Abstract
Combined serotonin-2A (5-HT2A) and dopamine-2 (D2) receptor blockade has been proposed as a candidate mechanism by which second-generation antipsychotics (SGAs) improve both cognition and negative symptoms in schizophrenic patients, in contrast to antipsychotics of the first generation. The SGA amisulpride, however, only binds to D2/D3 receptors, which makes it an interesting tool to test this assumption. In a randomized controlled trial, 52 schizophrenic patients were allocated to treatment with either olanzapine (10–20 mg/day) or amisulpride (400–800 mg/day). A comprehensive neuropsychological test battery and clinical ratings were used to assess participants at inclusion and after 4 and 8 weeks. Cognitive improvements of moderate size were observed, with effect sizes similar to those obtained in previous studies on the cognitive effects of SGAs. Importantly, amisulpride was not inferior to olanzapine for any cognitive domain. Combined 5-HT2A/D2 receptor blockade is probably not necessary for cognitive improvement by SGAs.
Similar content being viewed by others
INTRODUCTION
The advent of novel antipsychotic medications like amisulpride, aripiprazole, clozapine, olanzapine, quetiapine, remoxipiride, risperidone, sertindole, ziprasidone, and zotepine represents an important improvement in the treatment of schizophrenia. Among the advantages of these ‘second-generation’ antipsychotics (SGAs) (also referred to as ‘atypical’ or ‘modern’ antipsychotics) over ‘first-generation’ antipsychotics (FGAs) (also referred to as ‘typical’, ‘traditional’, or ‘conventional’ antipsychotics) are reduced extrapyramidal side effect profiles (Rosenheck et al, 1997; Simpson and Lindenmayer, 1997), reduced risk for tardive dyskinesia (Chouinard, 1995; Lieberman et al, 1994), greater effects on the negative and positive symptoms (Kane et al, 1988; Marder and Meibach, 1994; Beasley et al, 1996), and possibly beneficial effects on cognitive functioning (Purdon et al, 2000; Harvey et al, 2003; Bilder et al, 2002). SGAs have diverse receptor profiles, and the mechanism of action is still controversial (Seeman, 2002). The antagonism of SGAs to serotonin-2A (5-HT2A) receptors has been invoked to explain the improved efficacy of SGAs as compared to FGAs (with which they share the dopamine (D) antagonism), because most SGAs have a greater difference between 5-HT2 and D2 affinity than FGAs (Meltzer et al, 1989; Ichikawa and Meltzer, 1999; Meltzer, 1999). This view is supported by the fact that SGAs can increase cortical dopamine by 5-HT2A blockade in the rat (Liegeois et al, 2002). Furthermore, the role of 5-HT2A receptors in modulating working memory in humans has been established (Luciana et al, 1998; Williams et al, 2002).
Since the introduction of SGAs, treatment success is not only defined by effects on positive and negative symptoms, but also by improvements in domains of cognitive functions, which are highly relevant for functional outcome (Liddle, 2000; Sharma and Mockler, 1998; Sharma and Antonova, 2003). Several studies reported improvements after switching patients from FGAs to risperidone and clozapine (Keefe et al, 1999). In early randomized controlled trials, risperidone was found to be superior to haloperidol with regard to verbal working memory (Green et al, 1997) and verbal declarative memory (Kern et al, 1999). A randomized clinical trial of Purdon et al (2000) compared cognitive effects of haloperidol with two SGAs (olanzapine and risperidone) over 12 months and found olanzapine to be superior to risperidone and haloperidol in a global cognitive measure, with few reliable treatment differences for single tests or cognitive domains. This study has been criticized for high dropout rates, which were different between treatments (Weiss et al, 2002), and for a high average dosage of risperidone (Sharma, 2002). A subsequent 14-week study by Bilder et al (2002) confirmed that 10–40 mg olanzapine was superior to 10–30 mg haloperidol (particularly with regard to attention), but also found improvements in memory, which were most marked for 4–16 mg risperidone, implicating that different SGAs may differ in their patterns of cognitive effects. However, a large study of Harvey et al (2003), comparing the cognitive effects of 5–20 mg olanzapine or 2–6 mg/day risperidone over 8 weeks in 377 patients, found no differences between both treatments, while performance of all patients improved for several domains. Similarly, in a recent 6-week head to head study, Harvey et al (2004) demonstrated identical positive effects of ziprasidone and olanzapine on many cognitive functions. In order to assess the comparative neurocognitive effectiveness of several SGAs (olanzapine, quetiapine, risperidone, ziprasidone) in large samples, the NIMH has funded the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE; Keefe et al, 2003).
The available body of data is encouraging because many commonly prescribed SGAs seem to improve cognitive functioning reliably, albeit modestly. However, from a theoretical point of view, the cognitive equivalence of SGAs evident from large trials is somewhat disappointing, because the pharmacological differences between the SGAs tested so far do not result in different cognitive effects, and therefore the mode (or the modes) of action of SGAs on cognition remains unclear: ‘Whether relatively more potent 5-HT2A receptor compared to D2 antagonism has a major or, indeed any role in the cognitive effects of these agents is not known’ (Meltzer, 2002, p 824).
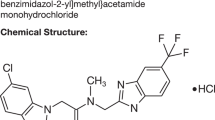
In order to test critically the supposed crucial role of 5-HT2A antagonism for cognitive improvement, an examination of substances that lack this 5-HT2A mechanism but that qualify as a SGA because of their clinical profile would be most informative. Fortunately, there is a SGA, approved for the treatment of schizophrenia in Europe and Canada, that can be used as a tool for testing the necessity of a 5-HT2A antagonism for cognitive change. Amisulpride is a pure D2/D3 receptor antagonist. However, amisulpride has not been compared with other SGAs having a 5-HT2A antagonism with regard to cognitive functions to date.
Aside from their putative effects on cognition, SGAs have clearly stronger effects on negative symptoms than FGAs, and the combined 5-HT2A/D2 antagonism, which might explain cognitive effects of SGAs, is also been considered to explain this superiority (Meltzer, 2002). However, a meta-analysis of Leucht et al (2002) showed that amisulpride was superior to FGA or placebo in improving primary negative symptoms, casting some doubt on the ‘combined antagonism’ notion. Negative symptoms often go together with cognitive dysfunction (Berman et al, 1997; Brebion et al, 2000), and negative symptom scales contain several items for the clinical assessment of cognition, like attention, abstraction, and insight. If the combined 5-HT2A/D2 antagonism is not necessary for the improvement of negative symptoms, as the meta-analysis of Leucht et al (2002) suggests, it may also not be relevant for the improvement of cognitive deficits.
In summary, recent data from well-designed studies show that several SGAs all sharing a serotonergic component improve cognitive functioning in schizophrenic patients. One prominent theory, mainly supported by animal data, proposes that SGAs increase cortical dopamine partly because of their ability to block potently serotonin 5-HT2A receptors (Liegeois et al, 2002; Meltzer and Sumiyoshi, 2003).
The present study was designed to compare directly two pharmacologically very distinct antipsychotic drugs, olanzapine and amisulpride, with regard to negative symptoms and cognitive deficits, and to test whether different mechanisms of action might underlie similar clinical efficacy. Thus, we tested the hypothesis that serotonergic action is the common and necessary mode of action of all antipsychotic medications with beneficial effects on negative symptoms and cognition.
METHODS
Participants
Patients admitted to the Psychiatric Hospital of the University of Bonn for in-patient treatment were considered eligible for the study if the following criteria were met: a diagnosis of schizophrenia according to DSM IV and ICD 10, age 18–65, Clinical Global Impressions (CGI)=4 or more, Positive and Negative Symptom Scale (PANSS)=61 or more, and no clozapine treatment within 3 months prior to inclusion. Furthermore, subjects were excluded if they had any history of CNS trauma, epilepsy, meningoencephalitis; instable somatic condition; substance dependency; lack of sufficient contraception in premenopausal females; history of antipsychotic drug resistance; and risk of suicide or aggressive behavior.
A total of 52 patients meeting these criteria were randomly allocated to treatment with either olanzapine (10–20 mg) or amisulpride (400–800 mg). Randomization was performed by distributing the study medications to containers according to a pseudo-random computer algorithm.
Prior to inclusion, 12 patients (eight in the amisulpride group, four in the olanzapine group) were treated with FGAs and three (all in the olanzapine group) with SGAs (two risperidone, one quetiapine). A total of 21 patients were antipsychotically untreated at least for 4 weeks prior to inclusion. Prior to inclusion, two patients (one amisulpride, one olanzapine) were treated with selective serotonin reuptake inhibitors (SSRIs) citalopram or sertraline, which was stopped 2 days prior to inclusion. Previous oral psychotropic medication was stopped 2 days prior to inclusion and treatment with depot antipsychotics was stopped at least two biological half-lifes prior to inclusion.
The study was approved by the institutional review board of the University of Bonn Medical School. All participants gave written informed consent before inclusion.
Treatments
After a wash-out phase of 2 days, in which only lorazepam up to 4 mg daily was permitted, participants received, according to randomization, a half-flexible dose range of 10–20 mg olanzapine or 400–800 mg amisulpride. Psychiatrists and patients were blinded to treatment group and prescribed levels of medication, starting with either 10 mg olanzapine or 400 mg amisulpride at day 1. According to clinical response, the dosage was adjusted within the first 3 days in the range defined above. The following other pharmacological treatments only were permitted: (1) up to 4 mg lorazepam per day for treatment of agitation, (2) adjunct treatment with zopiclone up to 22.5 mg daily, and (3) up to 4 mg of biperiden for treatment of extrapyramidal motor symptoms (EPMS). However, lorazepam, zopiclone, and biperiden were tapered 24 h before each neuropsychological testing.
Clinical Assessment
Blind raters performed all clinical symptom ratings with PANSS (Kay et al, 1992), Scale for the Assessment of Negative Symptoms (SANS; Andreasen, 1983), Simpson–Angus Scale (SAS; Simpson and Angus, 1979), and CGI (Guy, 1976) at inclusion (week 0) and after 1, 4, and 8 weeks.
Neurocognitive Assessment
The cognitive assessment was designed to cover a range of reliable and validated tests frequently used in similar studies. We attempted to balance the interest for a broad assessment of important cognitive domains with load on patients in order to reduce the possibility of attrition. The battery took about 90–120 min including breaks as needed, and was generally well tolerated by patients. The tests were grouped into four cognitive domains (attention, executive functions, working memory, and verbal learning and memory) according to a priori considerations. In addition, a global cognitive index was constructed by summing and averaging across the z-scored variables of neurocognitive tests.
The test battery was administered three times, the first time within the first week after randomization and start of treatment with olanzapine or amisulpride, the second time after 4 weeks, and the last time after 8 weeks (at the end of treatment). Since patients were acutely ill and required in-patient treatment, an assessment prior to antipsychotic medication was not performed, in order to establish cooperation of patients and thus to ensure reliable test performance.
Attention
We used the trail-making test A (TMT-A) to assess visomotor speed (Reitan and Wolfson, 1993). The dependent variable was the time required to complete the test. To assess vigilance, we used the identical pairs version of the continuous performance test (CPT-IP) (Cornblatt et al, 1988). The signal detection index d-prime and the reaction time to hits were the dependent variables.
Executive functions
The second part of the trail-making test (TMT-B) evaluated both visomotor speed and the ability to alternate between sets. The dependent variable was the time required to complete the test. To assess global verbal fluency, we administered three fluency tests: category and letter fluency (Spreen and Strauss, 1998) as well as action (verb naming) fluency (Piatt et al, 1999). The respective fluency scores were summed to a global fluency score, which was the dependent variable. We also administered the maze test to assess problem solving and higher cognitive functioning (Chapuis, 1959). The time required to complete the test and the sum of errors were the dependent variables.
Working memory
The letter-number sequencing task was used to measure verbal working memory (Wechsler, 1997). The sum of correct trials was the dependent variable. The first trial of the German version of the Rey auditory verbal learning test was also used as a measure for verbal working memory (Helmstaedter et al, 2001). The number of correct words was the dependent variable. To evaluate spatial working memory, we used the one-point test, delayed recall (Keefe et al, 1995). The dependent variable was the mean deviation from the shown points in millimeters. A further measure of visual working memory was assessed with the nonverbal part of the self-ordered pointing task (SOPT; Petrides and Milner, 1982). The sum of errors was the dependent variable.
Verbal learning and memory
To assess verbal declarative memory function, we administered the Rey auditory verbal learning test. The sum of words of trials 2–5, the delayed recall trial, and the recognition score p(A) (Forrester and Geffen, 1991) were the dependent variables. In addition, we assessed story recall with the logical memory task of the German version of the Rivermead behavioural memory test (Wilson et al, 1992). The number of recalled cues was the dependent variable.
With the exception of CPT-IP, the one-point test, and SOPT, we used three different parallel versions of the neurocognitive tests at the three test sessions.
Data Analysis
Before analysis of clinical and neuropsychological data, we examined demographic variables and severity of illness as well as test performance at inclusion in the patients who completed neuropsychological testing at least at week 4 compared with those who did not. All clinical and neurocognitive variables were analyzed by t-tests to determine whether baseline differences existed between treatment groups.
A total of 17 variables were extracted from the neuropsychological tests for each test session. The neuropsychological data of the patients were standardized with reference to the mean and standard deviation of the entire sample. Signs were adjusted so that negative values reflect impairment. The common z-metric also allows for an integration of single variables into cognitive domains and into a global cognitive index, which was used as a primary measure for confirmatory testing. We used the last observation carried forward (LOCF) method; thus, measures of patients who dropped out after week 4 were carried on with their last clinical and neuropsychological scores to week 8.
Negative symptoms and cognitive functioning constituted the main outcomes. Analysis of treatment effects in clinical scales used the general linear models approach to repeated measures analysis of variance (SPSS Inc., Chicago, Illinois) with week 0, 1, 4, and 8 (end point) scores as dependent variables, time as a within-subject repeated measure (four-fold), and treatment group (amisulpride, olanzapine) as a between-subjects fixed factor (two-fold). Analysis of treatment effects in each cognitive domain and the global index used the general linear models approach to repeated measures analysis of variance with week 1, 4, and 8 (end point) scores as dependent variables, time as a within-subject repeated measure (three-fold), and treatment group (amisulpride, olanzapine) as a between-subjects fixed factor (two-fold). Frequency data (gender, dropout rates) were analyzed by χ2 tests. Inter-relations between cognitive and clinical improvement were tested by Pearson's product-moment correlation. The confirmatory statistical comparisons of all data were carried out at a significance level set at P=0.05 (two-tailed).
Individual test scores were not analyzed separately, since with 17 tests we felt the analysis would suffer either from capitalization on chance (given the number of tests) or from overly conservative alpha levels that would be needed to correct for test multiplicity.
RESULTS
Demographic Data
Groups of patients randomized to receive either treatment did not differ with regard to proportion of male and female subjects, age, age of illness onset, number of previous episodes, years of education, or number of weeks in study. This was true for the full sample (N=26 in each treatment group) as well as for the sample with neuropsychological data at least for weeks 1 and 4 (N=18 in each treatment group) (Table 1 ).
Dropouts
A total of 52 patients were randomized. Two patients withdrew informed consent in the first week (amisulpride/olanzapine: 1/1). In all, 13 patients dropped out between weeks 1 and 4: two because of noncompliance (1/1), three were lost to follow-up (2/1), three were lost because of a lack of treatment efficacy (1/2), one turned out as slightly mentally retarded in the first neuropsychological test session (0/1), and four showed adverse events (amisulpride: one exanthema and one EPMS; olanzapine: one sedation and one increase of transaminases). A total of 10 patients dropped out between weeks 4 and 8: four were noncompliant (2/2), three were lost to follow-up (1/2), two showed adverse events (amisulpride: one galactorrhea; olanzapine: one sedation), and one was lost because of a lack of treatment efficacy (1/0). One further patient could not complete the neuropsychological assessment at weeks 4 and 8 and was therefore excluded from data analysis. Dropout rates in both treatment groups did not differ in χ2 tests. Patients who completed the study (at least until week 4) and patients who dropped out before week 4 did not differ at inclusion in psychopathology and cognition measures.
Psychopathology
At inclusion, both treatment groups did not differ significantly in any psychopathological scale. Analysis of variance (time × group, with repeated measures at factor time (four-fold, CGI item 2 three-fold)) showed a significant main effect of factor time in all scales and subscales, reflecting strong improvement of psychiatric symptoms (PANSS total: F(3/102)=80.9, P<0.001; SANS total: F(3/102)=24.8, P<0.001; CGI item 1: F(3/102)=70.4, P<0.001). No significant interactions of factor time and group occurred, but there were two trends of interaction in the PANSS general scale (F(3/102)=2.4, P=0.08) and SANS Affective Flattening scale (F(3/102)=2.0, P=0.12). The amisulpride group tended to show a stronger reduction of symptoms in these scales. Analysis of variance (with repeated measures at factor time) within each group showed a significant decrease of psychiatric symptoms in all scales and subscales in both groups with the exception of the SANS Affective Flattening scale where the improvement was not significant in the olanzapine group. Figures 1 and 2 show the development of psychiatric symptoms in PANSS and SANS across treatment period. The mean (±standard deviation) CGI item 1 (severity) scores (amisulpride/olanzapine) were for inclusion 6.1±0.7/6.2±0.4, for week 1 5.3±0.8/5.4±1.1, for week 4 3.9±1.0/4.4±0.9, and for the end point 3.7±1.0/4.3±1.1. The CGI item 2 (change) scores were for week 1 3.6±0.6/4.0±1.1, for week 4 3.1±1.0/3.3±0.8, and for the end point 2.7±1.1/3.1±1.0.
Neurological Symptoms
At inclusion, both treatment groups did not differ with regard to EPMS (measured with SAS). Analysis of variance (time × group, with repeated measures at factor time (four-fold)) showed no significant main or interaction effects. At the end of study, the amisulpride group showed slightly more EPMS, but this difference was not statistically significant (Figure 3).
Cognition
At inclusion (week 1), the treatment groups did not differ significantly in the global cognition index, which summarizes the performance of all neuropsychological tests. Analysis of variance (time × group, with repeated measures at factor time (three-fold)) showed a significant main effect of factor time (F(2/68)=10.0, P<0.001), but no significant interaction of both factors. Thus, both groups showed comparable and significant improvement of global cognitive functioning (see Table 2 ).
For cognitive domains (attention, executive functions, working memory, and declarative memory), the pattern was similar: at week 1, both groups did not differ significantly in any domain. Analyses of variance (time × group, with repeated measures at factor time (three-fold)) showed a significant main effect of factor time in executive functions (F(2/68)=4.9, P<0.01), working memory (F(2/68)=14.0, P<0.001), and declarative memory (F(2/68)=4.6, P<0.05), but not in attention (F(2/68)=1.4, P=0.25). No significant interactions of both factors occurred, but in attention there was a weak trend (F(2/68)=2.1, P=0.13) for an interaction of factors group and time, reflecting a stronger increase of attention performance in the amisulpride group. Otherwise, both groups showed comparable and significant improvement of executive functions, working memory, and declarative memory.
Analyses of variance (with repeated measures at factor time (three-fold)) within each treatment group showed a more differentiated pattern: the amisulpride group showed a significant main effect of factor time in the domains attention (F(2/34)=5.1, P<0.01), executive functions (F(2/34)=7.8, P<0.01), and working memory (F(2/34)=5.0, P<0.01), as well as in the global cognitive index (F(2/34)=13.4, P<0.001). The domain declarative memory showed a trend for a main effect in this factor (F(2/34)=2.7, P=0.08). The olanzapine group showed a significant main effect of factor time only in the domain working memory (F(2/34)=9.3, P<0.001), and trends for a main effect in this factor for declarative memory (F(2/34)=2.0, P=0.15) as well as for the global cognitive index (F(2/34)=2.5, P=0.10). Since overall ANOVA (including both treatment groups) did not result in a significant group × time interaction, these results from the within-group analyses have to be interpreted with caution, but they might indicate that amisulpride had a broader range of cognitive effects.
In order to compare the effect sizes of this study with those of other studies, effect sizes for improvement were calculated for patients by dividing the amount of improvement (z-score at end point (LOCF) minus z-core at week 1) by the standard deviation of all patients at week 0. This was carried out for each cognitive domain and for the global cognitive index. The effect sizes were 0.30 for the global cognitive index (amisulpride/olanzapine: 0.40/0.20), 0.25 for attention (0.57/−0.05), 0.30 for executive functions (0.42/0.18), 0.34 for working memory (0.28/0.39), and 0.14 for declarative memory (0.19/0.08).
Relationship of Cognitive Improvements to Change of Negative and Positive Symptoms
To examine which cognitive improvements were accompanied by symptomatic change, correlations between change scores of the cognitive domain measures and the reduction of negative and positive symptoms were calculated. Improvement of the PANSS positive subscale was neither correlated with improvement of the global cognitive index nor with improvements of any cognitive domain. In contrast, the improvement of the PANSS negative subscale (r=−0.40, P<0.05) and of the SANS total score (r=−0.47, P<0.01) showed moderate but significant associations with improvements of the global cognitive index. Furthermore, improvement of the global cognitive index was significantly correlated with improvement of the PANSS general subscale (r=−0.37, P<0.05), SANS Affective Flattening (r=−0.45, P<0.01), SANS Apathy (r=−0.49, P<0.01), SANS Anhedonia (r=−0.49, P<0.01), PANSS total score (r=−0.38, P<0.05), CGI-Severity (r=−0.51, P<0.01), and SAS (r=−0.40, P<0.05). Improvement of attention was significantly correlated with improvement of CGI-Severity (r=−0.39, P<0.05), SANS total (r=−0.38, P<0.05), and SANS Affective Flattening (r=−0.49, P<0.01). Improvement of executive functions was significantly correlated with improvement of SANS Apathy (r=−0.35, P<0.05). Improvement of working memory was significantly correlated with improvement of CGI-Severity (r=−0.48, P<0.01), SANS Apathy (r=−0.38, P<0.05), and SANS Anhedonia (r=−0.36, P<0.05). Improvement of declarative memory was significantly correlated with improvement of SAS (r=−0.37, P<0.05).
DISCUSSION
Both olanzapine and amisulpride proved to be well effective in alleviating both negative and positive symptoms, with no indication of differential effects in any of the rating scales. The consideration of the mean scores (regardless of statistical significance) gives no indication of superior efficacy of olanzapine. The equivalence of olanzapine and amisulpride with regard to positive and negative symptoms has also been demonstrated in another randomized comparison study with 377 acutely psychotic schizophrenic patients, where 2 months after treatment onset no differences in BPRS total or BPRS factor scores, or depressive symptoms (Martin et al, 2002) were evident. A meta-analysis by Davis et al (2003) indicated that olanzapine and amisulpride are both equally superior to conventional antipsychotics regarding PANSS or BPRS total scores (effect sizes, olanzapine, d=0.21, amisulpride, d=0.29). The effectiveness of amisulpride on negative symptoms was also confirmed by a meta-analysis of Leucht et al (2002). In line with much other evidence, the present study suggests that olanzapine and amisulpride exert highly similar effects on positive as well as negative symptoms, despite the fact that amisulpride lacks the 5-HT2A component. This is difficult to reconcile with the hypothesis that a serotonergic action is necessary to improve negative symptoms in schizophrenic patients (Meltzer et al, 1989; Ichikawa and Meltzer, 1999; Meltzer, 1999).
The present study is the first one directly comparing the cognitive benefits of olanzapine and amisulpride. In both treatment groups, statistically significant improvements occurred during treatment, which were comparable in effect size to the improvements noted in other studies (Harvey and Keefe, 2001). However, neither for the primary outcome measure (global cognitive index) nor for any of the four cognitive domain measures, a significant difference between both antipsychotics could be demonstrated. Exploratory data analysis for single tests revealed possibly stronger effects for olanzapine on working memory, and possibly stronger effects of amisulpride on attention and executive functioning. These effects may deserve further examination in future studies.
One limitation of the present study is its limited power to detect superiority. Since the effect size in favor of SGAs is usually about 0.2–0.5 standard deviations, very large sample sizes would be needed in order to detect differences, and even larger sample sizes are required to rule them out. But the fact that there was even a trend for a superiority of amisulpride for cognition makes an undetected superiority of olanzapine highly unlikely. Based on the effect sizes observed (0.4 for amisulpride, 0.2 for olanzapine, for the global cognitive index), one might rather anticipate that a study with high statistical power could demonstrate superiority of amisulpride.
Another issue is the number of dropouts. Of 52 subjects randomized, 15 dropped out of the study before week 4. The number of subjects lost to follow-up is not uncommon for such studies (Martin et al, 2002; Meyer-Lindenberg et al, 1997; Purdon et al, 2001; Volavka et al, 2002; Santarlasci and Messori, 2003) and there was no indication of selective attrition in one group, which might have biased the results.
The follow-up interval for the study has been 8 weeks, with several patients dropping out of the study after 4 weeks. Thus, stronger cognitive effects of one substance over the other one might have emerged after long-term treatment, but such a delay would have little pharmacological plausibility, and many previous studies have observed improvements within the first weeks of olanzapine treatment (Harvey et al, 2003).
In this study, the first neuropsychological assessment took place after subjects were already medicated for 0–8 days (mean±SD 4.8±2.2, median 5 days). We opted for this schedule in order to ensure sufficient attention and motivation to comply with the testing protocol. Subjects in both treatment groups did not differ from each other with regard to psychopathology or cognition at the first testing, and possible differences between groups therefore would not have been affected by this testing schedule. This procedure might underestimate the absolute benefit of either treatment, since some early cognitive improvements would go undetected. However, this shortcoming is irrelevant for the hypothesis under investigation.
The effect sizes of cognitive improvement in the present study are very similar to those summarized by Harvey and Keefe (2001) for studies of SGAs. Harvey and Keefe (2001, Table 4) reported effect sizes between 0.13 (for immediate memory) and 0.43 (for verbal fluency), for studies of 4–8 weeks duration where the amount of improvement was most often determined by switching patients from older antipsychotics to newer ones (the rather small change of declarative memory found in the present study is probably caused in part by a more difficult version of the auditory verbal learning test used at the third testing). Thus, the present trial achieved small to moderately sized cognitive improvements across 8 weeks (0.14–0.34 for the entire sample), equivalent to other studies with SGAs. It is therefore highly unlikely that the failure to find differential effects of olanzapine and amisulpride is the result of methodological limitations that would have precluded to identify such effects.
Amelioration of cognitive deficits was correlated with reduced negative but not with reduced positive symptoms across the duration of the trial. The independence of cognitive deficits from positive symptoms has been shown in previous studies (Breier et al, 1991; Green, 1996; Hughes et al, 2003). The improvement in negative symptoms and in cognitive deficits may partly be mediated by common underlying mechanisms, presumably dopaminergic, that are pharmacologically influenced by both atypical drugs studied here.
Olanzapine and amisulpride both exerted moderately sized positive effects on several aspects of cognition, and this is probably more than a trivial test repetition or training effect. It should be noted, though, that studies on cognitive effects of antipsychotics so far never assessed whether the treatment really narrows the gap between normal performance and the performance of patients, simply because a normal control group has not been studied with the same tests repeatedly. This issue requires further scrutiny. However, SGAs may allow for improvements to take place (due to practice or due to effects beyond practice), while FGAs may preclude such improvements at traditional dosage levels (eg by impairing cognitive and motor learning in the basal ganglia) or may even impede performance (by slowing motor functioning or by requiring anticholinergic medication to control EPMS) (CWGoCTE, 1998; Kasper and Resinger, 2003; Carpenter and Gold, 2002). Interestingly, low-dose haloperidol (5 mg average daily dose) was found to result in similar cognitive improvements in schizophrenic patients as risperidone (6 mg average daily dose) over 2 years (Green et al, 2002), implying that even FGAs may have neurocognitive benefits at lower than traditional doses.
Our data suggest that 5-HT2A blockade is not the common denominator of SGAs beneficial effects on cognition. The same is true for their clinical efficacy with regard to negative and positive symptoms.
This study cannot be taken as evidence against a common mechanism behind SGAs, the identification of which would possibly facilitate future drug development. One alternative hypothesis focuses on faster dissociation of all SGAs from the D2 receptor (Kapur and Seeman, 2001), and this would be a common mechanism for amisulpride and olanzapine (and other SGAs). Data reported in Seeman (2002) show that amisulpride dissociates as fast as clozapine from D2 receptors. The comparable clinical effectiveness of amisulpride with serotonergic SGAs has been interpreted by Lewis (2002) as indirect evidence for the fast dissociation hypothesis of Kapur and Seeman (2001). By the same token, the present data on equal cognitive effectiveness would also constitute indirect evidence for this fast dissociation hypothesis. At any rate, they provide direct evidence against a crucial role of 5-HT2A antagonism for obtaining cognitive effects in schizophrenia.
Serotonin receptors may still play a role for future drug developments. For example, 5-HT1A agonism increases dopaminergic and cholinergic neurotransmission in the cortex, and may therefore be a mechanism to improve cognition (Ichikawa and Meltzer, 1999; Meltzer, 1999). In fact, a clinical pilot study by Sumiyoshi et al (2001) found that the selective 5-HT1A agonist tandospirone, given as an add-on therapy, improved executive function and verbal memory in schizophrenic patients treated with conventional antipsychotics, while placebo did not. Similarly, 5-HT2A blockade with mianserin as an add-on improved some aspects of memory (but not executive functions) in schizophrenics treated with FGAs (Poyurovsky et al, 2003).
These findings are theoretically important for a better understanding of neurobiological mechanisms underlying the efficacy of SGAs. While animal data are valuable to derive hypotheses for a better understanding of drug actions in patients, these hypotheses have to be tested clinically. Cognitive impairments in schizophrenia continue to pose a burden on patients and caregivers, despite the modest improvements brought about by the SGAs. Only hypotheses confirmed by clinical data can guide the rational search for better drug treatments in the future.
References
Andreasen NC (1983). The Scale for Assessment of Negative Symptoms (SANS). The University of Iowa: Iowa City.
Beasley Jr CM, Tollefson G, Tran P, Satterlee W, Sanger T, Hamilton S (1996). Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial. Neuropsychopharmacology 14: 111–123.
Berman I, Viegner B, Merson A, Allan E, Pappas D, Green AI (1997). Differential relationships between positive and negative symptoms and neuropsychological deficits in schizophrenia. Schizophr Res 25: 1–10.
Bilder RM, Goldman RS, Volavka J, Czobor P, Hoptman M, Sheitman B et al (2002). Neurocognitive effects of clozapine, olanzapine, risperidone, and haloperidol in patients with chronic schizophrenia or schizoaffective disorder. Am J Psychiatry 159: 1018–1028.
Brebion G, Amador X, Smith M, Malaspina D, Sharif Z, Gorman JM (2000). Depression, psychomotor retardation, negative symptoms, and memory in schizophrenia. Neuropsychiatry Neuropsychol Behav Neurol 13: 177–183.
Breier A, Schreiber JL, Dyer J, Pickar D (1991). National Institute of Mental Health longitudinal study of chronic schizophrenia. Prognosis and predictors of outcome. Arch Gen Psychiatry 48: 239–246.
Carpenter WT, Gold JM (2002). Another view of therapy for cognition in schizophrenia. Biol Psychiatry 51: 969–971.
Chapuis F (1959). Der Labyrinth-Test. Verlag Hans Huber: Bern.
Chouinard G (1995). Effects of risperidone in tardive dyskinesia: an analysis of the Canadian multicenter risperidone study. J Clin Psychopharmacol 15: 36–44.
Cornblatt BA, Risch NJ, Faris G, Friedman D, Erlenmeyer-Kimling L (1988). The Continuous Performance Test, identical pairs version (CPT-IP): I. New findings about sustained attention in normal families. Psychiatry Res 26: 223–238.
CWGoCTE (Collaborative Working Group on Clinical Trial Evaluations (1998). Evaluating the effects of antipsychotics on cognition in schizophrenia. J Clin Psychiatry 59: 35–40.
Davis JM, Chen N, Glick ID (2003). A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 60: 553–564.
Forrester G, Geffen G (1991). Performance measures of 7- to 15-year-old children on the Auditory Verbal Learning Test. Clin Neuropsychol 5: 345–359.
Green MF (1996). What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153: 321–330.
Green MF, Marder SR, Glynn SM, McGurk SR, Wirshing WC, Wirshing DA et al (2002). The neurocognitive effects of low-dose haloperidol: a two-year comparison with risperidone. Biol Psychiatry 51: 972–978.
Green MF, Marshall Jr BD, Wirshing WC, Ames D, Marder SR, McGurk S et al (1997). Does risperidone improve verbal working memory in treatment-resistant schizophrenia? Am J Psychiatry 154: 799–804.
Guy W (1976). 028 CGI. Clinical global impressions. In: ECDEU Assessment Manual for Psychopharmacology, revised edition. National Institute of Mental Health (NIMH): Rockville, MD.
Harvey PD, Green MF, McGurk SR, Meltzer HY (2003). Changes in cognitive functioning with risperidone and olanzapine treatment: a large-scale, double-blind, randomized study. Psychopharmacology 169: 404–411.
Harvey PD, Keefe RS (2001). Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am J Psychiatry 158: 176–184.
Harvey PD, Siu CO, Romano S (2004). Randomized, controlled, double-blind, multicenter comparison of the cognitive effects of ziprasidone versus olanzapine in acutely ill inpatients with schizophrenia or schizoaffective disorder. Psychopharmacology 172: 324–332.
Helmstaedter C, Lendt M, Lux S (2001). Verbaler Lern- und Merkfähigkeitstest. Beltz: Göttingen.
Hughes C, Kumari V, Soni W, Das M, Binneman B, Drozd S et al (2003). Longitudinal study of symptoms and cognitive function in chronic schizophrenia. Schizophr Res 59: 137–146.
Ichikawa J, Meltzer HY (1999). Relationship between dopaminergic and serotonergic neuronal activity in the frontal cortex and the action of typical and atypical antipsychotic drugs. Eur Arch Psychiatry Clin Neurosci 249: 90–98.
Kane J, Honigfeld G, Singer J, Meltzer H (1988). Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45: 789–796.
Kapur S, Seeman P (2001). Does fast dissociation from the dopamine D2 receptor explain the action of atypical antipsychotics?: A new hypothesis. Am J Psychiatry 158: 360–369.
Kasper S, Resinger E (2003). Cognitive effects and antipsychotic treatment. Psychoneuroendocrinology 28: 27–38.
Kay SR, Opler LA, Fiszbein A (1992). Positive and Negative Syndrome Scale (PANSS). Manual. Multi-health Systems Inc.: North Tonawanda, NY.
Keefe RS, Mohs RC, Bilder RM, Harvey PD, Green MF, Meltzer HY et al (2003). Neurocognitive assessment in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project schizophrenia trial: development, methodology, and rationale. Schizophr Bull 29: 45–55.
Keefe RS, Roitman SE, Harvey PD, Blum CS, DuPre RL, Prieto DM et al (1995). A pen-and-paper human analogue of a monkey prefrontal cortex activation task: spatial working memory in patients with schizophrenia. Schizophr Res 17: 25–33.
Keefe RS, Silva SG, Perkins DO, Lieberman JA (1999). The effects of atypical antipsychotic drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophr Bull 25: 201–222.
Kern RS, Green MF, Marshall Jr BD, Wirshing WC, Wirshing D, McGurk SR et al (1999). Risperidone versus haloperidol on secondary memory: can newer medications aid learning? Schizophr Bull 25: 223–232.
Leucht S, Pitschel-Walz G, Engel RR, Kissling W (2002). Amisulpride, an unusual ‘atypical’ antipsychotic: a meta-analysis of randomized controlled trials. Am J Psychiatry 159: 180–190.
Lewis DA (2002). Atypical antipsychotic medications and the treatment of schizophrenia. Am J Psychiatry 159: 177–179.
Liddle PF (2000). Cognitive impairment in schizophrenia: its impact on social functioning. Acta Psychiatr Scand Suppl 400: 11–16.
Lieberman JA, Safferman AZ, Pollack S, Szymanski S, Johns C, Howard A et al (1994). Clinical effects of clozapine in chronic schizophrenia: response to treatment and predictors of outcome. Am J Psychiatry 151: 1744–1752.
Liegeois JF, Ichikawa J, Meltzer HY (2002). 5-HT(2A) receptor antagonism potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and inhibits that in the nucleus accumbens in a dose-dependent manner. Brain Res 947: 157–165.
Luciana M, Collins PF, Depue RA (1998). Opposing roles for dopamine and serotonin in the modulation of human spatial working memory functions. Cereb Cortex 8: 218–226.
Marder SR, Meibach RC (1994). Risperidone in the treatment of schizophrenia. Am J Psychiatry 151: 825–835.
Martin S, Ljo H, Peuskens J, Thirumalai S, Giudicelli A, Fleurot O et al (2002). A double-blind, randomised comparative trial of amisulpride versus olanzapine in the treatment of schizophrenia: short-term results at two months. Curr Med Res Opin 18: 355–362.
Meltzer HY (1999). The role of serotonin in antipsychotic drug action. Neuropsychopharmacology 21: 106–115.
Meltzer HY (2002). Mechanism of action of atypical antipsychotic drugs. In: Davis KL, Charney D, Coyle JT, Nemeroff C (eds). Neuropsychopharmacology: The Fifth Generation of Progress. Lippincott Williams & Wilkins: Philadelphia.
Meltzer HY, Bastani B, Ramirez L, Matsubara S (1989). Clozapine: new research on efficacy and mechanism of action. Eur Arch Psychiatry Neurol Sci 238: 332–339.
Meltzer HY, Sumiyoshi T (2003). Atypical antipsychotic drugs improve cognition in schizophrenia. Biol Psychiatry 53: 265–267.
Meyer-Lindenberg A, Gruppe H, Bauer U, Lis S, Krieger S, Gallhofer B (1997). Improvement of cognitive function in schizophrenic patients receiving clozapine or zotepine: results from a double-blind study. Pharmacopsychiatry 30: 35–42.
Petrides M, Milner B (1982). Deficits on subject-ordered tasks after frontal- and temporal-lobe lesions in man. Neuropsychologia 20: 249–262.
Piatt AL, Fields JA, Paolo AM, Troster AI (1999). Action (verb naming) fluency as an executive function measure: convergent and divergent evidence of validity. Neuropsychologia 37: 1499–1503.
Poyurovsky M, Koren D, Gonopolsky I, Schneidman M, Fuchs C, Weizman A et al (2003). Effect of the 5-HT2 antagonist mianserin on cognitive dysfunction in chronic schizophrenia patients: an add-on, double-blind placebo-controlled study. Eur Neuropsychopharmacol 13: 123–128.
Purdon SE, Jones BD, Stip E, Labelle A, Addington D, David SR et al (2000). Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. The Canadian Collaborative Group for research in schizophrenia. Arch Gen Psychiatry 57: 249–258.
Purdon SE, Malla A, Labelle A, Lit W (2001). Neuropsychological change in patients with schizophrenia after treatment with quetiapine or haloperidol. J Psychiatry Neurosci 26: 137–149.
Reitan RM, Wolfson D (1993). The Halstead–Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation, 2nd edn. Neuropsychology Press: Tucson.
Rosenheck R, Cramer J, Xu W, Thomas J, Henderson W, Frisman L et al (1997). A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. N Engl J Med 337: 809–815.
Santarlasci B, Messori A (2003). Clinical trial response and dropout rates with olanzapine versus risperidone. Ann Pharmacother 37: 556–563.
Seeman P (2002). Atypical antipsychotics: mechanism of action. Can J Psychiatry 47: 27–38.
Sharma T (2002). Atypical antipsychotics and cognition in schizophrenia. Arch Gen Psychiatry 59: 571–572.
Sharma T, Antonova L (2003). Cognitive function in schizophrenia. Deficits, functional consequences, and future treatment. Psychiatr Clin N Am 26: 25–40.
Sharma T, Mockler D (1998). The cognitive efficacy of atypical antipsychotics in schizophrenia. J Clin Psychopharmacol 18: 12–19.
Simpson G, Angus JA (1979). A rating scale for extrapyramidal side effects. Acta Psychiatr Scand 70: 11–19.
Simpson GM, Lindenmayer JP (1997). Extrapyramidal symptoms in patients treated with risperidone. J Clin Psychopharmacol 17: 194–201.
Spreen O, Strauss E (1998). A Compendium of Neuropsychological Tests, 2nd edn. Oxford University Press: New York.
Sumiyoshi T, Matsui M, Nohara S, Yamashita I, Kurachi M, Sumiyoshi C et al (2001). Enhancement of cognitive performance in schizophrenia by addition of tandospirone to neuroleptic treatment. Am J Psychiatry 158: 1722–1725.
Volavka J, Czobor P, Sheitman B, Lindenmayer JP, Citrome L, McEvoy JP et al (2002). Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry 159: 255–262.
Wechsler DA (1997). WAIS-III, WMS-III Technical Manual. Psychological Cooperation: San Antonio, TX.
Weiss EM, Bilder RM, Fleischhacker WW (2002). The effects of second-generation antipsychotics on cognitive functioning and psychosocial outcome in schizophrenia. Psychopharmacology 162: 11–17.
Williams GV, Rao SG, Goldman-Rakic PS (2002). The physiological role of 5-HT2A receptors in working memory. J Neurosci 22: 2843–2854.
Wilson B, Cockburn J, Baddeley A (1992). Der Rivermead Behavioural Memory Test, Manual. Thames Valley Test Company: Bury St Edmunds.
Acknowledgements
Eli Lilly and Company contributed supplemental funding. Experimental design, data acquisition, statistical analyses, and interpretation of the results were carried out without input from any pharmaceutical company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wagner, M., Quednow, B., Westheide, J. et al. Cognitive Improvement in Schizophrenic Patients does not Require a Serotonergic Mechanism: Randomized Controlled Trial of Olanzapine vs Amisulpride. Neuropsychopharmacol 30, 381–390 (2005). https://doi.org/10.1038/sj.npp.1300626
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300626
Keywords
This article is cited by
-
Comparative efficacy and safety between amisulpride and olanzapine in schizophrenia treatment and a cost analysis in China: a systematic review, meta-analysis, and cost-minimization analysis
BMC Psychiatry (2018)
-
Kognitive Störungen bei schizophrenen Patienten
Der Nervenarzt (2010)
-
Behandlung kognitiver Defizite bei Schizophrenie
Der Nervenarzt (2010)
-
Associations of SNAP-25 polymorphisms with cognitive dysfunctions in Caucasian patients with schizophrenia during a brief trail of treatment with atypical antipsychotics
European Archives of Psychiatry and Clinical Neuroscience (2008)
-
Efficacy of olanzapine versus quetiapine on cognitive dysfunctions in patients with an acute episode of schizophrenia
European Archives of Psychiatry and Clinical Neuroscience (2007)