Abstract
Study design: Case report.
Objective: To describe the clinical presentations, radiological features and clinical progress of a rare case of chondroblastoma of the lumbar spine.
Setting: Regional Hospital, Hong Kong, China.
Method: A 54-year-old male patient presented with low back pain and left sciatica. X-ray and MRI revealed tumour infiltration of the fifth lumbar vertebrae and left paraspinal muscles, which was found to be a chondroblastoma by repeated open biopsies. The tumour was removed surgically by combined anterior and posterior approaches, followed by spinal fusion and instrumentation.
Results: The anterior tricortical bone graft was complicated with fracture and nonunion. Surgical re-exploration confirmed local recurrence of tumour macroscopically and histologically. The patient developed symptoms and signs of cauda equina syndrome gradually despite repeated surgery and irradiation. The patient eventually died of complications of local recurrence and neurological deficit at 3 years and 8 months after the first operation.
Conclusion: This is the first case report of chondroblastoma of the lumbar spine. The clinical profile of this patient and the evidence from the literature review suggests that spinal chondroblastoma has a very aggressive behaviour with high recurrence and mortality rate.
Similar content being viewed by others
Introduction
Chondroblastoma is a rare, primary, usually benign, bone tumour of immature cartilage cell. It has been called a ‘cartilage containing giant-cell tumour’, ‘calcifying giant-cell tumour’ and ‘epiphyseal chondromatous giant-cell tumour’. Jaffe and Lichtenstein1 in 1942 started to use the name ‘benign chondroblastoma’ because of its cartilaginous nature.
It is reported that about 1% of benign primary bone tumours are chondroblastoma. They are usually found at the epiphyseal regions of the long bones.2 The common sites are femur, humerus, tibia and the tarsal bones. Most patients are adolescents and young adults. The male to female ratio is around 2:1. Common complaints of patients are local pain, swelling and loss of adjacent joint function. The typical X-ray finding is an eccentric osteolytic lesion at the epiphysis of the long bone with metaphyseal expansion and cortical thinning. The lesion might show up radio-opaque stippled or fluffy calcifications with occasional streaky bone formation.
The characteristic macroscopic appearance of the tumour is of a chondroid lesion with cystic and haemorrhagic areas. The consistency varies from soft to gritty depending upon the amount of calcification or ossification. Histologically, it is characterized by uniform closely packed polyhedral cells separated by a scanty interstitial matrix, the chondroid appearance. Other classic features include the presence of lattice-like intercellular calcifications resembling chicken wire or picket-fence and the multinucleated giant cells.
Treatment options for this benign tumour include local curettage with or without bone grafting or cryosurgery and resection with a margin of normal tissue. The local recurrence rate ranges from 24 to 100%, depending on the presence of aneurysmal bone cyst within the lesion and the treatment method. Malignant transformation or metastasis is extremely rare. Those reported cases were usually associated with a history of irradiation.
The spine is an extreme rare location for this tumour and only five case reports were found in the literature.3,4,5,6,7 Chondroblastoma of the lumbar spine has never been reported previously.
Case report
A 54-year-old man, clerk of a bank, had low back pain and left sciatica for four months. The pain was mild in severity, dull aching and continuous in character. There were neither constitutional symptoms nor sphincter disturbance. Examination revealed mild tenderness over his lower lumbar spine without any palpable mass. The only positive neurological sign was minimal weakness of extension of the left big toe.
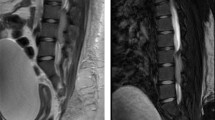
X-ray of lumbar spine showed an osteolytic lesion over the left side of fifth lumbar vertebral body with involvement of posterior complex (Figure 1). There was fine calcification over the left paraspinal region. All the blood tests, including common tumour markers, were normal. Bone scan was suggestive of secondary deposits in the fifth lumbar vertebrae and left sacroiliac joint without other active bone lesion. Magnetic resonance imaging (MRI) revealed a bone tumour involving most of the fifth lumbar vertebrae with soft tissue extension to the left psoas, left erector spinae muscles and spinal canal (Figure 2a,b).
With the tentative diagnosis of a metastatic lesion of the fifth lumbar vertebrae, open biopsy was performed through a midline incision posteriorly, but the specimen just yielded mature fatty tissue mixed with skeletal muscle fibres. A second open biopsy showed large mononuclear cells mixed with osteoclast-like giant cells growing in chondroid matrix, which was compatible with chondroblastoma, a diagnosis supported by an overseas expert (Figure 3).
After a thorough discussion with the patient on the dilemma of incomplete removal with possibility of recurrence and ‘wide excision’ with major postoperative neurological deficit, a less radical approach was adopted.
The tumour was surgically removed by an ‘intra-lesional excision’ through a combined posterior and anterior approach in August 1995. The tumour was first tackled posteriorly. The left posterior complex of L5, including the superior facet, pars interarticularis, inferior facet, transverse process and pedicle, was infiltrated by tumour. There was also soft tissue extension into the epidural space and left paraspinal muscles. Tumour tissue was removed as much as possible. Pedicle screws and Steffe plates were applied from L4 to S1 together with posterolateral fusion using autologous bone graft. The patient was turned into right lateral position. The fifth lumbar vertebral body was approached retroperitoneally. The whole L5 vertebral body, with the exception of the right lateral cortex, was filled up with tumour tissues. Corpectomy of L5 including the disc above and below was performed. Tricortical bone graft was obtained from left iliac crest and impacted into defect. The postoperative period was uneventful and he was discharged with an orthoplastic lumbar brace.
On consultation with an oncologist, it was decided to give adjuvant irradiation to the operative field after the bone graft was taken because the operation was an intralesional excision. However, before any irradiation was given, the patient had sudden onset of back pain in February 1996, that is, 6 months postoperatively. The repeated X-ray showed fracture of the anterior tricortical bone graft. He refused to have further surgery at that time and the fracture developed into nonunion.
Re-exploration was finally carried out anteriorly in April 1996 because of persistent back pain. Both ends of the original tricortical bone graft were fused with adjacent vertebral bodies. There was a nonunion at the midportion of the bone graft and it was surrounded by tumour tissues. The space was curetted again and another tricortical bone graft was inserted. The tumour tissue was found to be chondroblastoma again with no evidence of malignant transformation. He developed left lower limb swelling on the 3rd day. Doppler examination confirmed deep vein thrombosis of the left femoral vein. He was heparinized and treated with warfarin for 6 months.
Irradiation was given to the left sacral alar using two anteroposterior fields 3 months after the second operation. A total of 50 Gy in 25 fractions over 38 days was delivered using 8 MV photons. There was no irradiation to the anterior tricortical bone graft site initially because of the worry about interference of bone graft incorporation. He had residual mechanical back pain and the implants were found to loosen at the 4th month after the second operation.
Eventually, his mechanical spinal problem was managed operatively on November 1996, that is, 7 months after the second operation. Intraoperatively, it was found that there was incorporation of bone graft over the right posterolateral region, but the left side was mostly infiltrated by recurrent tumour, which was confirmed to be chondroblastoma again by postoperative histological examination. The loosened Steffe plates and screws were removed. Titanium Isola instrumentation was performed with pedicles screws at L2 and L3 bilaterally, pedicle screw at right S1 and bilateral iliac screws. Repeated posterolateral fusion from L2 to sacrum was performed bilaterally using allograft from the bone bank. His back pain was improved with the revision stabilization initially. Repeated MRI revealed an increase in the size of tumour, extending from the lower end of L4 to S1. Additional irradiation (60 Gy) was given from L3 to S2, using photons through lateral fields and anterior field with avoidance of previously irradiated area under steroid cover.
At 11/2 year after the third operation, the patient had progressive pain and tightness over his lumbar spine together with decrease in pin-prick sensation over both buttocks and lower limbs. There was weakness over both ankles and toes (grades 3–4) and difficulty in urination. The clinical picture was compatible with cauda equina syndrome. The third MRI confirmed a huge local recurrent tumour with cauda equina compression (Figure 4). The patient decided to have no more surgical intervention after analysing the remote benefit and the possible surgical risks. He also seeked advice and treatment from a herbalist.
The patient had increasing back pain and weakness of both lower limbs so much so that he became bed and wheelchair bound at 2 years after the third operation. There was a firm mass over his abdominal wound, which increased in size gradually. The posterior implant was found to be broken. Finally, he died at 21/2 years after the third operation because of fungating growth from the lower lumbar spine, multiple bed sores, urinary tract infection and septicaemia in an another hospital.
Discussion
Chondroblastoma is an uncommon and benign tumour of the bone. Pain is the most common complaint. The characteristic radiological features is an eccentric osteolytic lesion at the epiphyeal region of long bones with a sclerotic margin and intralesional calcification. Bloem and Mulder8 reported that radiological diagnosis had a sensitivity of 75% and specificity of 99%. The diagnosis can be confirmed by the histological features of rounded or polygonal chondroblast-like cells, cartilaginous intercellular matrix, multinucleated giant cells and the focal calcification.
Owing to the benign nature, this tumour is usually treated by local curettage with or without bone grafting or cryosurgery. Local recurrence is a rather common problem. Huvos and Marcove2 reported that the 3 years recurrence rates were 24% for chondroblastoma alone and 100% for chondroblastoma associated with aneurysmal bone cyst. Resection is advocated with a margin of surrounding normal tissue when this can be accomplished without great loss of function.9 Irradiation should be reserved for complicated cases because of the risk of irradiation-induced malignant transformation.10 Aggressive behaviour of chondroblastoma has been reported.11
Chondroblatoma is extremely rare in the spinal column. Buraczewski et al4 first reported a case of chondroblastoma of T3/4 in a 28-year-old man in 1957. The patient had spinal pain and neurological symptoms and signs. X-ray showed partial destruction of the neural arch of T3 and T4. Aspiration biopsy confirmed the diagnosis of chondroblastoma. The tumour was treated by laminectomy and resection, followed by postopertaive radiotherapy. The patient was found to be symptom-free 2 years after operation. However, the radiological picture was found to be nearly the same as before operation.
Wisniewski et al7 described a case of upper cervical chondroblastoma in 1973. The 17-year-old boy presented with progressive neck stiffness and occasional ‘dizziness’. The only physical signs were torticollis and limited neck movements. X-ray demonstrated an expansile osteolytic lesion at the right side of the atlas with involvement of the occipital condyle and axis. The tumour was treated by curettage under microscopic control. The postoperative clinical progress was not reported in the manuscript.
A fatal case of chondroblastoma of the sacrum was published by Akai et al.3 The 48-year-old patient presented with low back pain and was found to have a radiolucent lesion in the lateral half of the upper sacrum. Initial biopsy suggested a giant cell tumour. Surgical removal was considered to be too difficult and the tumour was treated with radiotherapy. The patient was lost to follow-up for 1 year but returned with abdominal pain, impaired renal function and hydronephrosis of the right kidney. The patient had further irradiation and surgical exploration with curettage. There was a gradual deterioration postoperatively and he eventually died 10 years after the initial presentation. Autopsy confirmed the diagnosis of chondroblastoma histologically.
Another fatal case of cervical chondroblastoma was reported by Hoeffel et al.5 The 9-year-old boy suffered from cervical pain and abnormal anterior position of the head. He was found to have clinical signs of superior mediastinum compression. X-ray showed an opacity and a discrete enlargement of the right foramen of the seventh cervical vertebra. The tumour was treated by repeated surgery and radiotherapy. The histological diagnosis was giant cell tumour initially but finally concluded to be chondroblastoma. However, the patient eventually died of complications of tetraplegia 72 months later.
Howe et al6 described a 16-year-old patient with chondroblastoma of C5/6, who had symptoms of tightness of neck muscles and limitation in motion.6 The tumour was treated with four-stage surgical procedures. The author did not describe the postoperative course of this patient. Lastly, Huvos and Marcove2 mentioned four cases and Bloem and Mulder8 reported one case of spinal chondroblastoma in their review without any text description.
The clinical presentation, the location, the types of operation and their clinical progress of all reported cases (including this case report) are summarized in Table 1. All spinal chondroblastoma were found in man only, in contrast with the 2:1 male to female ratio for all chondroblastoma.2 Their age ranged from 9 to 54. The patient of this report was the eldest one in this series. Pain was the most common complaint with the exception of Wisnieski's case. Neurological deficit was found in two-thirds of patients. The most common region was the cervical spine (50%). This is the first reported case of vertebral chondroblastoma originating from the lumbar spine. All cases had extraspinal soft tissue extension and calcification. All were treated with surgery eventually, but adjuvant irradiation was used in three patients. Two case reports did not mention the final outcome of the patients. Three patients died of complications of recurrent tumour at 3 years and 8 months, 6 years and 10 years after surgery. One patient was described to be ‘free of symptom’ 2 years after operation. Both the overall recurrence rate and mortality rate were 75%.
Primary tumours of the spine are both rare and difficult to treat. Complete surgical excision is the key factor for patient survival, recovery and maintenance of neurological function. Awareness of such a possibility is essential in the clinical management of neoplastic conditions of the spine. It is mandatory to identify the anatomical involvement of the spine by the tumour preoperatively using computerized tomogram (CT) scan and MRI. The Weinstein system of classification of spinal tumour is very useful for the surgical planning.12 It is recommended that primary spine tumours should be biopsied and treated by surgeons experienced in the approach and management of these most difficult problems.13 Biopsy from the transpedicular approach is preferred, so that the chance of contamination of surrounding soft tissues is minimal and the biopsy tract can be easily excised during the definitive procedure.
This patient had a benign chondroblastoma of the fifth lumbar vertebrae, which has involved zone I–IV, layer A–D, location 1 to 8 or 9 on presentation. It was beyond the possibility of complete excision without major neurological deficit because of the tumour invasion of the epidural space and paraspinal muscles. An intralesional type of excision together with spinal instrumentation was performed after analysing the problem with the patient. The end result was recurrence of tumour, confirmed by histology from re-exploration and repeated imaging, despite the combined efforts of operative interventions and irradiation. The patient eventually died of complications of recurrent tumour locally and cauda equina syndrome. The literature review shows evidence that chondroblastoma of the spine behaves more aggressively than those in long bones, with high recurrence rate and mortality rate.
Furthermore, this case illustrated the problem of mechanical instability after a vertebrectomy of L5. Both the initial and the revision spinal instrumentations resulted in failure. The main contributing factor is the failure of achieving a good spinal fusion as a result of recurrent tumour both anteriorly and posteriorly. However, this junctional level between the mobile lumbar spine and the rigid sacrum has its own biomechanical difficulty. Reconstruction and stabilization at this level are a great challenge to the spinal surgeon. Good and strong reconstruction of the anterior column is needed after an L5 vertebrectomy. The best option nowadays is a metal cage or femoral allograft with autograft composite nowadays because of their higher resistance to compressive load before the time of bone incorporation. Anterior instrumentation and stabilization is not possible at this level because of the presence of major great vessels. Stabilization can only be done posteriorly. It is advisable to have a strong and long construct using pedicle screws at the lumbar spine together with sacral and iliac fixation because of the inherent instability at this junctional level. It is mandatory to have good fusion in order to prevent failure of instrumentation.
Lastly, there was a problem of reassessment of the local condition when the patient had a fracture and nonunion of the bone graft as a result of the presence of stainless-steel implants. Titanium instrumentation should be the choice at the first operation.
In conclusion, this is the first case report of chondroblastoma of the lumbar spine. The clinical profile of this patient and the evidence from the literature review suggest that spinal chondroblastoma has an aggressive behaviour with high recurrence and mortality rate. Preoperative assessment by CT scan and MRI, well-performed transpedicular biopsy and primary en bloc excision may be the only chance to eradicate this tumour and prevent fatal outcome. Salvage or revision operation is difficult and usually futile. Stable anterior reconstruction, strong and long posterior titanium instrumentation, as well as good fusion are necessary at this junctional level.
References
Jaffe HL, Lichtenstein L . Benign chondroblastoma of bone. A reinterpretation of the so-called calcifying or chondromatous giant cell tumor. Am J Pathol 1942; 18: 969–983.
Huvos AG, Marcove RC . Chondroblastoma of bone: a critical review. Clin Orthop 1973; 95: 300–312.
Akai M et al. Chondroblastoma of the sacrum. Acta Orthop Scand 1986; 57: 378–381.
Buraczewski J, Lysakowska J, Rudowski W . Chondroblastoma (Codman's tumour) of the thoracic spine. J Bone Joint Surg [Br] 1957; 39-B: 705–710.
Hoeffel JC et al. About one case of vertebral chondroblastoma. Pediatr Radiol 1987; 17: 392–396.
Howe JW, Baumgard S, Yochum TR, Sladich MA . Case report 449. Skeletal Radiol 1988; 17: 52–55.
Wisniewski M et al. Chondroblastoma of the cervical spine. J Neurosurg 1973; 38: 763–766.
Bloem JL, Mulder JD . Chondroblastoma: a clinical and radiological study of 104 cases. Skeletal Radiol 1985; 14: 1–9.
Carnesale PG . Benign (occasionally malignant) tumors of bone. In: Canale ST (ed). Campbell's Operative Orthopaedics. Vol 1, 9th edn. Mosby-Year Book: St Louis, 1998, pp 703–713.
Hatcher CH . The development of sarcoma in bone subjected to roentgen or radium irradiation. J Bone Joint Surg Am 1945; 27-A: 179.
Huvos AG, Higinbotham NL, Marcove RC, O'leary P . Aggressive chondroblastoma: review of the literature on aggressive behavior and metastases with a report of one new case. Clin Orthop 1977; 126: 266–272.
Weinstein JN . Spine neoplasms. In: The Pediatric Spine–Principles and Practice, Vol 1. Raven Press: New York 1994, pp 887–916.
Weinstein JN . Primary tumors of the spine. Spine 1987; 12: 843–851.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Chung, O., Yip, S., Ngan, K. et al. Chondroblastoma of the lumbar spine with cauda equina syndrome. Spinal Cord 41, 359–364 (2003). https://doi.org/10.1038/sj.sc.3101458
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101458
Keywords
This article is cited by
-
Chondroblastoma of Thoracic Vertebrae: a Case Report and Review of the Literature
Indian Journal of Surgical Oncology (2024)
-
Clinicopathological characteristics and prognostic factors in axial chondroblastomas: a retrospective analysis of 61 cases and comparison with extra-axial chondroblastomas
World Journal of Surgical Oncology (2023)
-
Missed radiographic and clinical findings in a case of non-idiopathic scoliosis resulting from chondroblastoma
Spine Deformity (2021)
-
Clinical features, treatments and long-term follow-up outcomes of spinal chondroblastoma: report of 13 clinical cases in a single center
Journal of Neuro-Oncology (2018)