Summary:
Autologous HCT patients often have poor oral intake for 2–4 weeks post transplant. To compare outcomes between patients provided prophylactic total parenteral nutrition (TPN) or an oral diet (OD), 55 well nourished breast cancer/ hematopoietic cell transplantation (HCT) patients were randomized to TPN (n=27), beginning day −1, or OD (n=28). Parameters studied include length of stay (LOS), engraftment, infections, survival, weight, anthropometrics, handgrip strength, and quality of life (QOL) In all, 50% of OD patients were given TPN due to poor oral intake for 10 consecutive days. No significant differences were found between the groups for any of the above parameters except weight and anthropometrics, which were better maintained in the TPN group than the OD group. Trends were seen for increased infections, more stable handgrip strength, and improved QOL in the TPN group vs the OD group. Prophylactic TPN did result in a more intact nutritional status and preservation of lean body mass post transplant but did not impact LOS or survival when compared to OD. For this reason, TPN should be reserved for autologous HCT patients with pretransplant nutritional depletion, complications post transplant, or prolonged poor oral intake. These results should not be extrapolated to allogeneic HCT patients but are likely applicable to other well nourished autologous HCT patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Aker SN . Bone marrow transplantation: nutrition support and monitoring. In: Bloch AS (ed.). Nutrition Management of the Cancer Patient. Aspen Publishers: Rockville, MD, 1990, pp 199–225.
Herrmann VM, Petruska PJ . Nutrition support in bone marrow transplant recipients. Nutr Clin Pract 1993; 8: 19–27.
Weisdorf SA, Schwarzenberg SJ . Nutritional support of bone marrow transplant recipients. In: Forman SJ, Blume KG, Thomas ED (eds). Bone Marrow Transplantation. Blackwell Scientific Publications: Boston, MA, 1994, pp 327–336.
Weisdorf SA, Lysne J, Wind D et al. Positive effect of prophylactic total parenteral nutrition on long-term outcome of bone marrow transplantation. Transplantation 1987; 43: 833–838.
Dicato M . High-dose chemotherapy in breast cancer: where are we now? Semin Oncol 2002; 29: 16–20.
Baynes RD, Dansey RD, Klein JL et al. High-dose chemotherapy and hematopoietic stem cell transplantation for breast cancer: past or future? Semin Oncol 2001; 28: 377–388.
Carella AM, Beltrami C, Lerma E et al. Combined use of autografting and non-myeloablative allografting for the treatment of hematologic malignancies and metastatic breast cancer. Cancer Treat Res 2002; 110: 101–102.
Pecora AL, Lazarus HM, Stadtmauer EA et al. Effect of induction chemotherapy and tandem cycles of high-dose chemotherapy on outcomes in autologous stem cell transplant for metastatic breast cancer. Bone Marrow Transplant 2001; 27: 1245–1253.
Hamwi GJ . Changing dietary concepts. In: Danowski TS (ed.). Diabetes Mellitus: Diagnosis and Treatment, American Diabetes Association, Inc.: New York, Vol. 1, 1964, pp 73–78.
Harris JA, Benedict FG . A Biometric Study of Basal Metabolism in Man. Publication No. 279. Carnegie Institute: Washington, DC, 1919.
Kushner RF, Wall-Alonso E, Alverdy J . Obesity. In: Merritt RJ (ed.). The A.S.P.E.N. Nutrition Support Practice Manual. A.S.P.E.N.: Silver Springs, MD, 1998, pp 21/1–21/11.
Taylor SE, Lichtman RR, Wood JV et al. Illness-related and treatment-related factors in psychological adjustment to breast cancer. Cancer 1985; 55: 2506–2513.
Taylor SE, Lichtman RR, Wood JV et al. Breast self-examination among diagnosed breast cancer patients. Cancer 1984; 54: 2528–2532.
McNair DM, Lorr M, Droppleman LF . Edits Manual for the Profile of Mood States. EdITS/Educational and Industrial Testing Service: San Diego, CA, 1992, p 23.
Szeluga DJ, Stuart RK, Brookmeyer R et al. Nutritional support of bone marrow transplant recipients: randomized clinical trial comparing total parenteral nutrition to an enteral feeding program. Cancer Res 1987; 47: 3309–3316.
Strasser SI, Shulman HM, McDonald GB . Cholestasis after hematopoietic cell transplantation. Clin Liver Dis 1999; 3: 651–668.
Fleming CR . Hepatobiliary complications in adults receiving nutrition support. Dig Dis 1994; 12: 191–198.
Geibig CB, Ponting Owens J, Mirtallo JM et al. Parenteral nutrition for marrow transplant recipients: evaluation of an increased nitrogen dose. J Parenter Enteral Nutr 1991; 15: 184–188.
Keller U, Kraenzlin ME, Gratwohl A et al. Protein metabolism assessed by 1-13C leucine infusions in patients undergoing bone marrow transplantation. J Parenter Enteral Nutr 1990; 14: 480–484.
Cheney CL, Abson KG, Aker SN et al. Body composition changes in marrow transplant recipients receiving TPN. Cancer 1987; 59: 1515–1519.
Figueiredo FA, Dickson ER, Pasha TM et al. Utility of standard nutritional parameters in detecting body cell mass depletion in patients with end-stage liver disease. Liver Transplant 2000; 6: 575–581.
Vaz M, Thangam S, Prabhu A et al. Maximal voluntary contraction as a functional indicator of adult chronic undernutrition. Br J Nutr 1996; 76: 9–15.
Efthimiou J, Fleming J, Gomes C et al. The effect of supplementary oral nutrition in poorly nourished patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1988; 137: 1075–1082.
Johnson AM . Low levels of plasma proteins: malnutrition or inflammation? Clin Chem Lab Med 1999; 37: 91–96.
Vanek VW . The use of serum albumin as a prognostic or nutritional marker and the pros and cons of IV albumin therapy. Nutr Clin Pract 1998; 13: 110–122.
Boosalis MG, Ott L, Levine AS et al. Relationship of visceral proteins to nutritional status in chronic and acute stress. Crit Care Med 1989; 17: 741–747.
Deeg HJ, Seidel K, Bruemmer B et al. Impact of patient weight on non-relapse mortality after marrow transplantation. Bone Marrow Transplant 1995; 15: 461–468.
Perioperative total parenteral nutrition in surgical patients. The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. N Engl J Med 1991; 325: 525–532.
Buzby GP . Overview of randomized clinical trials of total parenteral nutrition for malnourished surgical patients. World J Surg 1993; 17: 173–177.
Bozzetti F, Gavazzi C, Miceli R et al. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: a randomized, clinical trial. J Parenter Enteral Nutr 2000; 24: 7–14.
De Cicco M, Panarello G, Fantin D et al. Parenteral nutrition in cancer patients receiving chemotherapy: effects on toxicity and nutritional status. J Parenter Enteral Nutr 1993; 17: 513–518.
Charuhas PM, Fosberg KL, Bruemmer B et al. A double-blind randomized trial comparing outpatient parenteral nutrition with intravenous hydration: effect on resumption of oral intake after marrow transplantation. J Parenter Enteral Nutr 1997; 21: 157–161.
Carlson LE, Koski T, Glück S . Longitudinal effects of high-dose chemotherapy and autologous stem cell transplantation on quality of life in the treatment of metastatic breast cancer. Bone Marrow Transplant 2001; 27: 989–998.
Hann DM, Garovoy N, Finkelstein B et al. Fatigue and quality of life in breast cancer patients undergoing autologous stem cell transplantation: a longitudinal comparative study. J Pain Symptom Manage 1999; 17: 311–319.
Rock CL, Flatt SW, Newman V et al. Factors associated with weight gain in women after diagnosis of breast cancer. Women's Healthy Eating and Living Study Group. J Am Diet Assoc 1999; 99: 1212–1221.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roberts, S., Miller, J., Pineiro, L. et al. Total parenteral nutrition vs oral diet in autologous hematopoietic cell transplant recipients. Bone Marrow Transplant 32, 715–721 (2003). https://doi.org/10.1038/sj.bmt.1704204
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704204
Keywords
This article is cited by
-
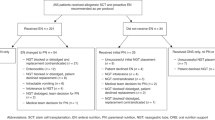
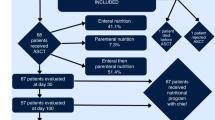
Effect of malnutrition-driven nutritional support protocol on clinical outcomes in autologous stem cell transplantation patients
Supportive Care in Cancer (2021)
-
Could enteral nutrition improve the outcome of patients with haematological malignancies undergoing allogeneic haematopoietic stem cell transplantation? A study protocol for a randomized controlled trial (the NEPHA study)
Trials (2015)
-
Impact of clinical pharmacist-based parenteral nutrition service for bone marrow transplantation patients: a randomized clinical trial
Supportive Care in Cancer (2013)
-
Factors influencing catheter-related infections in the Dutch multicenter study on high-dose chemotherapy followed by peripheral SCT in high-risk breast cancer patients
Bone Marrow Transplantation (2008)
-
Total parenteral nutrition and hematopoietic stem cell transplantation: an expensive placebo?
Bone Marrow Transplantation (2005)