Abstract
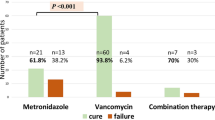
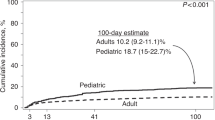
Autologous peripheral blood progenitor cell (PBPC) transplant recipients frequently receive multiple antibiotics for neutropenic fever in addition to high-dose chemotherapy. Although there are many possible causes for diarrhea in this population, empiric therapy for possible C. difficile colitis is common in some centers. This study sought to define the frequency of diarrhea and of a positive C. difficile toxin assay in PBPC transplant recipients. Data were collected on 80 patients enrolled in a randomized trial of two different antibiotic regimens during PBPC transplant. Data included the presence or absence of diarrhea, all microbiologic studies performed during the transplant admission, and all antimicrobials administered during the transplant admission. Of 80 patients enrolled, 61 (76.3%) developed diarrhea. Only 3/61 (4.9%) had a positive C. difficile toxin assay. A total of 122 C. difficile toxin assays were performed; for each positive C. difficile assay, 41 stool samples were analyzed. Twenty courses of oral metronidazole (18/20 empiric) and 10 courses of oral vancomycin (8/10 empiric) were given. A total of 25 of 61 patients with diarrhea (41%) received therapy for possible C. difficile. Diarrhea is common during autologous PBPC transplant but a positive C. difficile assay is uncommon. The practice of empiric therapy for C. difficile in this population in a non-outbreak setting should be re-evaluated. Bone Marrow Transplantation (2000) 25, 67–69.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Bartlett JG . Clostridium difficile: clinical considerations Rev Infect Dis 1990 12: (Suppl. 2) S243–S251
McFarland LV, Mulligan ME, Kwok RYY, Stamm WE . Nosocomial acquisition of Clostridium difficile infection New Engl J Med 1989 320: 204–210
Kelly CP, Pothoulakis C, LaMont JT . Clostridium difficile colitis New Engl J Med 1994 330: 257–262
Nath SK, Thornley JH, Kelly M et al. A sustained outbreak of Clostridium difficile in a general hospital: persistence of a toxigenic clone in four units Infect Control Hosp Epidemiol 1994 15: 382–389
Fekety R . Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis Am J Gastroenterol 1997 92: 739–750
Johnson S, Gerding DN . Clostridium difficile-associated diarrhea Clin Infect Dis 1998 26: 1027–1036
Grundfest-Broniatowski S, Quader M, Alexander F et al. Clostridium difficile colitis in the critically ill Dis Colon Rectum 1996 39: 619–623
Centers for Disease Control and Prevention. Recommendations for preventing the spread of vancomycin resistance: recommendations of the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR 44 (RR-12) 1995 1–13
Anglin AM, Klym B, Byers KE et al. Effect of a vancomycin restriction policy on ordering practices during an outbreak of vancomycin-resistant Enterococcus faecium Arch Intern Med 1997 157: 1132–1136
Gerding DN . Is there a relationship between vancomycin-resistant enterococcal infection and Clostridium difficile infection? Clin Infect Dis 1997 25: (Suppl. 2) S206–S210
Bilgrami S, Feingold JM, Dorsky D et al. Incidence and outcome of Clostridium difficile infection following autologous peripheral blood stem cell transplantation Bone Marrow Transplant 1999 23: 1039–1042
Kavan P, Sochor M, Nyc O et al. Pseudomembraneous clostridium after autologous bone marrow transplantation Bone Marrow Transplant 1998 21: 521–523
Cox GJ, Matsui SM, Lo RS et al. Etiology and outcome of diarrhea after marrow transplantation: a prospective study Gastroenterology 1994 107: 1398–1407
Yolken RH, Bishop CA, Townsend TR et al. Infectious gastroenteritis in bone-marrow-transplant recipients New Engl J Med 1982 306: 1010–1012
Blakey JL, Barnes GL, Bishop RF, Ekert H . Infectious diarrhea in children undergoing bone-marrow transplantation Aust NZ J Med 1989 19: 31–36
Aplin MS, Weiner R, Graham Pole J et al. Enterocolitis in allogeneic marrow transplant patients (abstract) Exp Hematol 1990 18: 696
Avery R, Pohlman B, Longworth D et al . A randomized prospective trial of single daily dose vancomycin and tobramycin plus oral ciprofloxacin versus standard triple antibiotics in febrile neutropenic recipients of autologous progenitor cell transplants. 15th Annual Meeting, American Society of Transplant Physicians, Chicago, May 1997, Abstr. No. 530
Knapp CC, Sandin RL, Hall GS et al. Comparison of Vidas Clostridium difficile toxin-A assay to cytotoxin-B tissue culture assay for the detection of toxins of C. difficile Diagn Microbiol Infect Dis 1993 17: 7–12
Lucas GM, Lechtzin N, Puryear DW et al. Vancomycin-resistant and vancomycin-suspectible enterococcal bacteremia: comparison of clinical features and outcomes Clin Infect Dis 1998 26: 1127–1133
Mossad SB, Longworth DL, Goormastic M et al. Early infectious complications in autologous bone marrow transplantation: a review of 219 patients Bone Marrow Transplant 1996 18: 265–271
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Avery, R., Pohlman, B., Adal, K. et al. High prevalence of diarrhea but infrequency of documented Clostridium difficile in autologous peripheral blood progenitor cell transplant recipients. Bone Marrow Transplant 25, 67–69 (2000). https://doi.org/10.1038/sj.bmt.1702086
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702086
Keywords
This article is cited by
-
Stufenweise Behandlung bei therapiebedingter Diarrhö
best practice onkologie (2024)
-
Diarrheal Morbidity During Hematopoietic Cell Transplantation: The Diagnostic Yield of Stool Cultures
Infectious Diseases and Therapy (2021)
-
Diagnosis and management of gastrointestinal complications in adult cancer patients: 2017 updated evidence-based guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO)
Annals of Hematology (2018)
-
Incidence and outcomes of Clostridium difficile-associated disease in hematopoietic cell transplant recipients
International Journal of Hematology (2014)
-
Antimicrobial therapy of febrile complications after high-dose chemotherapy and autologous hematopoietic stem cell transplantation—guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO)
Annals of Hematology (2012)