Abstract
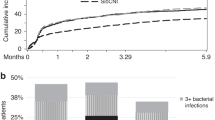
Infectious complications after autologous peripheral blood progenitor cell transplantation (PBPCT) have been reported in a few studies including small patient numbers. The present study was performed to assess the incidence, types, outcome and factors affecting early and late infections in 150 patients aged 18 to 68 years (median 46.5) who underwent high-dose therapy, with G-CSF. Patients were kept in reverse isolation rooms and received antimicrobial chemoprophylaxis with oral quinolone and fluconazole. One hundred and fifteen patients (76.7%) developed fever (median 3 days, range 1–29); 20 patients (55.5%) had Gram-positive and 13 (36.2%) Gram-negative bacterial infections. There were no fungal infections or infection-related deaths. Mucositis grade II–IV (P = 0.0001; odds ratio 3.4) and >5 days on ANC<100/μl (P = 0.0001; odds ratio 2.3) correlated with development of infection. Only days with ANC <100/μl affected infection outcome (P = 0.0024) whereas the antibiotic regimen did not. After day +30 there were four cases of bacterial pneumonitis (2.7%), one case of fatal CMV pneumonia (0.8%) and 20 of localized VZV infection (13.3%). Reduction of neutropenia duration with PBPCT and G-CSF is not enough to prevent early infectious complications since only a few days of severe neutropenia and mucositis are related to development of early infections. However, no infection-related deaths were seen. Although Gram-positive organisms were the major cause of bacteremia, a glycopeptide in the empirical antibiotic regimen did not affect infection outcome. In PBPCT recipients, early and late opportunistic infections were notably absent, which was at variance with what was seen with bone marrow recipients. Efforts should be made to prevent mucositis and neutropenia and identify new strategies of antibacterial prophylaxis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Offidani, M., Corvatta, L., Olivieri, A. et al. Infectious complications after autologous peripheral blood progenitor cell transplantation followed by G-CSF. Bone Marrow Transplant 24, 1079–1087 (1999). https://doi.org/10.1038/sj.bmt.1702033
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1702033
Keywords
This article is cited by
-
The D-index is not correlated with invasive fungal infection during the early-post engraftment phase among allogeneic hematopoietic stem cell transplant recipients
International Journal of Hematology (2020)
-
Recovery of mucosal-associated invariant T cells after myeloablative chemotherapy and autologous peripheral blood stem cell transplantation
Clinical and Experimental Medicine (2016)
-
Incidence, risk factors, and outcome of bacteremia following autologous hematopoietic stem cell transplantation in 720 adult patients
Annals of Hematology (2014)
-
Pegfilgrastim reduces the length of hospitalization and the time to engraftment in multiple myeloma patients treated with melphalan 200 and auto-SCT compared with filgrastim
Annals of Hematology (2011)
-
Febrile mucositis in haematopoietic SCT recipients
Bone Marrow Transplantation (2009)