Abstract
Peroxisome proliferator-activated receptor (PPAR) is a ligand-activated transcriptional factor that regulates lipid metabolism and inflammation. Behavioral sensitization is an experimental model of psychostimulant psychosis; it is elicited by repeated administration of psychostimulants and has recently been implicated in brain inflammation. We examined the involvement of PPARγ, one of the isotypes of PPAR, in development of behavioral sensitization to the stimulant effect of methamphetamine (METH) (1 mg/kg, subcutaneously) in mice. Repeated administration of METH (once daily for 5 days) enhanced the locomotor-activating effect of METH, which was reproduced by METH challenge on withdrawal day 7 (test day 12). The protein level and the activity of PPARγ were significantly increased in the nuclear fraction of whole brain after 5 days of METH administration (test day 5) and on withdrawal day 7 (test day 12). Both pioglitazone and ciglitazone (PPARγ agonists; 0.5–5.0 μg, intracerebroventricularly (i.c.v.), once daily) prevented the expression of behavioral sensitization to METH challenge on withdrawal day 7, but not the sensitization that occurred during repeated administration of METH. In addition, the magnitude of expression of behavioral sensitization was augmented by treatments with GW9662 (a PPARγ antagonist; 0.5–5.0 μg i.c.v., once daily) during the withdrawal period. The pioglitazone-induced alleviation of behavioral sensitization was synergistically facilitated by simultaneous i.c.v. injection of 9-cis-retinoic acid (1.0 μg), an agonist for the retinoid X receptor which is a ligand-activated nuclear receptor that forms heterodimers with PPAR. These results suggest that PPARγ has a significant role in the expression of behavioral sensitization to METH in mice.
Similar content being viewed by others
INTRODUCTION
Psychostimulants act on the mesolimbic dopamine system to elicit psychomotor excitation, such as increases in locomotor activity in animals. The repeated administration of psychostimulants to animals produces a progressive increase in locomotor activity over time, referred as to behavioral sensitization. The enhanced locomotor response to the stimulant is long lasting and can be elicited by a challenge dose of the drug after chronic administration has been discontinued. Behavioral sensitization is believed to be a model for stimulant psychosis in human, because the time course is similar to the transition to psychosis (Ujike, 2002) and sensitization has been used as an indicator of the development of drug addiction (Robinson and Berridge, 1993). Many studies have shown the possible cellular mechanisms underlying behavioral sensitization to psychostimulants (Nestler and Malenka, 2004), and much effort has been made to develop pharmacotherapies for drug addiction (O'Brien, 1997). Although several potential pharmacological treatments have been reported in individual studies to produce significant reductions in drug use, none has been found to be associated with consistent improvement in controlled clinical trials (O'Brien, 2001).
Inflammation of the central nervous system (CNS), neuroinflammation, is an important but poorly understood part of neurological disease. After acute brain injury or infection, there is a complex inflammatory response that involves activation of microglia and astrocytes and increased production of inflammatory chemical mediators (Lucas et al, 2006). It is possible that neuroinflammation contributes to cell death and damage during neurologic and neuropsychiatric diseases (McLeod et al, 2001). Recent studies have suggested that inflammatory mediators play a role in some effects of psychostimulants. Interleukin-6 (IL-6) increased sensitivity to the locomotor-activating effects of amphetamine (Zalcman et al, 1999), whereas tumor necrosis factor-α (TNF-α) blocked the acute effect of methamphetamine (METH) on locomotor activity and the development of sensitization to METH (Nakajima et al, 2004). In addition, nonsteroidal anti-inflammatory drugs (NSAIDs) protected striatal neurons against METH-induced neurotoxicity in mice (Asanuma et al, 2004). These reports indicate that neuroinflammation processes are involved in the effects of psychostimulants in the CNS.
Peroxisome proliferator-activated receptor (PPAR) is a ligand-activated transcription factor belonging to a nuclear hormone receptor superfamily. Three PPAR isoforms (α, β, and γ) have been identified and can be translocated to the nuclear fraction of cells as heterodimers with the retinoid X receptor (RXR). The ligand-activated heterodimers can bind to PPAR response element (PPRE) to regulate the transcription of target genes. It is well known that some fatty acids and prostanoids are natural ligands and NSAIDs, thiazolidinedione (TZD), and fibrates are clinically used ligands for PPARγ.
PPARγ plays a critical physiological role as primary lipid sensors and regulators of lipid metabolism. Thus, its ligands are clinically used for treatment of some diseases, including type 2 diabetes and hyperglycemia (Evans et al, 2004). However, PPARγ has additional effects on cellular physiology. More recently, it was found that activation of PPARγ mediated anti-inflammation in the cardiovascular system and the nervous system (Daynes and Jones, 2002). PPARγ ligands, therefore, have potential therapeutic use for inflammatory neurological diseases, such as Alzheimer's disease and multiple sclerosis (Feinstein, 2003). This evidence prompts us to question whether PPAR ligands might modify behavioral sensitization to the psychomotor effect of stimulants.
In the present study, we first examined the involvement of PPARγ in behavioral sensitization to the stimulant effects of METH in mice. The influence of METH administration on the expression and transcription activity of PPARγ was examined in the brain of mice using Western blotting and electrophoretic mobility shift assay (EMSA). Next, the effect of PPARγ ligands on behavioral sensitization to the stimulant effects of METH in mice was examined. We here present several lines of evidence that indicate that PPARγ plays an inhibitory role in the expression of behavioral sensitization to METH.
MATERIALS AND METHODS
Behavioral Experiment
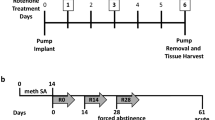
Male ICR mice (SLC, Hamamatsu, Japan) weighing 25–35 g were used. They were housed 5 to a cage in an air-conditioned (23–24°C, 60% humidity) and light-controlled (lights on from 0800 to 2000 hours) room. All drug injections and behavioral testing were performed during the light cycle. Mice were given either subcutaneous (s.c.) saline or METH (1 mg/kg) once a day for 5 consecutive days, and were then given no injections for 6 days. On day 7 of withdrawal, animals received a single injection of saline or METH, referred to as challenge. The PPAR ligands were administered intracerebroventricularly (i.c.v.) to mice once a day for 5 days from test day 1 to 5 (in Figure 4) or for 6 days from test day 6 to 11 (in Figures 5 and 6). Locomotor activity was measured in a 31 × 36 cm cage in a chamber with an array of fresnel lenses above the cage, which monitored motion in multiple zones of the cage (CompACT AMS, Muromachi Kikai, Tokyo, Japan). Animals received a single s.c. injection of saline and were left in the measurement cages for 3 h on the day before day 1 of METH treatment to allow them to adapt to the measurement environment and injection procedure. On the treatment days and on day 7 of withdrawal, animals were further habituated to the locomotor cages for 3 h. After habituation, animals received the injections, and subsequent locomotor activity was monitored for 3 h. All procedures were approved by Animal Research Committee of Wakayama Medical University in accordance with the Japanese Government Animal Protection and Management Law, Japanese Government Notification on Feeding and Safekeeping of Animals, and The Guidelines for Animal Experiments in Wakayama Medical University (approval number 64).
No significant effect of concurrent administration of PPAR ligands on the development of behavioral sensitization to METH. As indicated in (a), mice were treated with saline (SAL) or METH once a day for consecutive 5 days, and then received SAL or METH (1 mg/kg) challenge on day 7 of withdrawal (test day 12), referred to as SAL group or METH group, respectively. Vehicle (VEH), ciglitazone (CIG; 5 μg), pioglitazone (PIO; 5 μg), or GW9662 (GW; 5 μg) was i.c.v. injected to both the groups once a day 3 h before SAL or METH on days 1–5. The locomotor testing was performed after SAL or METH administration. Bar graphs show the total locomotor activity on day 5 (b) and on day 12 (c) (n=5). Statistically significant difference between treatments was determined by one-way ANOVA. (b) SAL group, F(3,19)=2.77, P=0.0752; METH group, F(3,19)=1.12, P=0.3722. (c) SAL group, F(3,19)=2.56, P=0.1373; METH group, F(3,19)=1.43, P=0.2714.
The expression of behavioral sensitization to METH is affected by injection of PPARγ ligands over the withdrawal period. (a) Drug regimen. (b) No influence of PPARγ ligands on the locomotor-stimulating effect of a single administration of METH in saline-treated mice on day 12. (c) Dose-dependent effect of PPARγ ligands on the expression of the enhanced stimulating effect emerged by METH challenge in METH-treated mice on day 12. Mice took the drug administration followed by locomotor testing; saline (SAL) or METH (1 mg/kg) were administered to animals once a day from day 1 to 5. From day 6 to 11, animals were treated with i.c.v. injection of vehicle (VEH), ciglitazone (CIG), pioglitazone (PIO), or GW9662 (GW) once a day, and then received METH (1 mg/kg) challenge on day 7 of withdrawal (test day 12). Statistically significant difference was determined by a one-way ANOVA followed by Dunnett's t test. (b) F(3,33)=0.08, P=0.9232, n=8. (c) F(9,69)=19.01, P<0.0001, n=6–8. *P<0.05 and **P<0.01 vs VEH.
Effect of 9-cis retinoic acid (R) on the expression of behavioral sensitization to METH. (a) Dose-dependent effect of R on the locomotor-stimulating effect induced by METH challenge in mice repeatedly treated with METH. Mice took the drug administration followed by locomotor testing. Vehicle (VEH) or R (0.3–3.0 μg) was i.c.v. injected to the mice developing behavioral sensitization to METH once a day on days 6–11, and then received METH challenge (1 mg/kg) on day 12 (n=6–7). (b) R potentiates inhibitory effect of pioglitazone (P) on maintained enhancement of locomotor-stimulating effect of METH. Saline (SAL group) or METH (METH group; 1 mg/kg) were administered to mice once a day from days 1 to 5. From days 6 to 11, animals were treated with i.c.v. injection of VEH, P (1.5 μg), R (1.0 μg), or P+R once a day, and then received METH challenge (1 mg/kg) on day 12 (n=6–8). Statistically significant difference was determined by a one-way ANOVA followed by Dunnett's test in (a) or Tukey–Kramer test in (b). (a) F(3,27)=3.23, P=0.0471. (b) SAL group, F(3,27)=2.39, P=0.1193; METH group, F(3,27)=9.82, P=0.0002. *P<0.05 and **P<0.01 vs VEH.
Immunohistochemistry
Six hours after saline or METH administration, mice were deeply anesthetized with pentobarbital (50 mg/kg) and perfused transcardially with cold phosphate-buffered saline, followed by 4% paraformaldehyde in phosphate buffer. The brains were removed, postfixed in the same fixative for 4 h, and then cryoprotected in 30% sucrose in phosphate buffer. The brains were cut into 20 μm coronal sections on a cryostat, and free-floating sections were used for PPARγ immunohistochemistry. The sections were incubated for 1 h with 2.5% non-fat dry milk and 0.1% Triton X-100 in 0.02 M Tris buffer and then incubated with rabbit anti-PPARγ antibody (1 : 100; sc-7196, Santa Cruz Biotechnology, Santa Cruz, CA, USA) for 48 h at 4°C. Sections were then washed with Tris buffer and incubated with 0.8% non-fat dry milk and 0.03% Triton X-100 in 0.02 M Tris buffer containing biotinylated goat anti-rabbit antibody (1 : 200) at room temperature for 1 h. Sections were washed and processed with avidin-biotinylated horseradish peroxidase (HRP) complex (Vector ABC kit, Vector Laboratories, Burlingame, CA, USA), and the reaction was visualized using diaminobenzidine. The immunohistochemically stained sections were observed with a light microscope. A selected brain area was the nucleus accumbens (NAcs) in sections at a level of 1.70 mm from bregma according to the atlas of Franklin and Paxinos (1997).
Preparation of Nuclear Fraction
Mice were killed by instantaneous dislocation of the neck, an appropriate method of humane killing, followed by removal of the whole brains without pons, medulla, and cerebellum. The whole brain was homogenized using a motor-driven glass-Teflon homogenizer in 3.5 ml of ice-cold hypotonic solution adjusted at pH 7.9 : 10 mM HEPES, 10 mM KCl, 1.5 mM MgCl2, 0.5 mM dithiothreitol (DTT), 1 mM phenylmethylsulfonyl fluoride (PMSF), and 1 μg/ml aprotinin. The homogenates were incubated on ice for 10 min. After addition of 1% Nonidet P-40, samples were further homogenized. The homogenate was centrifuged at 250g for 10 min and the resultant pellets were suspended in 0.45 ml of a lysis hypertonic solution adjusted at pH 7.9 : 5 mM HEPES, 20% glycerol, 400 mM NaCl, 1.5 mM MgCl2, 0.5 mM DTT, 1 μg/ml aprotinin, and 1 mM PMSF. After incubation on ice for 45 min, the suspension was centrifuged at 18 000g for 30 min at 4°C, and the resultant supernatants were retained as the nuclear extracts at −70°C.
Western Blotting
The protein concentration of the prepared nuclear extract was evaluated by the Bradford method and adjusted to 5 μg/μl. The following sample buffer was added in equal proportion to the extract, followed by boiling for 7 min: 0.5 M Tris, 10% sodium dodecylsulfate (SDS), 10% glycerol, 0.5% 2-mercaptoethanol, and 1% bromophenol blue. Proteins in the sample were separated by size on 7.5% SDS-polyacrylamide gel and transferred to nitrocellulose membranes in blotting buffer: 25 mM Tris, 192 mM glycine, 0.05% SDS, and 20% methanol. The transferred membranes were blocked at 4°C overnight by the blocking buffer: 10% non-fat-dried milk in Tris-buffered saline (20 mM at pH 7.6) containing 0.05% Tween 20 (Tween-TBS). The membrane was incubated at 4°C overnight and subsequently at room temperature for 1 h in rabbit anti-PPARγ polyclonal antibody diluted in Tween-TBS including the 5% non-fat-dried milk. Then, the membrane was incubated at room temperature for 2 h in secondary antibody, HRP-conjugated goat anti-rabbit IgG diluted in Tween-TBS containing 5% non-fat-dried milk. Chemiluminescence of the antigen-antibody peroxidase complex was performed by LumiGLO Reagent and Peroxide (PIERCE, Rockford, IL, USA), and detected by Chemiluiminator (ATTO, Tokyo, Japan) and analyzed by NIH image (NIH, Bethesda, MD, USA).
Electrophoretic Mobility Shift Assay
EMSA was performed for the determination of PPARγ activation using EMSA Gel-Shift Kits according to the manufacturer's instruction (Panomics, Redwood, CA, USA). The DNA probe containing the PPRE (Juge-Aubry et al, 1997) was double-stranded oligonucleotides labeled with biotin, provided by the manufacturer. The probe (10 ng) and the nuclear extracts (5 μg) were incubated for 30 min at 15°C in binding buffer with 1 μg poly d(I-C). In another experiment, rabbit anti-PPARγ polyclonal antibody was added to the reaction mixture. The DNA–protein complexes were separated at 4°C at 120 V by 6% polyacrylamide gel electrophoresis in Tris-borate buffer: 50 mM Tris, 45 mM boric acid, and 0.5 mM EDTA. The complexes were then transferred for 30 min at 300 mA to nylon membranes (Biodyne B, PALL, Tokyo, Japan) in blotting buffer: 25 mM Tris, 192 mM glycine, 0.05% SDS, and 20% methanol. The membrane was baked for 30 min at 85°C in a dry oven. For chemiluminescence of the DNA–protein complexes, the baked membrane was incubated at room temperature for 15 min with blocking buffer including streptavidin-HRP conjugate, followed by incubation with substrate solution at room temperature for 5 min. The chemiluminescence was detected by Chemiluiminator and analyzed by NIH image.
Drugs
METH hydrochloride (Dainippon Pharmaceutical Company, Osaka, Japan) was dissolved in saline. The following drugs were dissolved in 5% polyethyleneglycol and 5% Tween 80 in saline: ciglitazone, pioglitazone, and GW9662 (Sigma-Aldrich, St Louis, MO, USA); 9-cis-retinoic acid (BIOMOL, Plymouth Meeting, PA, USA). The other chemicals were purchased from Nacalai Tesque (Kyoto, Japan) or Wako Pure Chemical Industries (Osaka, Japan).
Statistical Analysis
Data represent the mean ±SEM. Statistical significance between unpaired groups was assessed by using a one-way analysis of variance (ANOVA) test followed by Dunnett's post hoc test (Figures 1, 2a, 3, 5c and 6a) or a two-way ANOVA followed by Bonferroni post hoc test (Figure 1) for multiple comparisons in the experiments on time-dependency of and dose-dependency of effects of tested drugs on behavioral sensitization. In other experiments, a one-way ANOVA was followed by Tukey–Kramer post hoc test (Figures 4, 5b and 6b). Significance was set at P<0.05 level.
Repeated administration of METH (1 mg/kg) developed behavioral sensitization in mice. Mice were given the drug administration followed by locomotor testing; saline (n=8) or METH (n=8) was administered to animals once a day from day 1 to 5. Animals received METH (1 mg/kg) challenge on day 7 of withdrawal (test day 12). The ordinate indicates the total amount of locomotor activity for 3 h after administration. Statistically significant difference between treatments was determined by a two-way ANOVA followed by Bonferroni test (vs saline): treatment, F(3,19)=27.48, P<0.0001; test day, F(3,19)=749.85, P<0.0001; interaction, F(3,19)=28.85, P<0.0001; ##P<0.01 vs saline. Statistically significant difference between test day was determined by a one-way ANOVA followed by Dunnett's test (vs day 1): saline, F(5,47)=7.48, P=0.0002; METH, F(5,47)=6.97, P=0.0009; *P<0.05 and ***P<0.001 vs on 1st day.
Expression of PPARγ progressively increased in the brain of mice repeatedly treated with METH (1 mg/kg). (a) Detection of PPARγ protein by Western blot. Upper data represent Western blot analysis of PPARγ in the brain. METH was administered to animals once a day from day 1 to 5, and mice were killed 6 h after its administration on days 1, 3, or 5 and without METH challenge on day 12 (7DW; day 7 of withdrawal). The whole brain was removed, and the nuclear extracts were prepared for Western blotting. Values are mean±SEM. Statistically significant difference between test day was determined by one-way ANOVA (F(4,19)=7.92, P=0.0003) followed by Dunnett's test: *P<0.05 and **P<0.01 vs saline (SAL) (n=4). (b) Expression of PPARγ in the NAc of mice. Mice were killed 6 h after METH administration on day 5 of its treatment. As control, naive mice received a single administration of saline and were killed 6 h after its administration. Sections including the ventral striatum were stained for PPARγ with diaminobenzidine (dark gray dots) and examined by light microscopy. (ac) Anterior commissure. A scale bar indicates 50 μm.
Time response analysis of the effect of METH on PPARγ activation. A photograph is representative chemiluminescence image of the EMSA. A line graph shows the effect of METH on PPARγ activation. Mice treated with METH were killed 6 h after its administration. The whole brain was removed, and the nuclear extracts were prepared for EMSA. Values are mean±SEM (n=4). Statistically significant difference between test day was determined by one-way ANOVA (F(4,19)=65.25, P<0.0001) followed by Dunnett's test: ***P<0.001 vs saline (SAL).
RESULTS
Development of Behavioral Sensitization to METH
Repeated administration of METH induced a progressive increase in locomotor activity in mice (Figure 1). Two-way ANOVA revealed that there was significant difference between saline and METH treatment (F(3,19)=749.85; P<0.001), between saline and METH treatment on the test days (F(3,19)=27.48; P<0.001) and a significant interaction between those factors (F(3,19)=28.85; P<0.001; treatment x test day). The locomotor activity was significantly greater on day 5 of treatment than on day 1 of treatment in mice receiving repeated administration of METH (q=9.35; P<0.01; Dunnett's test).
To test whether our regimen of METH administration produced long-lasting locomotor sensitization, the mice pretreated with saline or METH were challenged with 1.0 mg/kg METH on day 7 of withdrawal (test day 12). Mice receiving repeated administration of METH showed enhanced augmentation of locomotor activity on test day 12 (withdrawal day 7) (q=8.02; P<0.01 vs on day 1; Dunnett's test). The locomotor activity was also significantly greater in METH-treated mice with METH challenge, compared with saline-treated animals with METH challenge (q=11.55; P<0.01; Bonferroni test).
Effects of METH on Expression and Activity of PPARγ
To test whether METH administration affects PPARγ expression, we examined the protein levels of PPARγ in the nuclear extract on various days of treatment with METH (Figure 2a). Repeated administration of METH produced a progressive increase in the level of PPARγ over treatment days (F(4,19)=7.92, P=0.0003; one-way ANOVA followed by Dunnett's test). Significant METH-induced increment in PPARγ was observed on day 5 (q=4.26; P<0.01), but not on day 1 (q=0.17; P>0.05) or day 3 (q=1.59; P>0.05), compared with saline treatment. The METH-induced PPARγ increment remained significant on day 7 of METH withdrawal (test day 12) (q=3.42; P<0.01).
Concomitantly, we studied the expression of PPARγ in the NAcs, a primary locus related to behavioral sensitization. In saline-treated mice, some PPARγ immunoreactive cells were observed (Saline in Figure 2b). An increase in PPARγ immunoreactivity was observed on day 5 of METH treatment (METH in Figure 2b). The PPARγ activity was assessed by EMSA in the nuclear fraction of whole brain in mice (Figure 3). A slightly shifted signal corresponding to protein binding on the DNA probe was detected in the nuclear extracts from mice treated with saline. Significant increases in PPARγ activity appeared in the nuclear extracts from animals on day 5 of METH treatment (F(4,19)=65.25, P<0.0001; one-way ANOVA), compared with saline treatment (q=10.81; P<0.01; Dunnett's test). METH challenge on day 12 produced a significant increase in PPARγ activity (q=11.09; P<0.01 vs saline; Dunnett's test).
Effects of PPARγ Ligands on METH Sensitization
To reveal the pathophysiological significance of the elevated activity of PPARγ by the METH regimen, we examined the effects of PPARγ ligands on behavioral sensitization to METH. PPARγ ligands (5 μg i.c.v.) were administered concurrently with METH (1 mg/kg s.c.) once a day for 5 consecutive days (Figure 4a). The TZD derivative PPARγ agonists, ciglitazone and pioglitazone, and the PPARγ antagonist GW9662 were co-administered with METH. Mice treated with saline did not show significant change in locomotor activity on day 5, regardless of which PPARγ ligand was co-administered (F(3,19)=2.77; P>0.05; Figure 4b). No tested PPARγ ligands produced significant effects on the elevated locomotor stimulation produced by daily METH administration on day 5 (F(3,19)=1.12; P>0.05; Figure 4b). In addition, the locomotor activity on day 12 was not significantly changed by concurrent administration of any PPARγ ligand with saline (F(3,19)=2.56; P>0.05; Figure 4c) or METH (F(3,19)=1.43; P>0.05; Figure 4c).
We next examined the effects of PPARγ ligands on the expression of METH sensitization. The PPARγ ligands (0.5–5.0 μg i.c.v.) were injected once a day during the period of withdrawal from METH (on days 6–11), followed by METH challenge on day 12 (Figure 5a). None of the PPARγ ligands (5 μg) altered the increase in locomotor activity induced by METH challenge in saline-treated mice (F(3,33)=0.08; P>0.05; Figure 5b). On the other hand, both of the PPARγ agonists produced dose-dependent attenuation in the increase in locomotor activity induced by METH challenge in METH-treated mice (F(9,69)=19.01; P<0.0001; Figure 5c): ciglitazone (q=3.78; P<0.01 in 5 μg vs vehicle; Dunnett's test); pioglitazone (q=3.73; P<0.01 in 5 μg vs vehicle). In contrast, the enhanced locomotor-stimulating effect of METH was significantly augmented by GW9662 at 1.5 μg (q=3.26; P<0.05 vs vehicle) and 5 μg (q=5.60; P<0.01 vs vehicle).
Effect of RXR Agonist on Pioglitazone-Induced Prevention of METH Sensitization
It has been shown that PPARγ activates transcription as a heterodimer with RXR, which can be stimulated by ligands of either RXR or its partner receptor and synergistically activated in the presence of both ligands (Aranda and Pascual, 2001). Therefore, we tested the effect of an RXR ligand, 9-cis-retinoic acid (i.c.v.), alone or in combination with pioglitazone on the expression of behavioral sensitization to METH (Figure 6). Mice were treated with saline or METH followed by i.c.v. injection of pioglitazone or 9-cis-retinoic acid once a day for 6 consecutive days following withdrawal from METH, and received the METH challenge on day 12. Injection of 9-cis-retinoic acid alone (0.3–3 μg) reduced the METH challenge-induced increase in locomotor activity in a dose-dependent manner (F(3,27)=3.23, P<0.05, one-way ANOVA; q=3.02, P<0.05 in 3.0 μg vs vehicle, Dunnett's test; Figure 6a). We next used pioglitazone and 9-cis-retinoic acid at 1.5 μg and 1.0 μg, respectively, doses at which the drugs alone produced no significant effect (see Figures 5c and 6a), to examine the effect of their simultaneous injection on the METH challenge-induced effect (Figure 6b). 9-cis-retinoic acid, pioglitazone, or combinations of them did not alter the METH challenge-induced stimulant effect in saline-treated mice (F(3,27)=2.39, P>0.05). Simultaneous injection of 9-cis-retinoic acid and pioglitazone, however, significantly attenuated the METH challenge-induced stimulant effect, although administration of either drug alone was without significant effect in METH-treated mice (F(3,27)=9.82, P<0.001, one-way ANOVA; q=6.90, P<0.01 vs vehicle in METH group, Tukey–Kramer test; Figure 6b).
DISCUSSION
Behavioral sensitization, which develops with repeated administration of psychostimulants, is a neurobiological model for neural plasticity and a pathophysiological animal model for stimulant-induced psychosis and addiction in human. The accumulated evidence suggests possible mediators underlying behavioral sensitization. Effective pharmacotherapy, however, has not been established for drug psychosis that is elicited by repetitive drug administration. Recent studies proposed the involvement of inflammatory cytokines in the effects of METH on CNS function: IL-6 (Zalcman et al, 1999; Ladenheim et al, 2000) and TNF-α (Nakajima et al, 2004). We focused on PPARγ as a potential regulator of behavioral sensitization, because activation of PPARγ results in inhibition of the production of inflammatory mediators in several neurodegenerative diseases. The main result of the present study is the identification of PPARγ as a possible inhibitory mediator of the expression of behavioral sensitization.
The high doses of METH can induce neurotoxicity in the mesolimbic system. There is no study with the identical protocol to one in the present study, but some used METH at the higher dose and at the more number of injection times than in the present study to develop behavioral sensitization to METH. For example, once daily administration of 4 or 6 mg/kg METH for 14 consecutive days induced the upregulation of tyrosine hydroxylase (Chen and Chen, 2005) and increments of DA turnover (Nishikawa et al, 1983), which are markers for DA neuron activity commonly used in the investigation of METH-induced neurotoxicity. Thus, the protocol adopted in the present study is unlikely to induce neurotoxicity.
The NAc is a primary locus of the mesolimbic dopaminergic system involving the ventral tegmental area (VTA), which is responsible for the development of behavioral sensitization to psychostimulants. Immunohistochemical study revealed the expression of PPARγ in the NAc of naive mice (Figure 2a), which is consistent with reports by Moreno et al (2004). We found that repeated administration of METH increased PPARγ expression in the NAc after the final administration of METH (Figure 2b). These results indicate that PPARγ in the reward system is involved in behavioral sensitization to METH.
Upon stimulation by ligands for PPAR, PPAR and RXR bind to form a heterodimer in the cytosol, and subsequently are translocated to the nuclear fraction for transcriptional activation of their target genes (Bardot et al, 1993). Thus, Western blotting revealed that the expression of PPARγ was increased in the nuclear fraction of the whole brain of mice on day 5 of METH treatment (test day 5) and on day 7 of withdrawal from METH (test day 12) (Figure 2a). EMSA elucidated a significant increase in transcriptional activity of PPARγ in the same chronological order as the change in the level of PPARγ in mice with the METH regimen (Figure 3). The transactivation, however, was not significantly changed on day 1 of METH treatment, which indicates that a single administration of METH had no effect on the transactivation of PPARγ. These results strongly suggest that our regimen with METH induces increase in the PPARγ with enhanced transcriptional activity in the nuclear fraction. Furthermore, the time course of PPARγ expression and activity was similar to that of locomotor activity in mice receiving repeated administration of METH (Figures 1, 2 and 3). These results demonstrate that the development of behavioral sensitization is associated with increments of PPARγ expression.
It is not clear how repeated administration of METH activates PPARγ in the brain, because there are no reports on the involvement of the PPARγ activity in the effects of psychostimulants. The signals that regulate PPARγ expression are not well characterized, especially in the CNS, whereas the activation of inflammatory pathways leads to PPARγ expression in peripheral organs (Crosby et al, 2006). A candidate for an upstream molecule that regulates PPARγ expression in the CNS might be CCAAT enhancer-binding proteins (C/EBPβ), which is an inflammatory transcription factor and can upregulate PPARγ expression through binding to its element on PPARγ promoter region in peripheral organs (Wu et al, 1996). Moreover, it is interesting to note that C/EBPβ, RXRα, and PPARγ are all involved in astrocyte differentiation (Cristiano et al, 2005), which may contribute to the pathology of addiction and relapse (Bowers and Kalivas, 2003). This allows us to speculate that the upregulation of PPARγ by METH is a negative feedback control of astrocyte differentiation for relief of the enduring behavioral changes in METH addicts. The future studies are required to elucidate the mechanisms underlying PPARγ expression.
Upregulation and activation of PPARγ in METH-treated mice raises the question of what the pathophysiological significance of PPARγ activation is for behavioral sensitization. Treatment with each PPARγ agonist over the METH withdrawal period reduced maintained enhancement of the locomotor-activating effect of METH, whereas the same treatment with the PPARγ antagonist potentiated it (Figure 5c). Neither the PPARγ agonists nor the antagonist altered the locomotor-activating effect of a single administration of METH (Figure 5b). The involvement of PPARγ in the expression of behavioral sensitization is supported by the synergistically inhibitory effect of co-administration of the RXR ligand with the PPARγ ligand on behavioral sensitization (Figure 6b). Behavioral sensitization can be conceptualized into two distinct temporal domains termed initiation and expression (Robinson and Becker, 1986). Modifications in the VTA are involved in the induction of behavioral sensitization, and modifications in the NAc in the long-term maintenance (Vanderschuren and Kalivas, 2000). The present study found the increased expression of PPARγ in the NAc on day 5 of METH regimen (Figure 2b), associated with the significant increments of transactivation of PPARγ (Figure 3). These results suggest possible involvement of the activated PPAR in the NAc in the expression phase of behavioral sensitization. The phase-specific increments of PPARγ in the NAc might contribute to the phase-specific effectiveness of exogenously applied PPARγ ligands on behavioral sensitization to METH which is shown in Figures 4 and 5. These results suggest that ligand-activated PPARγ could modify specifically the consolidation, rather than induction, of the behavioral sensitization. Zalcman et al (1999) reported that IL-6, one of inflammatory cytokines, caused a lasting augmentation of responsiveness to psychostimulants. This might give an explanation to how the neuroinflammatory system activated by METH consolidates behavioral sensitization to METH: the thought of that can make a hypothesis that IL-6 is a candidate for inflammatory molecules involved in the expression phase of behavioral sensitization. That temporal characteristic could also be favorable for treating drug psychosis, because most patients suffer from craving and psychosis during drug withdrawal, but not in early phases of drug intake (Vocci et al, 2005).
Psychostimulants reportedly upregulate the expression of target genes via activation of inflammatory-responsive transcriptional factors. For example, psychostimulants stimulate activity of activator protein-1 (AP-1) and nuclear factor-κB (NF-κB), transcriptional factors which regulate a number of inflammatory gene expressions (Asanuma and Cadet, 1998; Lee et al, 2002). The expression of NF-κB is also induced in the NAc of mice treated chronically, but not acutely, with psychostimulants (Ang et al, 2001). The ligand-activated PPARγ inhibits NF-κB- and AP-1-driven transcription by physically interacting with NF-κB and AP-1 to weaken binding to DNA (Jiang et al, 1998). The inhibition leads to the reduction of inflammatory cytokines, such as IL-6 and TNF-α, because AP-1 and NF-κB can bind to the DNA element on the promoter region of the inflammatory cytokines encoding genes and activate transcription of the inflammatory cytokines gene as target genes (Chinetti et al, 2000). PPARγ possibly exerts anti-inflammatory activity in brain cells by reducing the expression of proinflammatory cytokines, nitric oxide synthase, and cyclooxygenase, through interfering with AP-1 and NF-κB (Feinstein, 2003). Thus, activation of PPARγ might be a pathway to halt the expression of METH sensitization. Indeed, an anti-inflammatory drug reportedly attenuated METH-induced neurotoxicity (Asanuma et al, 2004) and we also observed inhibitory effects of an NSAID on behavioral sensitization to METH (unpublished data).
In summary, this is the first demonstration that PPARγ is upregulated and activated in the brain cells by repeated injection of METH and modification of the activity of PPARγ results in alteration of the expression of behavioral sensitization in mice. More detailed analysis could lead to a promising remedy for psychostimulant psychosis with commonly used oral hypoglycemic agents, TZD derivatives, for which safety, at least in diabetics, has been established.
References
Ang E, Chen J, Zagouras P, Magna H, Holland J, Schaeffer E et al (2001). Induction of nuclear factor-kappaB in nucleus accumbens by chronic cocaine administration. J Neurochem 79: 221–224.
Aranda A, Pascual A (2001). Nuclear hormone receptors and gene expression. Physiol Rev 81: 1269–1304.
Asanuma M, Cadet JL (1998). Methamphetamine-induced increase in striatal NF-kappaB DNA-binding activity is attenuated in superoxide dismutase transgenic mice. Brain Res Mol Brain Res 60: 305–309.
Asanuma M, Miyazaki I, Higashi Y, Tsuji T, Ogawa N (2004). Specific gene expression and possible involvement of inflammation in methamphetamine-induced neurotoxicity. Ann NY Acad Sci 1025: 69–75.
Bardot O, Aldridge TC, Latruffe N, Green S (1993). PPAR-RXR heterodimer activates a peroxisome proliferator response element upstream of the bifunctional enzyme gene. Biochem Biophys Res Commun 192: 37–45.
Bowers MS, Kalivas PW (2003). Forebrain astroglial plasticity is induced following withdrawal from repeated cocaine administration. Eur J Neurosci 17: 1273–1278.
Chen PC, Chen JC (2005). Enhanced Cdk5 activity and p35 translocation in the ventral striatum of acute and chronic methamphetamine-treated rats. Neuropsychopharmacology 30: 538–549.
Chinetti G, Fruchart JC, Staels B (2000). Peroxisome proliferator-activated receptors (PPARs): nuclear receptors at the crossroads between lipid metabolism and inflammation. Inflamm Res 49: 497–505.
Cristiano L, Cimini A, Moreno S, Ragnelli AM, Paola Ceru M (2005). Peroxisome proliferator-activated receptors (PPARs) and related transcription factors in differentiating astrocyte cultures. Neuroscience 131: 577–587.
Crosby MB, Zhang J, Nowling TM, Svenson JL, Nicol CJ, Gonzalez FJ et al (2006). Inflammatory modulation of PPAR gamma expression and activity. Clin Immunol 118: 276–283 [E-pub 2005 November 2021].
Daynes RA, Jones DC (2002). Emerging roles of PPARs in inflammation and immunity. Nat Rev Immunol 2: 748–759.
Evans RM, Barish GD, Wang YX (2004). PPARs and the complex journey to obesity. Nat Med 10: 355–361.
Feinstein DL (2003). Therapeutic potential of peroxisome proliferator-activated receptor agonists for neurological disease. Diabetes Technol Ther 5: 67–73.
Franklin KBJ, Paxinos G (1997). The Mouse Brain in Stereotaxic Coordinates. Academic Press: San Diego.
Jiang C, Ting AT, Seed B (1998). PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature 391: 82–86.
Juge-Aubry C, Pernin A, Favez T, Burger AG, Wahli W, Meier CA et al (1997). DNA binding properties of peroxisome proliferator-activated receptor subtypes on various natural peroxisome proliferator response elements. Importance of the 5′-flanking region. J Biol Chem 272: 25252–25259.
Ladenheim B, Krasnova IN, Deng X, Oyler JM, Polettini A, Moran TH et al (2000). Methamphetamine-induced neurotoxicity is attenuated in transgenic mice with a null mutation for interleukin-6. Mol Pharmacol 58: 1247–1256.
Lee YW, Son KW, Flora G, Hennig B, Nath A, Toborek M (2002). Methamphetamine activates DNA binding of specific redox-responsive transcription factors in mouse brain. J Neurosci Res 70: 82–89.
Lucas SM, Rothwell NJ, Gibson RM (2006). The role of inflammation in CNS injury and disease. Br J Pharmacol 147: S232–240.
McLeod TM, Lopez-Figueroa AL, Lopez-Figueroa MO (2001). Nitric oxide, stress, and depression. Psychopharmacol Bull 35: 24–41.
Moreno S, Farioli-Vecchioli S, Ceru MP (2004). Immunolocalization of peroxisome proliferator-activated receptors and retinoid X receptors in the adult rat CNS. Neuroscience 123: 131–145.
Nakajima A, Yamada K, Nagai T, Uchiyama T, Miyamoto Y, Mamiya T et al (2004). Role of tumor necrosis factor-alpha in methamphetamine-induced drug dependence and neurotoxicity. J Neurosci 24: 2212–2225.
Nestler EJ, Malenka RC (2004). The addicted brain. Sci Am 290: 78–85.
Nishikawa T, Mataga N, Takashima M, Toru M (1983). Behavioral sensitization and relative hyperresponsiveness of striatal and limbic dopaminergic neurons after repeated METH treatment. Eur J Pharmacol 88: 195–203.
O'Brien CP (1997). A range of research-based pharmacotherapies for addiction. Science 278: 66–70.
O'Brien CP (2001). Drug addiction and drug abuse. In: Hardman JG, Limbird LE (eds). Goodman & Gilman's The Pharmacological Basis of Therapeutics. McGraw-Hill: New York. pp 621–642.
Robinson TE, Becker JB (1986). Enduring changes in brain and behavior produced by chronic amphetamine administration: a review and evaluation of animal models of amphetamine psychosis. Brain Res 396: 157–198.
Robinson TE, Berridge KC (1993). The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev 18: 247–291.
Ujike H (2002). Stimulant-induced psychosis and schizophrenia: the role of sensitization. Curr Psychiatry Rep 4: 177–184.
Vanderschuren LJ, Kalivas PW (2000). Alterations in dopaminergic and glutamatergic transmission in the induction and expression of behavioral sensitization: a critical review of preclinical studies. Psychopharmacology 151: 99–120.
Vocci FJ, Acri J, Elkashef A (2005). Medication development for addictive disorders: the state of the science. Am J Psychiatry 162: 1432–1440.
Wu Z, Bucher NL, Farmer SR (1996). Induction of peroxisome proliferator-activated receptor gamma during the conversion of 3T3 fibroblasts into adipocytes is mediated by C/EBPbeta, C/EBPdelta, and glucocorticoids. Mol Cell Biol 16: 4128–4136.
Zalcman S, Savina I, Wise RA (1999). Interleukin-6 increases sensitivity to the locomotor-stimulating effects of amphetamine in rats. Brain Res 847: 276–283.
Acknowledgements
We are grateful to Dr James H Woods and Dr Gail Winger for advice concerning this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, T., Kiguchi, N., Fukazawa, Y. et al. Peroxisome Proliferator-Activated Receptor Gamma Activation Relieves Expression of Behavioral Sensitization to Methamphetamine in Mice. Neuropsychopharmacol 32, 1133–1140 (2007). https://doi.org/10.1038/sj.npp.1301213
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301213
Keywords
This article is cited by
-
PPARα and PPARγ are expressed in midbrain dopamine neurons and modulate dopamine- and cannabinoid-mediated behavior in mice
Molecular Psychiatry (2023)
-
Molecular mechanisms of morphine tolerance and dependence; novel insights and future perspectives
Molecular and Cellular Biochemistry (2023)
-
Cannabidiol but not cannabidiolic acid reduces behavioural sensitisation to methamphetamine in rats, at pharmacologically effective doses
Psychopharmacology (2022)
-
Beta-caryophyllene inhibits cocaine addiction-related behavior by activation of PPARα and PPARγ: repurposing a FDA-approved food additive for cocaine use disorder
Neuropsychopharmacology (2021)
-
PPARγ activation by pioglitazone does not suppress cravings for alcohol, and is associated with a risk of myopathy in treatment seeking alcohol dependent patients: a randomized controlled proof of principle study
Psychopharmacology (2020)