Abstract
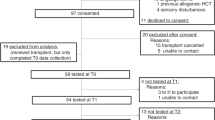
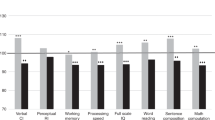
Neuropsychological deficits are potential side effects of hematopoietic stem cell therapy (HSCT). Systematic data on the long-term course of and therapeutic options for these consequences are limited. One hundred fifty-seven patients were screened for cognitive deficits following HSCT for malignant diseases at an in-patient oncologic rehabilitation clinic. Patients showing evidence of impairment were randomly assigned to one of two training groups: individualized PC-supported training or neuropsychological group therapy. The control group consisted of patients who received no specific training. During in-patient rehabilitation, the results of a comprehensive neuropsychological test battery improved significantly in all three groups, and no specific intervention effects were identified. Neuropsychological deficits were still evident in a subgroup of patients 6 months later. Correlation between neuropsychological testing and patients' self-evaluation of cognitive functioning in daily life was generally low. Sustained attention and verbal-semantic memory played the main role for self-appraisal and in the designation as ‘neuropsychologically impaired’. In conclusion, a substantial number of patients revealed evidence of cognitive deficits a long time after HSCT. There is a need for more studies and for the development of differentiated rehabilitative measures for such therapeutic consequences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Keime-Guibert F, Napolitano M, Delattre JY . Neurological complications of radiotherapy and chemotherapy. J Neurol 1998; 245: 695–708.
Shah AK . Cyclosporine A neurotoxicity among bone marrow transplant recipients. Clin Neuropharmacol 1999; 2: 67–73.
Tuxen MK, Hansen SW . Neurotoxicity secondary to antineoplastic drugs. Cancer Treat Rev 1994; 20: 191–214.
Verstappen CCP, Heimans JJ, Hoekman K, Postma TJ . Neurotoxic complications of chemotherapy in patients with cancer. Drugs 2003; 63: 1549–1563.
Butler RW, Copeland DR . Neuropsychological effects of central nervous system prophylactic treatment in childhood leukemia: methodological considerations. J Pediat Psychol 1993; 18: 319–338.
Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE . Late neurocognitive sequelae in survivors of brain tumors in childhood. Lancet Oncol 2004; 5: 399–408.
Waber DP, Tarbell NJ, Kahn CM, Gelber RD, Sallan SE . The relationship of sex and treatment modality to neuropsychologic outcome in childhood acute lymphoblastic leukemia. J Clin Oncol 1992; 10: 810–817.
Shusterman S, Meadows AT . Long term survivors of childhood leukemia. Curr Opin Hematol 2000; 7: 217–222.
Arvidson J, Kihlgren M, Hall C, Lönnerholm G . Neuropsychological functioning after treatment for hematological malignancies in childhood, including autologous bone marrow transplantation. Ped Hematol Oncol 1999; 16: 9–21.
Butler RW, Copeland DR . Attentional processes and their remediation in children treated for cancer: a literature review and the development of a therapeutic approach. J Int Neuropsychol Soc 2002; 8: 115–124.
Iuvone L, Mariotti P, Colosimo C, Guzzetta F, Ruggiero A, Riccardi R . Long-term cognitive outcome, brain computed tomography scan, and magnetic resonance imaging in children cured for acute lymphoblastic leukemia. Cancer 2002; 95: 2562–2570.
Van Dongen-Melman JEWM, De Groot A, Van Dongen JJM, Verhulst FC, Hählen K . Cranial irradiation is the major cause of learning problems in children treated for leukemia and lymphoma: a comparative study. Leukemia 1997; 11: 1197–1200.
Kaleita TA, Reaman GH, MacLean WE, Sather HN, Whitt JK . Neurodevelopmental outcome of infants with acute lymphoblastic leukemia: a Children's Cancer Group report. Cancer 1999; 85: 1859–1865.
Leahy AM, Teunissen H, Friedman DL, Moshang T, Lange BJ, Meadows AT . Late effects of chemotherapy compared to bone marrow trasnplantation in the treatment of pediatric acute myeloid leukemia and myelodysplasia. Med Pediatr Oncol 1999; 17: 167–171.
Reddy AT, Witek K . Neurologic complications of chemotherapy for children with cancer. Curr Neurol Neurosc Rep 2003; 3: 137–142.
Jenney MEM, Levitt GA . The quality of survival after childhood cancer. Eur J Cancer 2002; 38: 1241–1250.
Brouwers P, Poplack D . Memory and learning sequelae in long-term survivors of acute lymphoblastic leukemia: association with attention deficits. Am J Pediatr Hematol Oncol 1990; 12: 174–181.
Rodgers J, Horrocks J, Britton PG, Kernahan J . Attentional ability among survivors of leukemia. Arch Dis Child 1999; 80: 318–323.
Mirsky A, Anthony B, Duncan C, Ahearn M, Kellan S . Analysis of elements of attention: a neuropsychological approach. Neuropsychol Rev 1991; 2: 109–145.
Aaronson NK, Meyerowitz BE, Bard M, Bloom JR, Fawzy FI, Feldstein M et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a qualitiy-of-life instrument for use in international clinical trials in oncology. J Nat Cancer Inst 1993; 85: 365–376.
Smets EMA, Garssen B, Bonke B, De Haes JCJM . The Multidimensional Fatigue Inventory (MFI): psychometric qualities of an instrument to assess fatigue. J Psychosom Res 1995; 39: 315–325.
Herrmann CH, Buss U, Snaith RP . Hospital Anxiety and Depression Scale—Deutsche Version (HADS-D). Huber: Bern, Switzerland, 1995.
Zimmermann P, Messner C, Poser U, Sedelmaier P . Ein Fragebogen erlebter Defizite der Aufmerksamkeit (Questionnaire of Self-Perceived Deficits in Attention: FEDA) Unpublished manuscript. University of Freiburg: Germany, 1991.
Zimmermann P, Fimm B . Testbatterie zur Aufmerksamkeitsprüfung (Test Battery for Attentional Performance: TAP; Version 1.7). Psytest: Würselen, Germany, 2001.
Wilson BA, Cockburn J, Baddeley AD . Rivermead Behavioral Memory Test. Thames Valley Test Company: Bury St Edmunds, 1985 (German adaption: Beckers K, Behrends U, Canavan A. Neurologisches Therapie Centrum: Düsseldorf, Germany 1992).
Wechsler D . Wechsler Memory Scale—Revised Form (WMS-R). The Psychological Corporation: San Antonio, 1987 (German adaption: Härting C, Markowitsch HJ, Neufeld H, Calabrese P, Deisinger K, Kessler J. Huber: Bern, Switzerland, 2000).
Bäumler G . Der Lern- und Gedächtnistest LGT-3 (Learning and Memory Test). Hogrefe: Göttingen, Germany, 1974.
Bernabeu Verdu J, Lopez Luengo B, Fournier de Castillo C, Canete Nieto A, Suarez Rodriguez J, Castel Sanchez V . Attention process training application within an intervention project on attentional processes in children with cancer. Revista Neurol 2004; 38: 482–486.
Butler RW, Mulhern RK . Neurocognitive interventions for children and adolescents surviving cancer. J Pediatr Psychol 2005; 30: 65–78.
Andrykowski MA, Henslee PJ, Farral MG . Physical and psychosocial functioning of adult survivors of allogeneic bone marrow transplantation. Bone Marrow Transplant 1989; 4: 75–81.
Syrjala KL, Chapko MK, Vitaliano PP, Cummings C, Sullivan KM . Recovery after allogeneic marrow transplantation: prospective study of predictors of long-term physical and psychosocial functioning. Bone Marrow Transplant 1993; 11: 319–327.
Parth P, Dunlap WP, Kennedy RS, Lane NE, Ordy JM . Motor and cognitive testing of bone marrow transplant patients after chemoradiotherapy. Percept Mot Skills 1989; 68: 1227–1241.
Meyers CA, Weitzner M, Byrne K, Valentine A, Champlin RE, Przepiorka D . Evaluation of the neurobehavioral functioning of patients before, during, and after bone marrow transplantation. J Clin Oncol 1994; 12: 820–826.
Andrykowski MA, Schmitt FA, Gregg ME, Brady MJ, Lamb DG, Henslee-Downey PJ . Neuropsychologic impairment in adult bone marrow transplant candidates. Cancer 1992; 70: 2288–2297.
Harder H, Cornelissen JJ, Van Gool AR, Duivenvoorden HJ, Eijkenboom WMH, van den Bent MJ . Cognitive functioning and quality of life in long-term adult survivors of bone marrow transplantation. Cancer 2002; 95: 183–192.
Sostak P, Padovan CS, Yousry TA, Ledderose G, Kolb HJ, Straube A . Prospective evaluation of neurological complications after allogeneic bone marrow transplantation. Neurology 2003; 60: 842–848.
Ylikoski R, Ylikoski A, Erkinjuntti T, Sulkava R, Raininko R, Tilvis R . White matter changes in healthy elderly persons correlate with attention and speed of mental processing. Arch Neurol 1993; 50: 818–824.
Syrjala KL, Dikmen SS, Langer S, Roth-Roemer S, Abrams J . Neuropsychological changes from pretransplant to one year in patients receiving myeloablative allogeneic hematopoietic cell transplant. Blood 2004; 104: 3386–3392.
Booth-Jones M, Jacobsen PB, Ransom S, Soety E . Characteristics and correlates of cognitive functioning following bone marrow transplantation. Bone Marrow Transplant 2005; 36: 695–702.
Lezak MD, Howieson DB, Loring DW . Neuropsychological assessment, 4th edn. Oxford University Press: New York, NY, 2004.
Meyers CA . Neurocognitive dysfunction in cancer patients. Oncology 2000; 14: 75–79.
Tannock IF, Ahles TA, Ganz PA, van Dam FS . Cognitive impairment associated with chemotherapy for cancer: report of a workshop. J Clin Oncol 2004; 22: 2233–2239.
Meier RJ, Benton AL, Diller L (eds). Neuropsychological Rehabilitation. Churchill Livingstone: Edinburgh, 1987.
Sohlberg MM, Mateer CA . Introduction to cognitive rehabilitation. Theory and practice. Guilford Press: New York, NY, 1989.
Bartsch HH, Weis J, Mumm A . Stationäre Rehabilitation und ambulante Nachsorge bei allogener Stammzelltransplantation. Unpublished study report. Tumor Biology Center: Freiburg, Germany, 2006.
Weis J, Bartsch HH, Nagel GA, Unger C . Psychosocial care for cancer patients: a new holistic psychosomatic approach in acute care and rehabilitation. Psycho-Oncology 1996; 5: 51–54.
Poppelreuter M, Weis J, Külz AK, Tucha O, Lange KW, Bartsch HH . Cognitive dysfunction and subjective complaints of cancer patients: a cross-sectional study in a cancer rehabilitation center. Eur J Cancer 2004; 40: 43–49.
Sturm W, Willmes K, Orgass B, Hartje W . Do specific attention deficits need specific training? Neuropsychol Rehab 1997; 7: 81–103.
Sturm W . Evaluation in therapeutical contexts: attentional and neglect disorders. Eur Rev Appl Psychol 1996; 46: 207–215.
Acknowledgements
This study was supported by the Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF, Berlin, Germany, Grant number 02821) and the German Pension Fund (Deutsche Rentenversicherung-Bund, Berlin, Germany).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Poppelreuter, M., Weis, J., Mumm, A. et al. Rehabilitation of therapy-related cognitive deficits in patients after hematopoietic stem cell transplantation. Bone Marrow Transplant 41, 79–90 (2008). https://doi.org/10.1038/sj.bmt.1705884
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1705884
Keywords
This article is cited by
-
Cognitive adverse effects of chemotherapy and immunotherapy: are interventions within reach?
Nature Reviews Neurology (2022)
-
Computerized cognitive training in post-treatment hematological cancer survivors: a feasibility study
Pilot and Feasibility Studies (2021)
-
Late cognitive outcomes among allogeneic stem cell transplant survivors: follow-up data from a 6-year longitudinal study
Supportive Care in Cancer (2021)
-
Neuropsychologische Beeinträchtigungen nach Stammzelltransplantation
Der Onkologe (2016)
-
A systematic review and meta-analysis of changes in cognitive functioning in adults undergoing hematopoietic cell transplantation
Bone Marrow Transplantation (2013)