Abstract
Our objective was to determine if amphetamine improves visuospatial working memory, which is impaired in the schizophrenia spectrum and may be modulated by dopamine in prefrontal cortex. To this end, oral amphetamine (30 mg) was administered to 12 patients with schizophrenia spectrum personality disorders and 13 patients with other, nonschizophrenia-related personality disorders. Visuospatial working memory was assessed using the Dot test; a test in which subjects are asked to memorize and reproduce the position of a dot on a sheet of paper. Patients with schizophrenia spectrum personality disorders performed significantly worse than the comparison group in the placebo condition and showed significantly greater improvement after amphetamine, as compared to a nonschizophrenia-related personality disorder comparison group. Patients with greatest impairment at baseline improved most. Amphetamine tended to improve negative symptoms; whereas, positive symptoms remained unchanged. Amphetamine may improve visuospatial working memory in schizophrenia spectrum patients.
Similar content being viewed by others
Main
Cognitive impairment is a core abnormality found both in schizophrenia and in schizophrenia spectrum and is responsible for much of the functional impairment associated with schizophrenia (Green 1996). Atypical antipsychotic medications may ameliorate some of the cognitive deficits associated with schizophrenia (Green et al. 1997), but the mechanism of their action is not entirely understood. Improving cognitive function has important treatment implications, because cognitive impairment in schizophrenia may be a better predictor of daily functioning than symptom severity (Green 1996). A critical component of the cognitive dysfunction in both schizophrenia and the schizophrenia spectrum, the prototype of which is schizotypal personality disorder (SPD), is impaired working memory (Weinberger and Lipska 1995; Lees Roitman et al. 1996; Park and Holzman 1992; Park and McTigue 1997). Subjects with SPD (Lees Roitman et al. 1996; Park and McTigue 1997), as do schizophrenic patients (Park and Holzman 1992; Keefe et al. 1995), have shown deficits on a visuospatial working memory task.
There have been studies investigating cognitive enhancement after the effects of amphetamine in schizophrenia with mixed results (Daniel et al. 1991; Goldberg et al. 1991), but studies of schizophrenic patients may be confounded by psychotogenic effects of amphetamine in this population and prior or concurrent long-term administration of neuroleptic medications. SPD patients are less susceptible to psychosis, less severely ill, and less likely to have received antipsychotic medication and to have been institutionalized than patients with chronic schizophrenia. Cognitive impairment in SPD is less severe (Trestman et al. 1995) and may be more easily reversible (Siegel et al. 1996). Thus, these patients provide a unique population in which to evaluate new pharmacologic strategies aimed at improving cognition.
It seems that the schizophrenia spectrum may even extend beyond the borders of the full criteria for SPD (Siever et al. 1993). Family studies of schizophrenic patients have found attentional impairment in a Continuous Performance Task in their nonpsychotic relatives who do not meet full criteria for SPD (Keefe et al. 1997). Moreover, we have previously reported (Trestman et al. 1995) impaired cognitive function in DSM-III SPD patients (where four out of eight criteria must be present to meet the disorder; in contrast to DSM-III-R, where five of nine criteria must be present). Furthermore, there was no empirical basis for changing the threshold of 5/9 criteria in DSM-III-; rather, this change was based on the addition of a new criterion (LJS on DSM-III-R and DSM-IV subcommittee on personality disorders). In a reanalysis of cognitive performance on working memory (DOT test; Keefe et al. 1995) and the Continuous Performance Task (CPT-IP; Cornblatt et al. 1989) patients meeting 4/9 SPD criteria and paranoid personality disorder demonstrated impairment in these two tasks similar to those seen in patients who meet 5/9 criteria (i.e., full criteria for SPD in DSM-III-R) (Siever et al, unpublished data). Moreover, there is evidence from both phenomenologic and genetic data that link both SPD and paranoid personality disorder to schizophrenia (Kendler and Diehl 1993; Battaglia et al. 1995), whereas, there is conflicting evidence regarding the link between schizoid personality disorder and schizophrenia (Kendler and Gardner 1997; Keefe et al. 1997). For these reasons, we identified for this pilot study a schizophrenia spectrum personality disorder group in which patients met criteria for DSM-III-R SPD (n = 8); or met criteria for DSM-III-R paranoid personality disorder and four criteria for SPD (n = 4). Patients were included in the nonschizophrenia-related personality disorder group (n = 13) if they: (1) did not meet criteria for SPD; (2) did not meet criteria for paranoid personality disorder; and (3) met fewer than four criteria for SPD. These patients met criteria for the following DSM-III-R diagnoses: borderline personality disorder (n = 4); passive-aggressive personality disorder (n = 4); schizoid personality disorder (n = 3); narcissistic personality disorder (n = 2); antisocial personality disorder (n = 2); avoidant personality disorder (n = 2), and personality disorder not otherwise specified (n = 2) (the numbers add up to more than 13, because some patients met criteria for more than one personality disorder).
Studies suggest that dopamine may be implicated in the cognitive impairment of the schizophrenia spectrum. Working memory may be modulated by frontal dopaminergic activity primarily via the D1 receptor (Williams and Goldman-Rakic 1995). In schizophrenia, decreased homovanillic acid (HVA) has been associated with impaired cognitive performance (Kahn et al. 1994). In SPD, decreased plasma HVA has been associated with poor Wisconsin Card Sort Test (WCST) performance (Siever et al. 1993), a test of frontal lobe dysfunction. Thus, frontal hypodopaminergia may play a role in the pathogenesis of cognitive dysfunction in SPD, as in schizophrenia (Siever et al. 1993).
Amphetamine releases monoamines, particularly dopamine and norepinephrine, and blocks their reuptake. Preclinical studies show that moderate doses of amphetamine mainly activate D1 receptors (Ferger et al. 1994). In a previous study from our center, amphetamine improved WCST performance in SPD patients (Siegel et al. 1996) [three of whom (one SPD patient) are included in this report] . Working memory is one component of the WCST, in that performance of a test of verbal working memory (the Letter-Number span Test) accounts for the differences between normal and schizophrenic patients on the WCST (Gold et al. 1997). In this study, we evaluate working memory specifically and examine the effects of amphetamine on visuospatial working memory in patients with schizophrenia spectrum personality disorder. A measure of visuospatial working memory that is an analog of the delayed response test (Park and Holzman 1992) has been developed (The Dot test), and it has distinguished schizophrenic patients from normal control subjects (Keefe et al. 1995). This task involves a presentation of a dot at a specific position on standard size paper; subjects are then asked to reproduce it on a separate sheet. It is simple to administer, pharmacologic interventions on performance can be evaluated, and in our laboratory, SPD patients have shown impairment in this task, as compared to controls (Lees Roitman et al. 1996). We hypothesized that schizophrenia-related personality disorder patients would demonstrate working memory impairment (measured by increased distance error), as compared to the nonschizophrenia disorder personality disorder patients. We also hypothesized that schizophrenia spectrum personality disorder patients’ working memory would improve after amphetamine (as measured by a reduction in their distance error), as compared to placebo and to the nonschizophrenia-related personality disorder group; furthermore, neither group would evidence an increase in their psychotic-like symptoms after amphetamine; whereas, negative symptoms would improve after amphetamine.
METHODS
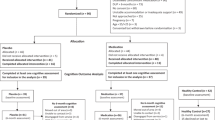
We studied 12 schizophrenia spectrum personality disorder patients (9 M/3 F; age 39.0 ± 10.5; education: 12.1 ± 3.0), and 13 with nonschizophrenia-related personality disorders (12 M/1 F; age: 44.3 ± 5.6; education: 16.3 ± 2.3) as defined above (p. 4). Patients were recruited from the outpatient clinics of the Mount Sinai and Bronx VA Medical Centers and diagnosed according to DSM-III-R using the Schedule for Affective Disorders and Schizophrenia and the Schedule for Interviewing DSM-III-R Personality Disorders (κ = 0.73 for SPD). Patients were medically healthy and free of psychoactive medication for at least 2 weeks, and had no history of substance dependence and no substance abuse in the preceding 6 months. Written informed consent was obtained, and all subjects participated as outpatients.
We administered amphetamine 30 mg/placebo in double-blind randomized fashion, with protocols separated by at least 2 days. Patients followed a low monoamine diet for 3 days before the study and fasted from midnight the night before. At 10 A.M. d-amphetamine 30 mg/placebo was given orally. One hour later, the Dot test of visuospatial working memory was administered, wherein subjects were shown a dot at a specific position on standard size paper presented in landscape position, and asked to reproduce it on a separate sheet immediately and after a 30-second delay, with 14 trials for each condition. The distance in cm between the drawn dot and the actual dot for immediate and delay conditions was measured and averaged for each condition; distance error was calculated as the 30-second delay minus immediate condition for each study day. Placebo- corrected performance was calculated as difference between the distance error on drug day and distance error on placebo day. The Positive and Negative Symptoms Scale (PANSS) was administered twice, at 8:30 A.M. and 12 P.M. Amphetamine drug levels (ng/ml; assayed by HPLC) were obtained at 12 P.M. and 1 P.M., and mean level is reported.
RESULTS
A repeated measures analysis of variance (ANOVA) was conducted with diagnosis (schizophrenia spectrum, nonspectrum) as the independent variable and amphetamine/placebo and delay condition (no delay, 30 s) as the within-subject factors.
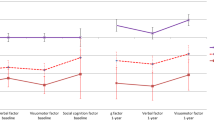
The following statistically significant effects were detected: (1) diagnosis (p < .02, where schizophrenia spectrum patients performed worse than nonspectrum patients); (2) drug (p < .03, where amphetamine improved performance as compared to placebo); (3) delay condition (p < .01, where the performance at the 30-s delay was worse than the no delay condition) (see Table 1). The most significant finding was a diagnosis by drug by delay condition interaction, in that the schizophrenia spectrum patients showed greater improvement after amphetamine as compared to placebo in the delay condition only (F[1,23] = 8.4, p < .01) as compared to the nonschizophrenia spectrum patient control group.
Stated differently, the two groups differed on the placebo corrected distance error (schizophrenia spectrum: −0.73 ± 0.9; nonschizophrenia spectrum: 0.15 ± .15; t = 2.83, n = 25, p < .02), where schizophrenia spectrum patients demonstrated a diminished distance error after amphetamine as compared to placebo; whereas, nonschizophrenia spectrum patients did not essentially differ between amphetamine and placebo. Placebo corrected distance error correlated inversely with distance error on placebo day (r = −0.76, n = 25, p < .001), indicating that the most impaired patients improved the most. The correlation was still statistically significant in the schizophrenia spectrum sample alone (r = −0.76, n = 12, p < .01); whereas, it did not reach significance in the nonschizophrenia spectrum sample (r = −0.40, n = 13, p = ns). Placebo corrected distance error was not significantly correlated with educational level (pooled within group correlation coefficient r = .32, df 22, p = ns), or age (r = −.14, df 22, p = ns).
Amphetamine improved negative symptoms in the whole sample, as measured by the PANSS (pre: 11.6 ± 4.6, post: 9.8 ± 2.9; paired t-test: t = 2.3, df 22, p < .03). Although not statistically significant in the SPD sample alone, the finding in the whole sample seemed to be largely attributable to the schizophrenia spectrum personality disorder patients, who improved more (post minus pre: −2.1 ± 4.2) than the nonschizophrenia spectrum patients (post minus pre: −1.5 ± 3.1, p = ns). Positive symptoms remained unchanged in the whole sample (pre: 9.6 ± 3.2, post: 9.8 ± 3.1; paired t-test: t = 0.9, df 17, p = ns) and in each group (schizophrenia spectrum: pre: 11.2 ± 4.0; post: 11.2 ± 3.5; t = 0.8, p = ns; nonspectrum pre: 8.5 ± 2.3; post: 8.6 ± 2.5; t = 0.5, p = ns); and no patient showed worsening of psychotic-like symptoms. The mean amphetamine levels did not differ between the two groups (schizophrenia spectrum: 67.8 ± 14.8; nonspectrum: 60.0 ± 15.0; t = 1.0, p = ns).
DISCUSSION
Abnormal visuospatial working memory has been reported in the schizophrenia spectrum; in an overlapping sample at our center, performance of 15 SPD patients on the Dot test was significantly impaired (Lees Roitman et al. 1996). In this preliminary study, we have shown a significant improvement in visuospatial working memory following administration of amphetamine in patients with schizophrenia spectrum personality disorder. This improvement might be secondary to an amphetamine-induced increase in dopamine, possibly acting at D1 receptors in the frontal cortex, because frontal hypodopaminergia has been linked with impaired cognitive functioning in the schizophrenia spectrum, and amphetamine may act primarily at the D1 receptor (Ferger et al. 1994). Patients who were more impaired at baseline showed greater amphetamine-induced improvement, particularly within the schizophrenia spectrum group. Although this improvement may represent, in part, a regression to the mean, this improvement may also be attributable to the differential amphetamine effect between schizophrenia spectrum patients who had greatest baseline impairment and the comparison group. The significant correlation in the schizophrenia spectrum, but not in the nonspectrum, patients is consistent with this possibility. These spectrum patients might have a greater cortical dopaminergic deficit to begin with, and, thus, may benefit more from amphetamine. It would be of interest to explore whether more specific D1 agonists would improve cognition further in these patients.
Negative symptoms improved after amphetamine. Larger samples are required to determine whether schizophrenia spectrum personality disorder patients improve more with regard to negative traits after amphetamine than nonspectrum patients, as suggested by this data. Psychotic-like symptoms in the schizophrenia spectrum group did not worsen after administration of amphetamine in contrast to schizophrenic patients who experience a transient worsening of their symptoms (see reviews by Angrist et al. 1980; van Kammen et al. 1982). We hypothesize this may be because schizophrenia spectrum patients release less dopamine after amphetamine as compared to schizophrenic patients whose increased dopamine release correlates with the worsening of their psychotic symptoms (Laruelle et al. 1996). We hypothesize that schizophrenia spectrum patients’ dopamine release after amphetamine is similar to normal subjects’ release after amphetamine consistent with our pilot data measuring dopamine release after amphetamine via SPECT utilizing an IBZM displacement paradigm (Koenigsberg et al. 1999).
These results invite replication; larger samples are required to test the effects of other clinical and demographic variables adequately. Because our comparison group did not have substantial cognitive impairment, it cannot be determined whether amphetamine improves cognitive impairment regardless of diagnosis: the close association between cognitive impairment and SPD traits suggests these two variables may represent the same underlying pathology and, therefore, may not be easily dissociable.
These findings may have important treatment implications, because patients with schizophrenia spectrum disorders represent a unique population in which to test the effects of such interventions that might improve deficit symptoms and cognitive impairment. More specific agents need to be piloted in more sustained treatment trials in the spectrum. The results of these studies conducted in these spectrum patients, who seem to have cognitive deficits that are somewhat less severe and more readily reversible than those of schizophrenic patients, may provide clues to new effective interventions in patients with chronic schizophrenia.
References
Angrist B, Rotrosen J, Gershon S . (1980): Responses to apomorphine, amphetamine, and neuroleptics in schizophrenic subjects. Psychopharmacology 67: 31–38
Battaglia M, Bernardeschi L, Franchini L, Bellodi L, Smeraldi E . (1995): A family study of schizotypal disorder. Schiz Bull 21: 33–46
Cornblatt BA, Lezenweger MF, Erlenmeyer-Kimling L . (1989): The continuous performance task, identical pairs version (CPT-IP). II. Contrasting attentional profiles in schizophrenic and depressed patients. Psych Res 26: 65–85
Daniel D, Weinberger D, Jones D, Zigun J, Coppola R, Handel S . (1991): The effect of amphetamine on regional cerebral blood flow during cognitive activation in schizophrenia. J Neurosci 11: 1907–1917
Ferger B, Kropf W, Kushinsky K . (1994): Studies on electroencephalogram in rats suggest that moderate doses of cocaine or d-amphetamine activate D1 rather than D2 receptors. Psychopharmacology-Berl 114: 297–308
Gold J, Carpenter C, Randolph C, Goldberg T, Weinberger D . (1997): Auditory working memory and Wisconsin Card Sorting Test performance in schizophrenia. Arch Gen Psychiat 54: 159–165
Goldberg T, Bigelow L, Weinberger D, Daniel D, Kleinman J . (1991): Cognitive and behavioral effects of co-administration of dextroamphetamine and haloperidol in schizophrenia. Am J Psychiat 148: 78–84
Green MF, Marshall BD, Wirshing WC, Ames D, Marder SR, McGurk S, Kern RS, Mintz J . (1997): Does risperidone improve verbal working memory in treatment-resistant schizophrenia? Am J Psychiat 154: 799–804
Green MF . (1996): What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiat 153: 321–330
Kahn RS, Harvey PD, Davidson M, Keefe RSE, Apter S, Neale JM, Mohs RC, Davis KL . (1994): Neuropsychological correlates of central monoamine function in chronic schizophrenia: Relationship between CSF metabolites and cognitive function. Schizophr Res 11: 217–224
Keefe RSE, Silverman J, Mohs R, Siever L, Harvey P, Friedman L, Roitman S, Du Pre R, Smith C, Schmeidler J, Davis K . (1997): Eye tracking, attention and schizotypal symptoms in nonpsychotic relatives of patients with schizophrenia. Arch Gen Psychiat 54: 169–176
Keefe RSE, Roitman SE, Harvey PD, Blum CS, DuPre RL, Prieto DP, Davidson M, Davis KL . (1995): A pen-and-paper human analog of a monkey prefrontal cortex activation task: Spatial working memory in patients with schizophrenia. Schizophr Res 17: 25–33
Kendler KS, Gardner CO . (1997): The risk of psychiatric disorders in relatives of schizophrenic and control probands: A comparison of three independent studies. Psychol Med 27: 411–419
Kendler KS, Diehl SR . (1993): The genetics of schizophrenia. A current genetic epidimiologic perspective. Schiz Bull 19: 261–285
Koenigsberg H, Mitropoulou V, Abi-Dargham A, Nunn M, Laruelle M, Siever L . (1999): Subcortical dopamine activity in schizotypal personality disorder. Presented as an NR abstract at the 152nd annual APA Meeting, Washington DC.
Laruelle M, Abi-Dargham A, Van Dyck C, Gil R, D'Souza C, Erdos J, McCance E, Rosenblatt W, Fingado C, Zogbi SS, Baldwin RM, Seibyl JP, Krystal JH, Charney DS, Innis RB . (1996): Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic patients. Proc Natl Acad Sci USA 93: 9235–9240
Lees Roitman SE, Keefe RSE, DuPre RL, Siever L . (1996): Visuospatial working memory in schizotypal personality disorder. Abstract #266, Society of Biological Psychiatry Annual Meeting, 1996.
Park S, Holzman PS . (1992): Schizophrenics show spatial working memory deficits. Arch Gen Psych 49: 975–982
Park S, McTigue K . (1997): Working memory and the syndromes of schizotypal personality. Schizophr Res 26: 213–220
Siegel BV, Trestman RL, O'Flaithbheartaigh S, Mitropoulou V, Amin F, Kirrane R, Silverman JM, Schmeidler J, Keefe RSE, Siever L . (1996): D-amphetamine challenge effects on Wisconsin Card Sort Test. Performance in schizotypal personality disorder. Schizophr Res 20: 29–32
Siever L, Kalus OF, Keefe RSE . (1993): The boundaries of schizophrenia. Psychiat Clin N Am 16: 217–244
Trestman RL, Keefe RSE, Mitropoulou V, Harvey PD, deVegvar ML, Losonczy MF, Lees-Roitman S, Davidson M, Aronson A, Silverman J, Siever LJ . (1995): Cognitive function and biological correlates of cognitive performance in schizotypal personality disorder. Psychiat Res 59: 127–136
van Kammen DP, Bunney WE, Docherty JP, Marder S, Ebert MH, Rosenblatt JE, Rayner JN . (1982): d-Amphetamine-induced heterogeneous changes in psychotic behavior in schizophrenia. Am J Psychiat 139: 991–997
Weinberger DR, Lipska BK . (1995): Cortical maldevelopment, antipsychotic drugs, and schizophrenia: A search for common ground. Schizophr Res 16: 87–110
Williams GV, Goldman-Rakic PS . (1995): Modulation of memory fields by dopamine D1 receptors in prefrontal cortex. Nature 376: 572–575
Acknowledgements
This work was supported in part by a VA Postdoctoral Research Training Award to Dr. Kirrane, NIMH Grant RO1-MH 56140, and VA Merit award to Dr. Siever, and NIH SMO1 RR00071 to the Mount Sinai Hospital General Clinical Research Center.
Author information
Authors and Affiliations
Additional information
This work was presented at the American Psychiatric Association Annual Meeting, San Diego, CA, May 17–22, 1997
Rights and permissions
About this article
Cite this article
Kirrane, R., Mitropoulou, V., Nunn, M. et al. Effects of Amphetamine on Visuospatial Working Memory Performance in Schizophrenia Spectrum Personality Disorder. Neuropsychopharmacol 22, 14–18 (2000). https://doi.org/10.1016/S0893-133X(99)00075-5
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00075-5
Keywords
This article is cited by
-
Effects of the D1 Dopamine Receptor Agonist Dihydrexidine (DAR-0100A) on Working Memory in Schizotypal Personality Disorder
Neuropsychopharmacology (2015)
-
Remediation and Cognitive Enhancers in Schizotypal Personality Disorder
Current Treatment Options in Psychiatry (2014)
-
SSR504734 enhances basal expression of prepulse inhibition but exacerbates the disruption of prepulse inhibition by apomorphine
Psychopharmacology (2013)
-
The amphetamine sensitization model of schizophrenia: relevance beyond psychotic symptoms?
Psychopharmacology (2009)
-
Persönlichkeitsstörungen – Diagnostische Konzepte – Neurobiologie-Pharmakotherapie
Psychiatrie und Psychotherapie (2008)