Abstract
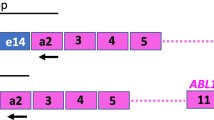
Real-time quantitative RT-PCR (RQ-PCR) is a sensitive tool to monitor minimal residual disease (MRD) in leukemic patients through the amplification of a fusion gene (FG) transcript. In order to correct variations in RNA quality and quantity and to calculate the sensitivity of each measurement, a control gene (CG) transcript should be amplified in parallel to the FG transcript. To identify suitable CGs, a study group within the Europe Against Cancer (EAC) program initially focused on 14 potential CGs using a standardized RQ-PCR protocol. Based on the absence of pseudogenes and the level and stability of the CG expression, three genes were finally selected: Abelson (ABL), beta-2-microglobulin (B2M), and beta-glucuronidase (GUS). A multicenter prospective study on normal (n=126) and diagnostic leukemic (n=184) samples processed the same day has established reference values for the CG expression. A multicenter retrospective study on over 250 acute and chronic leukemia samples obtained at diagnosis and with an identified FG transcript confirmed that the three CGs had a stable expression in the different types of samples. However, only ABL gene transcript expression did not differ significantly between normal and leukemic samples at diagnosis. We therefore propose to use the ABL gene as CG for RQ-PCR-based diagnosis and MRD detection in leukemic patients. Overall, these data are not only eligible for quantification of fusion gene transcripts, but also for the quantification of aberrantly expressed genes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Coustan-Smith E, Behm FG, Sanchez J, Boyett JM, Hancock ML, Raimondi SC et al. Immunological detection of minimal residual disease in children with acute lymphoblastic leukaemia. Lancet 1998; 351: 550–554.
Lucio P, Gaipa G, van Lochem EG, van Wering ER, Porwit-MacDonald A, Faria T et al. BIOMED-I concerted action report: flow cytometric immunophenotyping of precursor B-ALL with standardized triple-stainings. BIOMED-1 concerted action investigation of minimal residual disease in acute leukemia: international standardization and clinical evaluation. Leukemia 2001; 15: 1185–1192.
Brisco MJ, Condon J, Hughes E, Neoh SH, Sykes PJ, Seshadri R et al. Outcome prediction in childhood acute lymphoblastic leukaemia by molecular quantification of residual disease at the end of induction. Lancet 1994; 343: 196–200.
San Miguel JF, Martinez A, Macedo A, Vidriales MB, Lopez-Berges C, Gonzalez M et al. Immunophenotyping investigation of minimal residual disease is a useful approach for predicting relapse in acute myeloid leukemia patients. Blood 1997; 90: 2465–2470.
Cave H, van der Werff ten Bosch J, Suciu S, Guidal C, Waterkeyn C, Otten J et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of Cancer – Childhood Leukemia Cooperative Group. N Engl J Med 1998; 339: 591–598.
van Dongen JJ, Seriu T, Panzer-Grumayer ER, Biondi A, Pongers-Willemse MJ, Corral L et al. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet 1998; 352: 1731–1738.
Lion T, Henn T, Gaiger A, Kalhs P, Gadner H . Early detection of relapse after bone marrow transplantation in patients with chronic myelogenous leukaemia. Lancet 1993; 341: 275–276.
Diverio D, Rossi V, Avvisati G, De Santis S, Pistilli A, Pane F et al. Early detection of relapse by prospective reverse transcriptase-polymerase chain reaction analysis of the PML/RARalpha fusion gene in patients with acute promyelocytic leukemia enrolled in the GIMEMA-AIEOP multicenter ‘AIDA’ trial. GIMEMA-AIEOP Multicenter ‘AIDA’ Trial. Blood 1998; 92: 784–789.
Romana SP, Poirel H, Leconiat M, Flexor MA, Mauchauffe M, Jonveaux P et al. High frequency of t(12;21) in childhood B-lineage acute lymphoblastic leukemia. Blood 1995; 86: 4263–4269.
Pallisgaard N, Hokland P, Riishoj DC, Pedersen B, Jorgensen P . Multiplex reverse transcription-polymerase chain reaction for simultaneous screening of 29 translocations and chromosomal aberrations in acute leukemia. Blood 1998; 92: 574–588.
Grimwade D . Screening for core binding factor gene rearrangements in acute myeloid leukemia. Leukemia 2002; 16: 964–969.
Gabert J . Detection of recurrent translocations using real time PCR; assessment of the technique for diagnosis and detection of minimal residual disease. Haematologica 1999; 84: 107–109.
Bustin SA . Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol 2000; 25: 169–193.
Lion T . Current recommendations for positive controls in RT-PCR assays. Leukemia 2001; 15: 1033–1037.
Zhang Z, Harrison P, Gerstein M . Identification and analysis of over 2000 ribosomal protein pseudogenes in the human genome. Genome Res 2002; 12: 1466–1482.
Pallisgaard N, Clausen N, Schroder H, Hokland P . Rapid and sensitive minimal residual disease detection in acute leukemia by quantitative real-time RT-PCR exemplified by t(12;21) TEL-AML1 fusion transcript. Genes Chromosomes Cancer 1999; 26: 355–365.
Guerrasio A, Pilatrino C, De Micheli D, Cilloni D, Serra A, Gottardi E et al. Assessment of minimal residual disease (MRD) in CBFbeta/MYH11-positive acute myeloid leukemias by qualitative and quantitative RT-PCR amplification of fusion transcripts. Leukemia 2002; 16: 1176–1181.
Emig M, Saussele S, Wittor H, Weisser A, Reiter A, Willer A et al. Accurate and rapid analysis of residual disease in patients with CML using specific fluorescent hybridization probes for real time quantitative RT-PCR. Leukemia 1999; 13: 1825–1832.
Schoch C, Schnittger S, Bursch S, Gerstner D, Hochhaus A, Berger U et al. Comparison of chromosome banding analysis, interphase- and hypermetaphase-FISH, qualitative and quantitative PCR for diagnosis and for follow-up in chronic myeloid leukemia: a study on 350 cases. Leukemia 2002; 16: 53–59.
Hochhaus A, Reiter A, Saussele S, Reichert A, Emig M, Kaeda J . Molecular heterogeneity in complete cytogenetic responders after interferon-alpha therapy for chronic myelogenous leukemia: low levels of minimal residual disease are associated with continuing remission. German CML Study Group and the UK MRC CML Study Group. Blood 2000; 95: 62–66.
Matsushita M, Ikeda H, Kizaki M, Okamoto S, Ogasawara M, Ikeda Y et al. Quantitative monitoring of the PRAME gene for the detection of minimal residual disease in leukaemia. Br J Haematol 2001; 112: 916–926.
Marcucci G, Livak KJ, Bi W, Strout MP, Bloomfield CD, Caligiuri MA . Detection of minimal residual disease in patients with AML1/ETO-associated acute myeloid leukemia using a novel quantitative reverse transcription polymerase chain reaction assay. Leukemia 1998; 12: 1482–1489.
Degan M, Mazzocco FT, Di Francia R, Rossi FM, Pinto A, Gattei V . Normalizing complementary DNA by quantitative reverse transcriptase-polymerase chain reaction of beta2-microglobulin: molecular monitoring of minimal residual disease in acute promyelocytic leukemia. Diagn Mol Pathol 2000; 9: 98–109.
Radich JP, Gooley T, Bryant E, Chauncey T, Clift R, Beppu L et al. The significance of bcr-abl molecular detection in chronic myeloid leukemia patients ‘late’, 18 months or more after transplantation. Blood 2001; 98: 1701–1707.
Krauter J, Hoellge W, Wattjes MP, Nagel S, Heidenreich O, Bunjes D et al. Detection and quantification of CBFB/MYH11 fusion transcripts in patients with inv(16)-positive acute myeloblastic leukemia by real-time RT-PCR. Genes Chromosomes Cancer 2001; 30: 342–348.
Cassinat B, Zassadowski F, Balitrand N, Barbey C, Rain JD, Fenaux P et al. Quantitation of minimal residual disease in acute promyelocytic leukemia patients with t(15;17) translocation using real-time RT-PCR. Leukemia 2000; 14: 324–328.
Ballerini P, Landman Parker J, Laurendeau I, Olivi M, Vidaud M, Adam M et al. Quantitative analysis of TEL/AML1 fusion transcripts by real-time RT-PCR assay in childhood acute lymphoblastic leukemia. Leukemia 2000; 14: 1526–1528.
Marcucci G, Caligiuri MA, Dohner H, Archer KJ, Schlenk RF, Dohner K et al. Quantification of CBFbeta/MYH11 fusion transcript by real time RT-PCR in patients with INV(16) acute myeloid leukemia. Leukemia 2001; 15: 1072–1080.
Gabert J, Beillard E, van der Velden VHJ, Bi W, Grimwade D, Pallisgaard N et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction (RQ-PCR) of fusion gene transcripts for residual disease detection in leukemia – A Europe Against Cancer Program. Leukemia 2003; (in press).
van Dongen JJ, Macintyre EA, Gabert JA, Delabesse E, Rossi V, Saglio G et al. Standardized RT-PCR analysis of fusion gene transcripts from chromosome aberrations in acute leukemia for detection of minimal residual disease. Report of the BIOMED-1 concerted action: investigation of minimal residual disease in acute leukemia. Leukemia 1999; 13: 1901–1928.
Dirnhofer S, Berger C, Untergasser G, Geley S, Berger P . Human beta-actin retropseudogenes interfere with RT-PCR. Trends Genet 1995; 11: 380–381.
Arcari P, Martinelli R, Salvatore F . Human glyceraldehyde-3-phosphate dehydrogenase pseudogenes: molecular evolution and a possible mechanism for amplification. Biochem Genet 1989; 27: 439–450.
Kollia P, Stavroyianni N, Stamatopoulos K, Zoi K, Viniou N, Mantzourani M et al. Molecular analysis of transferrin receptor mRNA expression in acute myeloid leukaemia. Br J Haematol 2001; 115: 19–24.
Sposi NM, Cianetti L, Tritarelli E, Pelosi E, Militi S, Barberi T et al. Mechanisms of differential transferrin receptor expression in normal hematopoiesis. Eur J Biochem 2000; 267: 6762–6774.
Willenbrink W, Halaschek J, Schuffenhauer S, Kunz J, Steinkasserer A . Cyclophilin A, the major intracellular receptor for the immunosuppressant cyclosporin A, maps to chromosome 7p112-p13: four pseudogenes map to chromosomes 3, 10, 14, and 18. Genomics 1995; 28: 101–104.
Kidd V, Lion T . Debate round-table. Appropriate controls for RT-PCR. Leukemia 1997; 11: 871–881.
Stentoft J, Pallisgaard N, Kjeldsen E, Holm MS, Nielsen JL, Hokland P . Kinetics of BCR-ABL fusion transcript levels in chronic myeloid leukemia patients treated with STI571 measured by quantitative real-time polymerase chain reaction. Eur J Haematol 2001; 67: 302–308.
Cross NC, Feng L, Chase A, Bungey J, Hughes TP, Goldman JM . Competitive polymerase chain reaction to estimate the number of BCR-ABL transcripts in chronic myeloid leukemia patients after bone marrow transplantation. Blood 1993; 82: 1929–1936.
Lyon MF . X-chromosome inactivation and human genetic disease. Acta Paediatr Suppl 2002; 91: 107–112.
Lupberger J, Kreuzer KA, Baskaynak G, Peters UR, le Coutre P, Schmidt CA . Quantitative analysis of beta-actin, beta-2-microglobulin and porphobilinogen deaminase mRNA and their comparison as control transcripts for RT-PCR. Mol Cell Probes 2002; 16: 25–30.
Hamalainen HK, Tubman JC, Vikman S, Kyrola T, Ylikoski E, Warrington JA et al. Identification and validation of endogenous reference genes for expression profiling of T helper cell differentiation by quantitative real-time RT-PCR. Anal Biochem 2001; 299: 63–70.
Acknowledgements
Additional contributors not listed in the authors list: M González, Servicio de Hematologia, Hospital Clinico Universitario, Salamanca, Spain; G Barbany, Department of Medical Sciences, Uppsala University Hospital, Uppsala, Sweden; F Pane, CEINGE-DasMelab, Universita di Napoli Federico II, Napoli, Italy; Hélène Cavé, Lab de Biochimie Génétique, Hopital Robert Debré, Paris, France; J Aerts, Experimentele Laboratoriumgeneeskunde, Leuven, Belgium; M Lafage-Pochitaloff, Laboratoire de Cytogénétique Hématologique, Institut Paoli Calmettes, Marseille, France; A Porwit, Department of Pathology, Karolinska Hospital, Stockholm, Sweden. We also thank the other laboratories of the Europe Against Cancer Network for their support and discussions. We thank W Mayser for his logistic support during meetings, K Livak and X Thirion for useful discussions, N Brochard for secretarial assistance and D Grimwade for critical review of the manuscript. This work was supported by the SANCO European Commission (no. SI2.129294 (99CVF2-016) and Applied Biosystems (Foster City, CA, USA). Additional support was provided by national grants: ARC no. 5484, Ligue Contre le Cancer, Dutch Cancer Society/Koningin Wilhelmina Fonds (Grant SNWLK 2000-2268); Associazione Italiana per la Ricerca sul Cancero (AIRC), MURST.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information Supplementary Information accompanies the paper on Leukemia website (http://www.nature.com/leu).
Supplementary information
Rights and permissions
About this article
Cite this article
Beillard, E., Pallisgaard, N., van der Velden, V. et al. Evaluation of candidate control genes for diagnosis and residual disease detection in leukemic patients using ‘real-time’ quantitative reverse-transcriptase polymerase chain reaction (RQ-PCR) – a Europe against cancer program. Leukemia 17, 2474–2486 (2003). https://doi.org/10.1038/sj.leu.2403136
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2403136