom drainage system for bladder management.
Objective: To highlight the importance of penile care for bladder drainage following SCI.
Setting: Spinal Injuries Unit, Stanmore, UK.
Subject: A 39-year-old male who sustained a lumbar level SCI in December 2000. He presented acutely with leakage of urine around his condom drainage device.
Main outcome measure: The examination revealed an eroded area on the ventral aspect of the proximal penile shaft, which corresponded to the site of condom attachment. An indwelling urethral catheter was inserted as a temporary measure before reconstruction.
Result: At operation, in addition to the preoperatively observed area of erosion, the penile urethra was found to be cleaved for almost its entire length.
Conclusions: The patient had suffered two complications from a combination of two types of bladder management, and surgery was successful in treating both the urethral cleavage and the skin erosion.
Similar content being viewed by others
Introduction
Following the acute phase of spinal cord injury (SCI) several bladder management possibilities exist. The chosen method depends on the urodynamic findings, available resources and patient preferences. Most patients with SCI will use urethral catheterisation, either as indwelling catheterisation or clean intermittent self-catheterisation (CISC).1
The use of condom drainage system can render a male SCI patient effectively dry, but can lead to penile or urethral complications in 15–30% of patients.2 Other commonly reported problems range from allergic reactions and local defects in the skin, to gangrene and partial amputation of the penis.3,4 Additionally, it is well established that chronic urethral catheterisation can lead to penile cleavage.
We report a serious complication of alternating between using an indwelling urethral catheter and condom drainage system that highlights the extreme vigilance required in neuropathic patients.
Case report
A 39-year-old male presented to the emergency department complaining of frequent slippage of his condom drainage system and persistent urinary leakage around the site of its penile attachment. He had previously sustained a burst fracture of his L1 vertebra in December 2000. The patient had a history of alcohol abuse and associated psychological problems.
Videourodynamic investigation had subsequently revealed an acontractile bladder, and he was initially commenced on a regime of CISC. At 6 months prior to his emergency presentation, the patient had become poorly compliant with CISC. He had begun to alternate between a condom drainage system and an indwelling urethral catheter to manage his bladder, on the advice of his District Nurse.
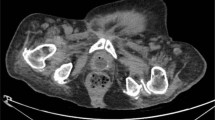
Clinical examination in the emergency department revealed a 3.5 × 2.5 cm2 area of erosion on the ventral aspect of the proximal penile shaft, which corresponded to the site of condom attachment. The urethral mucosa was exposed along the length of the eroded area (Figure 1). A urethral catheter was inserted into the bladder and the patient was scheduled for elective urethral reconstruction.
When the penile skin was incised preoperatively, cleavage of the entire length of the penile urethra was observed (Figure 2). The more distal area of urethral cleavage had been obscured by the overlying skin. A formal urethroplasty was successfully performed, and the patient is now effectively managing his bladder by CISC alone.
Discussion
The optimal management of the neuropathic bladder can at times be difficult to achieve. A balance has to be maintained between the ‘ideal’ management and what can be realistically achieved in individual circumstances. If condoms and urethral catheters are used for bladder management additional care is required to avoid potentially serious pitfalls. These complications are inevitably worsened by decreased sensation in SCI patients. Often the direct handling and maintenance of such systems is performed by carers, and increasingly the long-term care of SCI patients is now performed in the community by district nurses and general practitioners. It is therefore imperative that all members of the multidisciplinary team managing this group of patients understand the potential serious complications associated with condom drainage systems and urethral catheters, particularly in psychologically vulnerable patients. Carers and patients should be extremely vigilant with regard to penile skin care in order to avoid the progression of minor skin trauma to the anatomical destruction highlighted in this report. Condom drainage and permanent urethral catheterisation as a management strategy should be avoided both as combined and independent treatment modalities where possible in this patient group, and alternatives such as CISC be strongly considered where feasible.
References
Jamil F . Towards a catheter free status in neurogenic bladder dysfunction: a review of bladder management options in spinal cord injury (SCI). Spinal Cord 2001; 39: 355–361.
Golji H . Complications of external condom drainage. Paraplegia 1981; 19: 189–197.
Harmon CB, Connolly SM, Iarson TR . Condom related allergic contact dermatitis. J Urol 1995; 153: 1227–1228.
Steinhardt G, McRoberts JW . Total distal penile necrosis caused by condom catheter. JAMA 1980; 244: 1238.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bycroft, J., Hamid, R. & Shah, P. Penile erosion in spinal cord injury – an important lesson. Spinal Cord 41, 643–644 (2003). https://doi.org/10.1038/sj.sc.3101523
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101523
Keywords
This article is cited by
-
Catheter-induced urethral injury and tubularized urethral plate urethroplasty in such iatrogenic hypospadias
African Journal of Urology (2020)
-
Hypospadias in spinal cord injury: association with indwelling catheter drainage and disturbance of behavior: a report of three cases
Spinal Cord (2015)
-
Erosion of urethra in female patients with spinal cord injury
Spinal Cord (2005)