Abstract
To investigate the effect on the sleep EEG, a 1-mg oral dose of SR 46349B, a novel 5-HT2 antagonist, was administered three hours before bedtime. The drug enhanced slow wave sleep (SWS) and reduced stage 2 without affecting subjective sleep quality. In nonREM sleep (NREMS) EEG slow-wave activity (SWA; power within 0.75–4.5 Hz) was increased and spindle frequency activity (SFA; power within 12.25–15 Hz) was decreased. The relative NREMS power spectrum showed a bimodal pattern with the main peak at 1.5 Hz and a secondary peak at 6 Hz. A regional analysis based on bipolar derivations along the antero-posterior axis revealed significant ‘treatment’ × ‘derivation’ interactions within the 9–16 Hz range. In enhancing SWA and attenuating SFA, the 5-HT2 receptor antagonist mimicked the effect of sleep deprivation, whereas the pattern of the NREMS spectrum differed.
Similar content being viewed by others
Main
The pivotal role of serotonin (5-hydroxytryptamine, 5-HT) in sleep regulation has been the mainstay of the monoamine theory of sleep (Jouvet 1972). Although the views about the functions of this neurotransmitter have evolved, there is little doubt about its involvement in sleep mechanisms (McCormick 1992). Serotonergic neurons of the nucleus raphe dorsalis are most active during wakefulness and have been proposed to participate in the build-up of sleep propensity (Adrien 1995). Animal studies revealed that these neurons decrease firing upon transition from wakefulness to nonREM sleep (NREMS), and become quiescent during REM sleep (REMS). Thus, deactivation of the serotonergic system may facilitate the production of NREMS and REMS (Adrien 1995). One of the complexities in accounting for the actions of 5-HT is the large number of different receptors and receptor subtypes. 5-HT receptors are classified into four distinct classes, comprising seven fully characterized functional receptor subtypes and several recombinant receptors (Hoyer and Martin 1996). While the involvement of three main classes (i.e., 5-HT1, 5-HT2, and 5-HT3 receptors) in the regulation of sleep and wakefulness has been studied, it is the postsynaptic 5-HT1A receptor that seems to mediate the inhibition of REMS and the promotion of wakefulness, whereas activation of the 5-HT2 receptor may exert a tonic inhibition of slow wave sleep (SWS) (see Adrien 1995 for review). In relation to sleep homeostasis, the latter is of particular interest because 5-HT2 antagonists were shown to increase the amount of SWS and to enhance EEG slow-wave activity (SWA; power within 0.75–4.5 Hz) in humans and animals (Idzikowski et al. 1986; Borbély et al. 1988; Dijk et al. 1989). The 5-HT2 receptor family is subdivided into three specific subtypes (i.e., 5-HT2A, 5-HT2B, and 5-HT2C receptors) (Humphrey et al. 1993). Whereas it is not clear whether 5-HT2B binding sites are present in the human brain, the 5-HT2A subtype may be identical with the classical 5-HT2 receptor. However, 5-HT2C receptors have been proposed to play a more important role in the regulation of SWS than 5-HT2A receptors (Sharpley et al. 1994).
SWA represents a physiological marker of the homeostatic facet of sleep regulation (Borbély and Tononi 1998). It shows typically a declining trend across successive NREMS episodes and has been considered to be an indicator of NREMS intensity. Sleep loss enhances SWA and daytime sleep attenuates it (Borbély et al. 1981; Aeschbach et al. 1996; Werth et al. 1996). During the transition from waking to sleep, the activity of the ascending monoaminergic reticular pathways is progressively reduced which leads to a hyperpolarization of thalamocortical neurons (McCormick and Bal 1997). A moderate hyperpolarization results in fluctuations of the membrane potential in the frequency range of sleep spindles, whereas a strong hyperpolarization gives rise to fluctuations in the slow-wave range (Steriade et al. 1993, 1994). These changes at the cellular level are mirrored by the sleep EEG, which exhibits sleep spindles in stage 2 of NREMS and slow waves during deep NREMS (i.e., stages 3 and 4). Application of 5-HT to thalamocortical neurons may block rhythmic burst firing and suppress slow synchronized oscillations (McCormick 1992). Animal studies suggest that these effects are mediated via 5-HT2 receptors (McCormick and Wang 1991; Bobker 1994).
It was shown repeatedly that the physiological enhancement of “sleep pressure” by sleep deprivation enhances power density in the entire delta and theta frequency range (∼0.5-10 Hz), whereas power in the frequency band of sleep spindles (12-15.0 Hz) is reduced (Borbély et al. 1981; Dijk et al. 1990, 1993; Aeschbach et al. 1996). Both SWA and spindle frequency activity (SFA, power within 12.25-15.0 Hz) were shown to rise more rapidly than in baseline in the beginning of recovery sleep (Dijk et al. 1990; Aeschbach et al. 1996). Recent studies demonstrated that these EEG changes reflecting sleep regulatory mechanisms show distinct regional differences. Thus in the first two sleep cycles, SWA recorded from frontal derivations was more prominent than SWA from more posterior derivations, a difference that vanished in the later sleep cycles (Werth et al. 1997). The possibility that restorative processes of NREMS are most intense over the frontal cortex is also supported by a sleep deprivation experiment (Werth et al. 1998). These observations prompted us to perform a topographical analysis in the present study and to see whether interference with the serotonergic system has specific regional effects.
The development of specific 5-HT2 receptor antagonists provided new tools to investigate the role of the serotonergic system in sleep regulation. SR 46349B is a novel, potent and selective 5-HT2A receptor antagonist in rodents (Rinaldi-Carmona et al. 1992). It was administered to healthy young subjects to investigate its effects on the sleep EEG and to compare them with the changes that had been previously observed after sleep deprivation. The main question addressed in the present study was whether this 5-HT2 antagonist mimics the effects of physiological sleep intensification. In view of the close association between body temperature and sleep regulation, and the involvement of central 5-HT2 receptors in thermoregulation (Schwartz et al. 1995), rectal temperature was measured during all sleep episodes.
METHODS
Subjects and study protocol
Male volunteers from the student populations of the University of Zürich and the Swiss Federal Institute of Technology were recruited for participation in this study. After a telephone screening, they were invited to the sleep laboratory to complete a questionnaire on subjective sleep quality, current sleep-wake habits, medical history, and the use of caffeine and ethanol. They all reported being good sleepers, being in good health and were not taking any medication or consuming any illicit drugs. They underwent a physical examination including routine screening laboratory tests of blood and urine. They were asked to keep a sleep-, caffeine-, and ethanol-log during one week. Subsequently, the subjects were screened by polysomnography in the sleep laboratory to exclude sleep disturbances such as sleep apnea and nocturnal myoclonus. Written informed consent was obtained prior to the screening night. Subjects with sleep apnea, a nocturnal myoclonus-index of ten or more per hour of sleep, and a sleep-efficiency of less than 70% were excluded. Ten healthy, right-handed men with a mean age of 22.0 ± 0.3 (SEM) years (range: 20–25 years) and a mean body-mass index (BMI) of 21.5 ± 1.2 (SEM) kg/m2 (range: 19.7–24.1 kg/m2) were selected and paid for participation. Their diaries and questionnaires revealed regular time in bed between approximately 2300 and 0700 hrs and no subjective sleep disturbances. All subjects were nonsmokers and reported a consumption of less than eight alcoholic drinks per week, and less than three caffeine-containing beverages (coffee, tea, cola drinks) per day. At least three days prior to each sleep recording and during the experiment, the subjects were asked to abstain from ethanol and caffeine. During the pre-study week, they also were instructed to keep a regular sleep-wake cycle with sleep scheduled from 2300 to 0700 hrs. Compliance with these instructions was verified on the basis of records from activity monitors worn on the wrist of the non-dominant arm as well as by determination of the breath-ethanol concentration and the level of caffeine in saliva upon arrival in the sleep laboratory (at approximately 1930 hrs). Breath-ethanol concentrations were measured with a Lion Alcometer S-D2 (Lion Laboratories plc., Barry, Wales, UK). Saliva samples were stored at −20°C and later assayed for caffeine with an EMIT®-Caffeine Test (Syva Company, Palo Alto, CA). The caffeine level in the subjects’ saliva was invariably below the limit of detection (1.0 μmol/l) and no ethanol in their breath was detected.
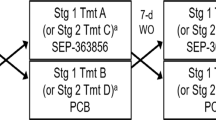
The study protocol was approved by the local ethical committee for research on human subjects and consisted of two sessions of two consecutive nights. On each session, an adaptation night was followed by an experimental night. Subjects slept in the completely dark and sound attenuated bedrooms of the sleep laboratory from 2300 to 0700 hrs. At 2000 hrs prior to the scheduled experimental nights they received a tablet which either contained 1 mg SR46349B or placebo (manufacturer: SANOFI Recherche, Montpellier Cédex 4, France). Thus, a single oral dose of SR 46349B was administered to each subject according to a randomized, placebo-controlled, double-blind, cross-over design. A 1-mg dose was chosen on the basis of previous, unpublished dose-response studies.
Fifteen minutes after awakening, subjective sleep quality (estimated sleep latency, perceived number of awakenings, estimated wake duration after sleep onset, sound vs. fragmented sleep, and superficial vs. deep sleep) and self-rated state (recuperated vs. tired, bad mood vs. good mood, lack of energy vs. full of energy, tense vs. relaxed, and unable to concentrate vs. able to concentrate) were assessed by a questionnaire and 100-mm on some live visual analogue scales.
Polygraphic recordings, heart rate and core body temperature
The electroencephalogram (EEG), electrooculogram (EOG), submental electromyogram (EMG), electrocardiogram (ECG), and rectal temperature were recorded by a polygraphic amplifier (PSA24, Braintronics Inc., Almere, The Netherlands), digitized, and transmitted via fiber-optic cables to a personal computer. EEG electrodes were placed at the locations F3, F4, C4, P3, P4, O1, O2, Cz, and A2, and referenced against C3. EEG, EOG, and EMG signals were conditioned by the following analogue filters: a high-pass filter (−3 dB at 0.16 Hz), a low-pass filter (−3 dB at 102 Hz, < −40 dB at 256 Hz), and a notch filter (50 Hz). Data were sampled with a frequency of 512 Hz, digitally filtered (EEG: low-pass FIR filter, −3 dB at 49 Hz; EMG: band-pass FIR filter, −3 dB at 15.6 and 54 Hz), and stored on hard-disk with a resolution of 128 Hz. Subsequently, power spectra for consecutive 4-s epochs, weighted by application of a 10% cosine window, were computed by a Fast-Fourier transform routine, resulting in a frequency resolution of 0.25 Hz. Values above 25 Hz were omitted. Sleep stages were visually scored from the records of the C3A2 derivation for consecutive 20-s epochs according to the criteria of Rechtschaffen and Kales (1968). Power spectra of five consecutive 4-s epochs were averaged and matched with the sleep scores. Four-s epochs with artifacts were identified and eliminated. Consecutive NREM-REMS cycles were defined according to modified criteria of Feinberg and Floyd (1979). NREMS episodes starting with stage 2 and containing at least 15 minutes of the stages 2, 3 and 4 were succeeded by REMS episodes of at least 5 minutes duration. For the completion of the first cycle no minimal criterion for the REMS duration was applied. With the exception of two sleep episodes, at least four NREM-REMS cycles were completed in all experimental nights.
Regional differences were investigated by comparing the spectra of the bipolar derivations along the antero-posterior axis. Due to artifacts, the data of two subjects had to be excluded from the topographical analyses.
One value of heart rate (beats per minute, as calculated from the mean time interval between consecutive R-waves) and one value of core body temperature were stored every 20 sec. Due to technical problems the temperature data of two subjects were lost.
Statistics
For statistical analyses the SAS General Linear Model procedure (SAS Institute Inc., Cary, NC) with Greenhouse-Geisser correction was used (if a factor had more than two levels). Visually scored sleep variables, EEG power spectra in NREMS and REMS, the time course and evolution of SWA and in the first four NREMS episodes, and regional differences of EEG spectra were analyzed. Significant effects of the treatment and differences between bipolar derivations were assessed using one-, two-, and three-way analyses of variance for repeated measures (rANOVA). Statistical models included terms for the between factor ‘sequence’ and multiple within factors as described in the Results section. The significance level was set at p<0.05. To approximate the normal distribution, values of sleep latency, REMS latency, absolute power densities and ratios of power densities between derivations were log-transformed prior to statistical tests.
RESULTS
Sleep variables derived from visual scoring and subjective sleep quality
The major change induced by the drug consisted of the large increase of SWS as well as its constituent stages 3 and 4 (Table 1 and Table 2). While the enhancement of SWS reached the highest level in the second NREMS episode, it was increased in each of the first three episodes. In contrast, stage 2 was reduced in the second NREMS episode. Waking after sleep onset and the combined arousal variable (wakefulness + movement time + stage 1) did not differ significantly from the placebo level, but movement time was reduced. There was no significant difference in the all-night duration of REMS. However, when expressed as a percentage of total sleep time, REMS was decreased (Table 2). The duration of the second and the third NREMS episodes were prolonged (Table 1).
No significant differences between the placebo and treatment nights were observed for sleep episode, total sleep time, sleep efficiency, latency to stage 1, latency to stage 2, and REMS latency (Table 2).
State variables in the morning, and subjective sleep quality did not differ significantly between the treatments.
EEG power spectra
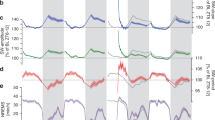
Figure 1 is a composite representation of the sleep stage profiles and EEG SWA from a subject after placebo (upper panel) and drug treatment (lower panel). Note the increase in stage 3 and 4 sleep and the concomitant enhancement of SWA in the drug night. The comparison of corresponding NREMS episodes reveals enhanced SWA in the second and following episodes. In the mean all-night power spectra shown in Figure 2, the values for the drug night are expressed as percentage of the placebo night. Power density values were averaged into 0.5-Hz (0.25-5.0 Hz) and 1.0-Hz (5.25-25.0 Hz) bins. The spectra were calculated separately for NREMS (stages 2, 3, and 4), stage 2, SWS, and REMS. The NREMS spectrum showed a bimodal pattern in the low-frequency range. The major peak was situated at 1.5 Hz and a secondary peak at 6 Hz. Within the 11.25–14.0 Hz and 15.25–19.0 Hz range, the drug values were below the placebo level, the minimum corresponding to the 12.25–14.0 Hz spindle frequency range. The changes in the spectra were most pronounced in the second and third NREMS episode (data not shown). The spectrum in stage 2 was very similar to that of NREMS with the exception that the enhancement was restricted to the low-frequency range (⩽ 3 Hz). In contrast, the SWS spectrum did not exhibit an increase of SWA. Power in the 2.75–3.0 Hz bin was even below the placebo level. The increased SWA in stage 2 and the absence of an increase in SWS is also evident in the records shown in Figure 1. In REMS, power density was reduced in two bins of the delta band (2.75–3.25 Hz).
Sleep stages and EEG slow-wave activity (SWA, power density within 0.75–4.5 Hz; C3A2-derivation) of a subject after intake of placebo (upper panel) and SR 46349B (lower panel). 1, 2, 3, and 4: NREMS stages 1–4; W, wakefulness; MT, movement time; R, REMS. The curves of SWA were smoothed by a three-point moving average.
EEG power density (C3A2-derivation) in nonREM sleep (NREMS, stages 2, 3, and 4), stage 2 (S2), slow wave sleep (SWS, stages 3 and 4) and REM sleep (REMS) after SR 46349B administration. For each frequency bin (•, ± 1 SEM, n = 10), means were expressed as a percentage of the corresponding value after placebo (horizontal dashed lines at 100%). Values are plotted at the upper limit of the bins. Triangles at the bottom of the panels indicate frequency bins which differed significantly from placebo (p < .05, rANOVA with within factor ‘treatment’); their orientation indicates the direction of deviation from placebo.
Dynamics of slow-wave activity (SWA) and spindle frequency activity (SFA)
In both the placebo and drug condition SWA was high in NREMS and low in REMS, and a declining trend was present over consecutive NREMS episodes. In Figure 3 (upper panel) the enhancement of SWA by SR 46349B is evident. This was confirmed by a rANOVA with the within factors ‘treatment’ (placebo, SR 46349B) and ‘time-bin’ (1–20) which revealed a significant effect of the factor ‘treatment’ for NREMS episodes 2 and 3 (F1,8 = 263.5, p < .0001 and F1,8 = 24.1, p < .001, respectively). A statistical trend for ‘treatment’ was present for episodes 1 and 4 (F1,7 = 4.8, p < .07 and F1,7 = 3.8, p < .1).
Time course of EEG slow-wave activity (SWA, 0.75–4.5 Hz range; C3A2-derivation) and spindle frequency activity (SFA, 12.25–15.0 Hz range; C3A2-derivation) plotted after treatment with placebo (left) and SR 46349B (right). For each subject, individual NREMS episodes were subdivided into 20 equal time-bins, and REMS episodes as well as the interval between lights-out and sleep onset were subdivided into four equal time-bins. Data were averaged across subjects (n = 10) and plotted against the mean timing of NREMS and REMS. Vertical bars represent ± 1 SEM and dashed vertical lines delimit REMS episodes. Triangles indicate NREMS episodes with a significant ‘treatment’ effect (see text for statistics); orientation of the triangles indicates the direction of deviation from placebo.
The typical pattern of SFA with low values in REMS episodes, and a higher level, U-shaped pattern in NREMS, was present in both conditions. However, SFA was significantly lower in the drug night in all four NREMS episodes (Figure 3, lower panel; rANOVA, within factor ‘treatment’: NREM-1: F1,7 = 7.4, p < .03; NREM-2: F1,8 = 17.8, p < .003; NREM-3: F1,8 = 15.2, p < .005; and NREM-4: F1,7 = 11.3, p < .02). The global pattern during the first four NREMS episodes was similar in both conditions (rANOVA on mean episodic SFA values: ‘treatment’ × ‘episode’: F3,24 = 2.1, n.s.).
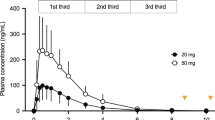
Evolution of SWA and SFA in the first four NREMS episodes
The build-up of SWA and SFA in the first part of NREMS episodes, and the decline in the final part of the episodes, are illustrated in Figure 4. Values for consecutive 2-min epochs are plotted for the first and last 30 min of each episode. For each 30-min interval a significant effect of ‘2-min epoch’ was revealed by rANOVA for SWA and SFA (data not shown). SWA values of several 2-min bins of episodes 2, 3, and 4 were higher after drug treatment than after placebo. To analyze the rise rate of SWA, the median of the differences of adjacent 2-min values was computed for the interval from −2 min to +20 min for each NREMS episode. A significantly higher rise rate was observed for the drug condition in the second (6.4 vs. 19.8%/2 min) and fourth episodes (2.0 vs. 3.9%/2 min; rANOVAs with within factor ‘treatment: F1,8 = 10.7, p < .02 and F1,8 = 25.7, p < .01, respectively), and a similar tendency prevailed in the third episode (5.1 vs. 8.5%/2 min, F1,8 = 3.4, p = .1).
Evolution of slow-wave activity (SWA, 0.75–4.5 Hz range, C3A2-derivation; upper panels) and spindle frequency activity (SFA, 12.25–15.0 Hz range, C3A2-derivation; lower panels) during the first 30 minutes and last 30 minutes of the first four NREMS episodes, after administration of placebo (open circles) and SR 46349B (filled circles). The data are expressed as a percentage of the mean power density in NREMS of the placebo night (indicated by horizontal dashed lines at 100%). Mean values (n = 10) are plotted for consecutive 2-min epochs; vertical lines represent 1 SEM. Dashed vertical lines indicate the beginning and the end of the NREMS episodes. Repeated measures ANOVA with the within factors ‘treatment’ and ‘2-min epoch’ revealed a significant effect of ‘treatment’ in the initial and final 30 minutes of most NREMS episodes. SWA: NREM-1, rise: F1,7 = 0.6, n.s.; fall: F1,8 = 3.4, n.s.; NREM-2, rise: F1,8 = 19.7, p < .003; fall: F1,8 = 16.2, p < .004; NREM-3, rise: F1,8 = 6.5, p < .04; fall: F1,8 = 10.9, p < .02; NREM-4, rise: F1,7 = 8.7, p < .03; fall: F1,7 = 2.4, n.s.; SFA: NREM-1, rise: F1,7 = 8.5, p < .03; fall: F1,8 = 10.7, p < .02; NREM-2, rise: F1,8 = 8.7, p < .02; fall: F1,8 = 33.5, p < .0005; NREM-3, rise: F1,8 = 12.5, p < .008; fall: F1,8 = 17.1, p < .004; NREM-4, rise: F1,7 = 9.2, p < .02; fall: F1,7 = 20.3, p < .003. Triangles at the bottom of the panels indicate epochs with significant treatment effects; open triangels: p < .05, filled triangles: p < .01 (rANOVA with within factor ‘treatment’); orientations point to the direction of deviation from placebo.
SFA showed a rapid initial rise reaching the peak value after 5–10 min after the onset of NREMS, and decreased thereafter. In the last 30 min of NREMS, a transient increase preceded occasionally the sharp decline in the first three NREMS episodes. This typical time course of SFA was preserved after drug administration (rANOVA: ‘treatment’ × ‘2-min epoch’, p ⩾ .09 in the initial and final 30 min of the first four NREMS episodes). Nevertheless, the SFA values were below the placebo level in several 2-min epochs as shown by the statistics in Figure 4.
Regional differences of the EEG spectra
The six panels on the right side of Figure 5 show the relative NREMS spectra of the drug night for three bipolar derivations along the antero-posterior axis recorded from the left and right hemisphere. Absolute spectra averaged over both hemispheres are shown in the left column of the figure. The pattern of changes seen for the referential derivation (Figure 2) was present also for the bipolar derivations. It consisted of a main peak in the low delta band, a secondary peak around 6 Hz and a trough at 13 Hz. Significant deviations from placebo are indicated by the F-values at the bottom of the panels (rANOVA with within factor ‘treatment’).
All-night EEG power spectra of bipolar derivations along the antero-posterior axis. Power density values for each frequency bin are expressed as μV2/0.25 Hz (left; placebo: thin line, SR 46349B: thick line; values averaged over left and right hemispheres), or as a percentage of the corresponding value after placebo (right; vertical lines represent ± 1 SEM, n = 8). Mean values are plotted in the middle of the bins. Vertical bars above the abscissae represent significant log. F-values of a rANOVA on log-transformed absolute power density values with the within factor ‘treatment’ (df = 1,6).
The regional differences of the bipolar derivations along the antero-posterior axis are indicated in Figure 6 where the mean values of the middle (CP) and posterior derivations (PO) are expressed as a percentage of the anterior derivation (FC). The F-values of a rANOVA with the within factors ‘A-P derivation’ (FC, CP, PO), ‘L-R derivation’ (left hemisphere, right hemisphere) and ‘treatment’ confirm that significant regional differences prevail in the 1.125–2.0 Hz and 4.375–14.5 Hz range (Figure 6, middle panel). Although the regional differences were similar for the placebo and drug condition, a significant interaction ‘treatment’ × ‘A-P derivation’ was present in the 9.125–12.0 Hz range as well as in most bins within the 13.375–16.0 Hz band. The latter was due to the anterior shift of power in these frequency bins. The interaction ‘treatment’ × ‘L-R derivation’ (hemispheres) and the 3-way interaction ‘treatment’ × ‘A-P derivation’ × ‘L-R derivation’ were not significant.
Regional differences of all-night power spectra in NREMS (stages 2, 3, and 4) along the antero-posterior axis after placebo (continuous lines) and SR 46349B (interrupted lines). Top panel: For each frequency bin, power density values in the central (thick lines) and parietal (thin lines) derivations are expressed as a percentage of the corresponding values in the frontal derivation (100%). Mean values over the left and right hemispheres are plotted in the middle of the bins. Bottom panels: Vertical bars represent significant log. F-values of a rANOVA on log-transformed absolute power density values with the within factors ‘treatment’ (df = 1,6), ‘A-P derivation’ (FC, CP, PO; df = 2,12), and ‘L-R derivation’ (left hemisphere, right hemisphere; df = 1,6).
Core body temperature
Rectal temperature declined in the first 6 hours of sleep and showed an increasing trend in the last 2 hours (Figure 7). However, temperature was lower in the drug night than in the placebo night. The difference of the mean values in hour 5–6 was 0.24°C. A rANOVA with the within factors ‘treatment’ and ‘hour’ (1–8) revealed significant effects of ‘treatment’ (F1,6 = 6.3, p < .05) and ‘hour’ (F7,42 = 10.1, p<0.004; ‘treatment’ × ‘hour’: F7,42 = 0.7, n.s.).
Time course of rectal temperature after administration of placebo (open circles) and SR 46349B (filled circles). Mean values (n = 8) are plotted in the middle of consecutive 1-hour intervals; vertical lines represent ± 1 SEM. A rANOVA with the within factors ‘treatment’ and ‘hour’ revealed a significant ‘treatment’ effect (F1,6 = 6.03, p < .05).
DISCUSSION
The present study shows that a single oral dose of 1 mg SR 46349B, a potent and selective 5-HT2 receptor antagonist, affects the sleep stages and EEG power spectra of young healthy men. The principal effect consisted of a massive increase of SWS and SWA. Similar changes had been reported for the less selective 5-HT2 antagonists ritanserin and seganserin (Idzikowski et al. 1986;; Declerck et al. 1987; Borbély et al. 1988; Dijk et al. 1989). In previous studies, also a 10-mg dose of the 5-HT1A agonist ipsapirone enhanced SWA in the first two hours of NREMS (Seifritz et al. 1996), yet did not increase SWS (Gillin et al. 1994, 1996). The effects of ipsapirone on EEG power spectra in NREMS were remarkably similar to those induced by seganserin (Seifritz et al. 1996). These results and single unit recordings (Ashby et al. 1994) support the notion that inhibitory 5-HT1A receptors and excitatory 5-HT2 receptors mediate opposite changes. Unlike ritanserin (Borbély et al. 1988), seganserin (Dijk et al. 1989), and ipsapirone (Tissier et al. 1993; Gillin et al. 1994, 1996; Driver et al. 1995), SR 46349B did not influence the amount and the latency to REMS.
Hypothermia is also a well-known effect of the 5-HT1A agonist ipsapirone (Lesch et al. 1990). The slight hypothermia induced by SR 46349B demonstrates that the 5-HT1A and 5-HT2 receptors mediate opposite changes also at the level of thermoregulation.
There were striking similarities between the effects of SR 46349B and those induced by sleep deprivation (SD). Specifically, after both interventions: 1) the maximum increase of delta frequency activity was at 1.5 Hz (SD: Borbély et al. 1981, 1984; Dijk et al. 1990, 1993; Tobler and Borbély 1990; Aeschbach et al. 1996) (SR 46349B: Figure 2); 2) the build-up rate of SWA within NREMS episodes was increased (SD: Dijk et al. 1993; Aeschbach et al. 1996) (SR 46349B: Figure 4); and 3) SFA was reduced (SD: Borbély et al. 1981; Dijk et al. 1990, 1993) (SR 46349B: Figures 3 and 4). These findings suggest that 5-HT2A receptors are involved in the regulation of SWS. However, since the selective specificity of SR 46349B for 5-HT2A receptors has been so far demonstrated only in rodents (Rinaldi-Carmona et al. 1992), this aspect needs to be confirmed in humans.
There were also differences from the physiological effects. For one, unlike the typical unimodal increase of power in the delta and theta band following prolonged waking, the relative spectra of the present study had a bimodal appearance with a trough at 3.5–5 Hz. The trough appears to be a state independent feature, since it was present in both SWS and REMS (Figure 2). An association of this bimodal spectral pattern with the serotonergic system is supported by the observation that it is common to both 5-HT2 antagonists, i.e., seganserin in humans (Dijk et al. 1989) and ritanserin in rats (Borbély et al. 1988), and 5-HT1A agonists, i.e., ipsapirone (Seifritz et al. 1996). Another difference from the physiological changes was that low-frequency EEG activity was increased only in stage 2 (Figure 2), whereas prolonged waking had been shown to enhance SWA also in SWS and REMS (Borbély et al. 1981). Moreover, unlike after recovery from SD, the second and third NREMS episodes were prolonged. This suggests that antagonism at 5-HT2 receptors promotes the maintenance of synchronized EEG activity without enhancing maximal SWA beyond the usual level. The reduction of SFA at the expense of SWA seems to reflect the promotion of ‘deep NREMS’. The finding that NREMS does not appear to be intensified beyond the baseline level is in accordance with the observation that sleep was not perceived to be deeper than usual.
Different effects at the level of 5-HT receptors may be responsible for the discrepancies between physiological and pharmacological effects. In the present study, blockade of 5-HT2 binding sites may have prevented depolarization of thalamocortical neurons by their natural ligand (McCormick 1992Bobker 1994), and prolonged burst-pause firing and EEG synchronization. In contrast, due to continued 5-HT release during wakefulness (Portas et al. 1998), the serotonergic system may be desensitized after SD. Functional desensitization of endogenous 5-HT2 receptors associated with a partial down-regulation of receptor number has been demonstrated recently in vitro after treatment with 5-HT (Saucier et al. 1998).
The topographic analysis along the antero-posterior axis revealed robust derivation effects that correspond to those reported previously (Werth et al. 1997). The typical drug-induced changes were evident in all bipolar derivations. Nevertheless, the subtle yet significant interactions between treatment and derivation showed that the compound did affect the spatial distribution of EEG power. Interestingly, the significant interaction included not only the frequency range around 15 Hz in which drug-induced changes were manifest, but also frequencies at 10 Hz where no significant treatment effects were seen. These selective changes may be related to the regional distribution of cortical 5-HT2 receptors (Pazos et al. 1987) and demonstrate that the spatio-temporal analysis of the sleep EEG may disclose novel effects in pharmacological studies.
In conclusion, the antagonism of 5-HT2 receptors mimics the effects of sleep deprivation by enhancing SWA and attenuating SFA. However, unlike after prolonged waking, it is the duration of the NREMS fraction dominated by high SWA, which is increased, rather than NREMS intensity as reflected by the level of SWA in SWS (Figure 2). Moreover, perceived sleep intensity is not augmented. The 5-HT2 receptor antagonist induces a bimodal pattern in the NREMS spectrum which differs from the unimodal pattern seen after sleep deprivation. The bimodality is caused by a state independent reduction of power at 2–3 Hz. This effect has been reported for other 5-HT2 receptor antagonists, as well as for a 5-HT1A agonist. Hypothermia may represent a similar common feature of 5-HT2 antagonists and 5-HT1A agonists. The present results show that altering the balance between 5-HT2 and 5-HT1A receptor activity may be necessary, but is not sufficient, for inducing the changes in the EEG spectrum which are typically seen after sleep deprivation.Borbély Tobler Hanagasioglu 1984
References
Adrien J . (1995): The serotoninergic system and sleep-wakefulness regulation. In Kales A (ed), The Pharmacology of Sleep. New York, Springer, pp 91–116
Aeschbach D, Cajochen C, Landolt HP, Borbély AA . (1996): Homeostatic sleep regulation in habitual short and long sleepers. Am J Physiol 270: R41–R53
Ashby CR Jr, Edwards E, Wang RY . (1994): Electrophysiological evidence for a functional interaction between 5-HT1A and 5-HT2A receptors in the rat medial prefrontal cortex: An iontophoretic study. Synapse 17: 173–181
Bobker DH . (1994): A slow excitatory postsynaptic potential mediated by 5-HT2 receptors in nucleus prepositus hypoglossi. J Neurosci 14: 2428–2434
Borbély AA, Baumann F, Brandeis D, Strauch I, Lehmann D . (1981): Sleep deprivation: Effect on sleep stages and EEG power density in man. Electroenceph Clin Neurophysiol 51: 483–493
Borbély AA, Tobler I, Hanagasioglu M . (1984): Effect of sleep deprivation on sleep and EEG power spectra in the rat. Behav Brain Res 14: 171–182
Borbély AA, Tononi G . (1998): The quest for the essence of sleep. Daedalus. Proc Am Acad Arts Sci 127: 167–196
Borbély AA, Trachsel L, Tobler I . (1988): Effect of ritanserin on sleep stages and sleep EEG in the rat. Eur J Pharmacol 156: 275–278
Declerck AC, Wauquier A, Van der Ham-Veltman PHM, Gelders Y . (1987): Increase in slow-wave sleep in humans with the serotonin-S2 antagonist ritanserin. The first exploratory polygraphic sleep study. Curr Ther Res Clin Exp 41: 427–432
Dijk DJ, Beersma DGM, Daan S, van den Hoofdakker RH . (1989): Effects of seganserin, a 5-HT2 antagonist, and temazepam on human sleep stages and EEG power spectra. Eur J Pharmacol 171: 207–218
Dijk DJ, Brunner DP, Borbély AA . (1990): Time course of EEG power density during long sleep in humans. Am J Physiol 258: R650–R661
Dijk DJ, Hayes B, Czeisler CA . (1993): Dynamics of electroencephalographic sleep spindles and slow wave activity in men: Effect of sleep deprivation. Brain Res 626: 190–199
Driver HS, Flanigan MJ, Bentley AJ, Luus HG, Shapiro CM, Mitchell D . (1995): The influence of ipsapirone, a 5-HT1A agonist, on sleep patterns of healthy subjects. Psychopharmacology 117: 186–192
Feinberg I, Floyd TC . (1979): Systematic trends across the night in human sleep cycles. Psychophysiology 16: 283–291
Gillin JC, Jernajczyk W, Valladares-Neto D, Golshan S, Lardon M, Stahl SM . (1994): Inhibition of REMS by ipsapirone, a 5-HT1A agonist, in normal volunteers. Psychopharmacology 116: 433–436
Gillin JC, Sohn JW, Stahl SM, Lardon M, Kelsoe J, Rapaport M, Ruiz C, Golshan S . (1996): Ipsapirone, a 5-HT1A agonist, suppresses REMS equally in unmedicated depressed patients and normal controls. Neuropsychopharmacology 15: 109–115
Hoyer D, Martin GR . (1996): Classification and nomenclature of 5-HT receptors: A comment on current issues. Behav Brain Res 73: 263–268
Humphrey PPA, Hartig P, Hoyer D . (1993): A proposed new nomenclature for 5-HT receptors. Trends Pharmacol Sci 14: 233–236
Idzikowski C, Mills FJ, Glennard R . (1986): 5-Hydroxytryptamine-2 antagonist increases human slow wave sleep. Brain Res 378: 164–168
Jouvet M . (1972): The role of monoamines and acetylcholine-containing neurons in the regulation of the sleep-waking cycle. Ergebn Physiol 64: 166–307
Lesch KP, Poten B, Söhnle K, Schulte HM . (1990): Pharmacology of the hypothermic response to 5-HT1A receptor activation in humans. Eur J Clin Pharmacol 39: 17–19
McCormick DA . (1992): Neurotransmitter actions in the thalamus and cerebral cortex and their role in neuromodulation of thalamocortical activity. Prog Neurobiol 39: 337–388
McCormick DA, Bal T . (1997): Sleep and arousal: Thalamocortical mechanisms. Annu Rev Neurosci 20: 185–215
McCormick DA, Wang Z . (1991): Serotonin and noradrenaline excite GABAergic neurons of the guinea pig and cat nucleus reticularis thalami. J Physiol 442: 235–255
Pazos A, Probst A, Palacios JM . (1987): Serotonin receptors in the human brain. IV. Autoradiographic mapping of serotonin-2 receptors. Neuroscience 21: 123–239
Portas CM, Bjorvatn B, Fagerland S, Grønli S, Mundal V, Sørensen E, Ursin R . (1998): On-line detection of extracellular levels of serotonin in dorsal raphe nucleus and frontal cortex over the sleep/wake cycle in the freely moving rat. Neuroscience 83: 807–814
Rechtschaffen A, Kales A . (eds) (1968):A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Sleep. Washington, D.C.: Public Health Service, U.S. Government Printing Office
Rinaldi-Carmona M, Cogny C, Santucci V, Simiand J, Gautret B, Neliat G, Labeeuw B, Le Fur G, Soubrie P, Breliere JC . (1992): Biochemical and pharmacological properties of SR 46349B, a new potent and selective 5-hydroxytryptamine2 receptor antagonist. J Pharmacol Exp Ther 262: 759–768
Saucier C, Morris SJ, Albert PR . (1998): Endogenous serotonin-2A and -2C receptors in Balb/c-3T3 cells revealed in serotonin-free medium: Desensitization and down-regulation by serotonin. Biochem Pharmacol 56: 1347–1357
Schwartz PJ, Wehr TA, Rosenthal NE, Bartko JJ, Oren DA, Luetke C, Murphy DL . (1995): Serotonin and thermoregulation: Physiologic and pharmacologic aspects of control revealed by intravenous m-CPP in normal human subjects. Neuropsychopharmacology 13: 105–115
Seifritz E, Moore P, Trachsel L, Bhatti T, Stahl SM, Gillin JC . (1996): The 5-HT1A agonist ipsapirone enhances EEG slow wave activity in human sleep and produces a power spectrum similar to 5-HT2 blockade. Neurosci Lett 209: 41–44
Sharpley AL, Elliott JM, Attenburrow M-J, Cowen PJ . (1994): Slow wave sleep in humans: Role of 5-HT2A and 5-HT2C receptors. Neuropharmacology 33: 467–471
Steriade M, Contreras D, Amzica F . (1994): Synchronized sleep oscillations and their paroxysmal developments. Trends Neurosci 17: 199–208
Steriade M, McCormick DA, Sejnowski TJ . (1993): Thalamocortical oscillations in the sleeping and aroused brain. Science 262: 679–685
Tissier MH, Lainey E, Fattaccini CM, Hamon M, Adrien J . (1993): Effects of ipsapirone, a 5-HT1A agonist, on sleep/wakefulness cycles: Probable post-synaptic action. J Sleep Res 2: 103–109
Tobler I, Borbély AA . (1990): The effect of 3-h and 6-h sleep deprivation on sleep and EEG spectra of the rat. Behav Brain Res 36: 73–78
Werth E, Achermann P, Borbély AA . (1997): Fronto-occipital EEG power gradients in human sleep. J Sleep Res 6: 102–112
Werth E, Achermann P, Borbély AA . (1998): Regional differences in the sleep EEG: Functional implications. Sleep 21(suppl):207
Werth E, Dijk DJ, Achermann P, Borbély AA . (1996): Dynamics of the sleep EEG after an early evening nap: Experimental data and simulations. Am J Physiol 271: R501–R510
Acknowledgements
We thank Dr. Corinne Roth for her assistance with the experiment and Dr. Irene Tobler for comments on the manuscript. This research was supported by SANOFI Recherche, the Swiss National Science Foundation (Grant Nr. 3100–042500.94 and 3100–053005.97) and the Human Frontiers Science Program RG 81/96.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Landolt, HP., Meier, V., Burgess, H. et al. Serotonin-2 Receptors and Human Sleep: Effect of a Selective Antagonist on EEG Power Spectra. Neuropsychopharmacol 21, 455–466 (1999). https://doi.org/10.1016/S0893-133X(99)00052-4
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00052-4
Keywords
This article is cited by
-
An examination of sleep spindle metrics in the Sleep Heart Health Study: superiority of automated spindle detection over total sigma power in assessing age-related spindle decline
BMC Neurology (2023)
-
Genetic endophenotypes for insomnia of major depressive disorder and treatment-induced insomnia
Journal of Neural Transmission (2019)
-
Sleep as a Therapeutic Target in the Aging Brain
Neurotherapeutics (2019)
-
Selective Serotonin 5-HT2A Receptor Antagonists and Inverse Agonists Specifically Promote Slow Wave Sleep (Stage N3) in Man
Sleep and Vigilance (2017)
-
Differential regulation of observational fear and neural oscillations by serotonin and dopamine in the mouse anterior cingulate cortex
Psychopharmacology (2014)