Abstract
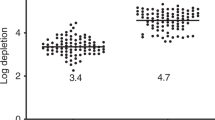
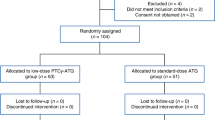
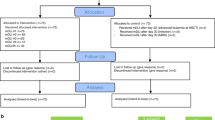
From March 1994 to September 1997, 30 patients with hematological malignancies (12 ANLL, 10 CML, four ALL and four multiple myeloma) received HLA-identical allogeneic bone marrow transplants with the marrow graft selectively depleted of CD4+ lymphocytes and the CD8+ cell content adjusted to 1 × 106/kg. Total depletion of CD4+ and partial depletion of CD8+ lymphocytes was carried out by an immunomagnetical method. All patients were considered as having high risk for developing GVHD by at least one of the following criteria: patient age >35 years; donor age >35 years; donor multiparity or marrow from an unrelated donor. Twenty-four cases received marrow from an identical sibling and six from an unrelated donor. In order to assess the role of methotrexate (MTX) in addition to cyclosporin A (CsA) after transplant, patients were randomly assigned to received either CsA alone (n = 15) or CsA plus a short course of MTX (n = 15). No case of primary graft failure was observed, but two patients developed late graft failure. Six patients presented grade II acute GVHD and no case of severe III–IV GVHD was seen. The actuarial probability of developing grade II–IV acute GVHD was 25.9 ± 9.6% for the entire population. Patients receiving post-transplant CsA + MTX had significantly less probability of acute GVHD than those receiving CsA exclusively (6.7 ± 6.4% vs 50.5 ± 17.8%, P = 0.03) and the schedule of post-transplant immunosuppression was the only factor associated with the incidence of acute GVHD in a multivariate analysis. The actuarial incidence of chronic GVHD for the entire population was 31.8 ± 12.5, and there was no significant difference between both groups with additional prophylaxis. Four patients with CML and three with ANLL relapsed: the actuarial probability of remaining in complete remission for all patients was 53.6 ± 17.3%. For patients with acute leukemia, the probability of remaining in complete remission did not differ significantly between those transplanted in first complete remission and those receiving a transplant in more advanced phases of the disease (87.5 ± 11.6% vs 72.9 ± 16.5%; P = 0.44). The incidence of mixed chimerism assessed by PCR was 34%. Nineteen patients are alive between 2 and 43 months post-transplant, the probability of overall survival being 57.8 ± 10.4%. Our data indicate that this method of selective T cell depletion is very effective in preventing acute GVHD in high risk patients, particularly when used in combination with post-transplant CsA + MTX.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Herrera, C., Torres, A., García-Castellano, J. et al. Prevention of graft-versus-host disease in high risk patients by depletion of CD4+ and reduction of CD8+ lymphocytes in the marrow graft. Bone Marrow Transplant 23, 443–450 (1999). https://doi.org/10.1038/sj.bmt.1701493
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1701493
Keywords
This article is cited by
-
Clinical-scale single-step CD4+ and CD8+ cell depletion for donor innate lymphocyte infusion (DILI)
Bone Marrow Transplantation (2008)
-
A comparison of an anti-CD25 immunotoxin, Ontak and anti-CD25 microbeads for their ability to deplete alloreactive T cells in vitro
Bone Marrow Transplantation (2006)