Abstract
Fluoxetine, a selective serotonin (5-hydroxytryptamine, 5-HT) reuptake inhibitor, is used widely to treat depression and related disorders. By inhibiting presynaptic 5-HT reuptake, fluoxetine is thought to act by increasing 5-HT in the synaptic cleft, thus 5-HT binding to postsynaptic 5-HT2A/2C receptors. These receptors can be coupled via a G-protein to phospholipase A2 (PLA2), which when activated releases the second messenger arachidonic acid from synaptic membrane phospholipids. To image this activation, fluoxetine (10 mg/kg) or saline vehicle was administered i.p. to unanesthetized rats, and regional brain incorporation coefficients k* of intravenously injected radiolabeled arachidonic acid were measured after 30 min. Compared with vehicle, fluoxetine significantly increased k* in prefrontal, motor, somatosensory, and olfactory cortex, as well as in the basal ganglia, hippocampus, and thalamus. Many of these regions demonstrate high densities of the serotonin reuptake transporter and of 5-HT2A/2C receptors. Brain stem, spinal cord, and cerebellum, which showed no significant response to fluoxetine, have low densities of the transporters and receptors. The results show that it is possible to image quantitatively PLA2-mediated signal transduction in vivo in response to fluoxetine.
Similar content being viewed by others
INTRODUCTION
Fluoxetine is widely used to treat depression, obsessive–compulsive disorder, panic disorder, and bulimia (Fuller, 1995). It is a selective serotonin (5-hydroxytryptamine, 5-HT) reuptake inhibitor, enhancing postsynaptic serotonergic neurotransmission by increasing the concentration of 5-HT in the synaptic cleft (Fuller and Wong, 1977; Wong et al, 1995).
Acute administration of fluoxetine to rodents elicits anxiogenic effects in social interaction and maze tests (Kurt et al, 2000; To et al, 1999), potentiates defensive reactions such as flight and biting (Griebel et al, 1995), and potentiates amphetamine-induced locomotor activity (Sills et al, 1999). Acute drug also stimulates secretion of pituitary ACTH and adrenal corticosterone (Dinan, 1996; Li et al, 1993). It triggers transcription of the gene encoding the corticotrophin-release factor and its type 1 receptor (Torres et al, 1998), thus affecting the hypothalamic–pituitary–adrenal axis that is considered hyperactive in depressed patients (Leonard, 2001).
Acute administration of fluoxetine also exerts inhibitory effects. It reduces spontaneous motor activity in 6- to 8-month-old rats, and to a lesser extent in aged rats (Stanford et al, 2002). It reduces regional cerebral metabolic rates for glucose (rCMRglc) in awake rats (Freo et al, 2000) as well as in humans (Cook et al, 1994). Similar reductions in rCMRglc in rats have been noted in response to the 5-HT2A/2C receptor agonist (±)-2,5-dimethoxy-4-iodophenyl-2-aminopropane (DOI) (Freo et al, 1991).
5-HT2A/2C receptors can be coupled via G-proteins to phospholipase A2 (PLA2) (Berg et al, 1998; Felder et al, 1990; Kim et al, 1999; Qu et al, in press), which when activated will release arachidonic acid (20:4 n-6) from the stereospecifically numbered (sn)-2 position of phospholipids (Axelrod, 1990). Both arachidonate and its eicosanoid metabolites are important second messengers (Fitzpatrick and Soberman, 2001). Much of the released arachidonate is not metabolized to eicosanoids, however, but rapidly re-esterified into synaptic membrane phospholipids, together with arachidonate derived from the plasma. The re-esterification process can be imaged in unanesthetized rats by injecting radiolabeled arachidonic acid intravenously following drug, and measuring its regional brain incorporation with quantitative autoradiography (Chang et al, 1997; DeGeorge et al, 1991; Jones et al, 1996; Rapoport, 2001; Robinson et al, 1992).
In this regard, we reported that radiolabeled arachidonate could be used to image brain PLA2 activation in rats administered the 5-HT2A/2C receptor agonist, DOI (Qu et al, 2001a,2003). Significant increases in tracer incorporation, noted in brain areas with high densities of 5-HT2A/2C receptors, could be blocked by pretreatment with the 5-HT2 antagonist mianserin. The increases were considered to follow the binding of DOI to 5-HT2A/2C receptors, and activation of the PLA2 to which these receptors are coupled.
We thought it of interest to see if fluoxetine also would increase incorporation of labeled arachidonate into the brain, as might be expected from its ability to increase 5-HT in the synaptic cleft and thus 5-HT occupancy of 5-HT2A/2C receptors (see above). To test this expectation, we decided to measure the incorporation of radiolabeled arachidonate from plasma into the brain of unanesthetized rats, 30 min after giving fluoxetine 10 mg/kg i.p. At 30–60 min, this dose increases 5-HT levels in the rat brain, and the levels remain elevated for 3 h (Guan and McBride, 1988). Additionally, after 30 min, fluoxetine at doses of 4 mg/kg and 40 mg/kg i.p., respectively, has been reported to reduce rCMRglc in 28 of 66 regions (mean global decrease was 23%) and 37 of 66 (mean global decrease was 33%) regions examined (Freo et al, 2000).
MATERIALS AND METHODS
Materials
Radiolabeled [5,6,8,9,11,12,14,15-3H]arachidonate ([3H]arachidonate) at a specific activity of 200 Ci/mmol was purchased from Moravek Biochemicals (Brea, CA). Radiochemical purity as shown by thin-layer chromatography always exceeded 96%. Fluoxetine was purchased from Sigma-Research Biochemicals International (Natick, MA). Sodium pentobarbital was purchased from Richmond Veterinary Supply (Richmond, VA).
Animals
Male Fischer-344 rats (Charles River Laboratories, Wilmington, MA), weighing 290–320 g and 12-weeks old, were housed under standard laboratory conditions with a 12 h light–12 h dark cycle, with ready access to laboratory chow and water. The experimental protocol was approved by the National Institute of Child Health and Human Development Animal Care and Use Committee, and conformed to the Guide for the Care and Use of Laboratory Animals (National Institute of Health Publication 86-23). Rats were divided into two groups, eight animals in each: (1) those administered fluoxetine, 10 mg/kg i.p. in 1 ml saline, 30 min before tracer infusion and (2) controls administered 1 ml i.p. saline 30 min before tracer infusion.
Arterial and Venous Catheterization
The in vivo fatty acid method to image brain PLA2 signaling has been described elsewhere (DeGeorge et al, 1991; Hayakawa et al, 2001; Qu et al, 2003). Briefly, rats in each of the two groups were anesthetized with halothane (1–3% v/v in O2). PE 50 polyethylene catheters (Clay Adams, Lincolnshire, IL) filled with heparinized saline (100 IU/ml) were surgically implanted into a femoral artery and vein, after which the incision site was infiltrated with a local anesthetic (lidocaine) and closed with wound clips. The rats were wrapped loosely in a fast-setting plaster cast, secured to a wooden block with the upper body free, and allowed to recover from anesthesia in a temperature-controlled and sound-dampened box for 4 h. Body temperature was kept at 36–37°C using a rectal thermometer and a feedback heating device.
Drug Administration and Tracer Infusion
After a rat was allowed to recover from anesthesia for 4 h, 125 μl arterial blood was withdrawn to measure pH, pO2, and pCO2. At 30 min after the administration of i.p. saline or fluoxetine (see above), 1.75 mCi/kg [3H]arachidonate in 2 ml of 5 mM HEPES buffer, pH 7.4, containing 50 mg/ml fatty acid-free bovine serum, was infused through the venous canula with an infusion pump (Harvard Instruments, Holliston, MA), at a rate of 400 μl/min for 5 min. Timed 125-μl arterial blood samples were collected from the beginning of infusion to 20 min, when the rats were killed with 65 mg i.v. sodium pentobarbital. The brain was immediately removed and frozen in 2-methylbutane at −70°C for subsequent quantitative autoradiography. Plasma was separated from arterial blood by centrifugation, and its lipids were extracted by the method of Folch (Folch et al, 1957). Radioactivity in the organic fraction was measured by liquid scintillation counting.
Autoradiography and Calculations
Frozen brains were sectioned on a cryostat at −20°C. Sets of three adjacent 20-μm sections were collected and mounted on glass coverslips at 140 μm coronal intervals and dried. The three sections were exposed together with [3H]methylmethacrylate autoradiographic standards (Amersham, Arlington Heights, IL) to [3H]phosphor imaging plates (Fuji Medical Systems, Stamford, CT) for 7 days, which were then scanned by a BAS 5000 scanner system (West Lafayette, IN) following the manufacturer's instructions. An adjacent section was collected and stained with cresyl violet to identify brain regions using a rat-brain atlas (Paxinos and Watson, 1987).
Regional brain radioactivity was measured in sextuplicate by quantitative densitometry using phosphor-imaging software (Image Gauge V3.45, Fuji). Regional brain incorporation coefficients k* were calculated as

where k* is in units of ml/s/g; c*brain (20:min) is brain radioactivity at 20 min after the onset of infusion, in units of nCi/g; c*plasma is plasma fatty acid radioactivity in units of nCi per ml; and t is the time after the onset of [3H]arachidonate infusion.
Data were compared statistically using Prism software for the Macintosh (Abacus Concepts, Berkeley, CA) and are reported as means±SEM. Student's t-test tests were used to evaluate statistical significance between experimental and control means. P⩽0.05 was taken as indicating statistically significance.
RESULTS
Table 1 summarizes the mean physiological parameters in unanesthetized control and fluoxetine-treated rats. The control means are similar to published values (Qu et al, 2003) and were not changed significantly by drug.
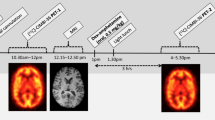
Figure 1 presents representative autoradiographs of coronal brain sections from a rat administered fluoxetine i.p. and a control rat. Fluoxetine 10 mg/kg i.p. caused significant widespread increases in k* for [3H]arachidonate. The mean regional incorporation coefficients k* corresponding to such increases are presented in Table 2.
As illustrated by Table 2, 30 min after fluoxetine administration, 42 of 85 brain regions had significantly increased mean values for k* (by about 30%) compared with control values. Significant increases were evident in prefrontal frontal, motor and somatosensory cortex, and olfactory and pyriform cortex, but not in the auditory or visual cortex. Regions in the caudate-putamen, nucleus accumbens, globus pallidus, amygdala, septum, thalamus, and hypothalamus also showed significant increments in k*, whereas significant changes generally were absent in regions of the brain stem, spinal cord, and cerebellum. The hippocampus showed elevations in CA1, CA2, and CA3 areas, but not in the dentate gyrus. The choroid plexus, where the control value of k* was much greater than in the brain parenchyma, demonstrated a 40% increase in k* in response to fluoxetine. White matter incorporation of [3H]arachidonate was unaffected by fluoxetine.
DISCUSSION
At 30 min following administration to unanesthetized adult male rats of fluoxetine (10 mg/kg i.p.), the incorporation coefficient k* for [3H]arachidonate was increased significantly compared with control in 45 of 85 brain regions that were examined. Significant increases were noted in regions of the prefrontal and frontal cortex, motor and somatosensory cortex, and of the basal ganglia, septum, hippocampus, thalamus, and hypothalamus, but not of the auditory or visual cortex, white matter, brain stem, spinal cord, or cerebellum (Table 2) (Appel et al, 1990; Li et al, 2001; Pazos and Palacios, 1985).
Fluoxetine, a high–affinity, high-selectivity antagonist of the serotonin reuptake transporter (Wong et al, 1991) promotes accumulation of 5-HT in the synaptic cleft. Acutely administered fluoxetine has been reported to increase extracellular 5-HT in many brain areas, including the striatum (Perry and Fuller, 1993; Rutter and Auerbach, 1993), thalamus (Dailey et al, 1992), diencephalon (Rutter et al, 1993), hypothalamus (Perry et al, 1993), and nucleus accumbens. Increases were evident within 30–60 min and last for up to 3 h (Guan et al, 1988). In light of our observations that DOI increases k* for [3H]arachidonate and that the increases can be blocked by a 5-HT2 antagonist (Qu et al, 2003), our results with fluoxetine (Table 2) suggest that increased synaptic cleft 5-HT caused by the drug indirectly increased the 5-HT occupancy of 5-HT2A/2C receptors, which are coupled to PLA2, so as to release arachidonic acid (Berg et al, 1998; Felder et al, 1990; Kim et al, 1999). The regional incorporation coefficient k* for [3H]arachidonate reflects this release (see Introduction) (Rapoport, 2001; Robinson et al, 1992).
While many brain areas with reported high densities of the serotonin reuptake transporter and of 5-HT2A/2C receptors demonstrated significant increases in k* for [3H]arachidonate in response to fluoxetine (Table 2), exceptions were evident. High densities of the serotonin reuptake transporter have been noted in the olfactory tubercle, lateral septal nucleus, olfactory tubercle, lateral septal nucleus, hypothalamic and thalamic nuclei, globus pallidus, central gray, superior colliculus, substantia nigra, interpeduncular nucleus, dorsal and lateral raphé, locus coeruleus. Lesser but nevertheless high densities are present in the frontal cortex, caudate-putamen, ventral pallidum, and hippocampus (Choi et al, 2000; De Souza and Kuyatt, 1987; McReynolds and Meyer, 1998; Moll et al, 2000). k* was elevated significantly in many of these regions, but not in all of them (eg lateral septal nucleus, superior colliculus, median, and dorsal raphé). High 5-HT2 receptor densities are reported in the cerebral cortex (particularly layer IV), olfactory and pyriform cortex, nucleus accumbens, caudate-putamen body and tail (Appel et al, 1990; Li et al, 2001; Pazos and Palacios, 1985). Frontal and motor cortical regions have higher densities than other cortical regions. Densities are not as high in the caudate-putamen head, globus pallidus, red nuclei, septal nuclei, and most parts of the hippocampus, thalamus, and hypothalamus. Spinal cord, brain stem, and cerebellum have few transporter or 5-HT2A/2C receptor sites, and as expected k* was not elevated significantly in these areas.
Increases in k* may not occur at all brain sites containing the serotonin reuptake transporter because transporter sites and postsynaptic 5-HT2A/2C receptors are not always colocalized. The transporter can be found at axons distant from 5-HT2 synapses (Zhou et al, 1998), and some 5-HT2 synapses may lack the transporter altogether (Brown and Molliver, 2000). Additionally, fluoxetine can increase brain dopamine levels (Yoshino et al, 2002) to activate PLA2 at dopaminergic D2 receptor sites rather than at 5-HT2A/2C receptor sites (Hayakawa et al, 2001; Vial and Piomelli, 1995). Finally, fluoxetine can noncompetitively inhibit cholinergic muscarinic (Owens et al, 1997) and nicotinic receptors (Fryer and Lukas, 1999) and thereby reduce release of arachidonic acid.
Indeed, PLA2 can be activated via a G-protein when an agonist binds to cholinergic muscarinic receptors and dopaminergic D2 receptors as well as to 5-HT2A/2C receptors (Bayon et al, 1997; Cooper et al, 1996; DeGeorge et al, 1991; Felder et al, 1990; Hayakawa et al, 2001; Kim et al, 1999; Vial et al, 1995). PLA2 also may be activated by Ca2+ entry into cells when glutamate acts at NMDA receptors or acetylcholine acts at nicotinic receptors. Thus, baseline k* for [3H]arachidonate in control rats represents the sum of baseline activation of PLA2 via these different receptor subtypes, as well as incorporation because of membrane synthesis (particularly relevant for white matter myelin) (Rapoport et al, 1997).
A 10-fold higher baseline value of k* for [3H]arachidonate in the choroid plexus, as well as a significant increment in k* in response to DOI or fluoxetine (Table 2) are consistent with high densities of 5-HT2C-binding sites in the choroid plexus (Kaufman et al, 1995; Li et al, 2001; Qu et al, 2003) and with activation of PLA2 via these receptors. Fluoxetine has been reported to bind to 5-HT2C sites in the choroid plexus (Palvimaki et al, 1996). The high baseline k* in the choroid plexus is consistent with high rates of uptake of radiolabeled fatty acids into median eminence, subfornical organ, pineal gland, adenohypophysis, and neurohypophysis (Noronha et al, 1990; Noronha et al, 1989; Qu et al, 2003). These regions lack the continuous capillary bed of the blood–brain barrier (Rapoport, 1976), allowing access of labeled fatty acid both in its unbound unesterified form (as for the brain parenchyma), and when bound to albumin (Robinson et al, 1992). High values of k* for labeled arachidonate also have been noted in the heart (Murphy et al, 2000).
Fluoxetine can induce hyperthermia in rats (Lin et al, 1998). The activity of PLA2 as well that of other enzymes might be expected to increase with an increase in temperature (Bell et al, 1996). However, it is unlikely that hyperthermia accounted for the findings in this paper, as increased values for k* were not found in regions having low densities of the serotonin reuptake transporter, and because body temperature was maintained between 36 and 37°C in this study (see Materials and methods). Additionally hyperthermia has been shown to produce widespread increases in rCMRglc in awake rats (Mickley et al, 1997), whereas fluoxetine, when administered under the same conditions in our study, has been shown either to not change or to reduce rCMRglc (Freo et al, 2000).
Serotonin release from presynaptic elements can be controlled by two types of autoreceptors (Cerrito and Raiteri, 1980). 5-HT1A autoreceptors are found at the somatodendritic region of cell bodies in midline and raphé nuclei in the pons and upper brain stem, whereas 5-HT1B autoreceptors are located at axon terminals, where they control local 5-HT synthesis and release (Cooper et al, 1996; Hervas et al, 2000; Martin and Sanders-Bush, 1982). Acutely administered fluoxetine has been reported to inhibit electrical activity of serotonin neurons by activating somatodendritic 5-HT1A autoreceptors (Czachura and Rasmussen, 2000; Fuller, 1995), thus reducing 5-HT released into the synaptic cleft. With chronic fluoxetine, inhibition of 5-HT unit activity is less because of desensitization of the 5-HT1A autoreceptor. Desensitization and recovery of firing of 5-HT neurons develop slowly and concurrently, and may contribute to the delayed onset of therapeutic efficacy (Bergqvist et al, 1999; Blier and De Montigny, 1983).
The widespread increments in k* for [3H]arachidonate in response to acute fluoxetine (Table 2) contrast with reports of no change or decrements in rCMRglc under comparable experimental conditions (Freo et al, 2000). A similar discrepancy between increased radiolabeled arachidonate incorporation but decreased or no change in rCMRglc follows DOI or methiothepin administration to unanesthetized rats (Freo et al, 1991; Qu et al, 2001b,2003; Ricchieri et al, 1987). These discrepancs likely arise because [3H]arachidonate incorporation localizes the postsynaptic PLA2-mediated release of arachidonic acid at the serotonergic neuron, whereas rCMRglc represents ATP consumption by the downstream firing of presynaptic axon terminals of that neuron (Ashby et al, 1990; Purdon and Rapoport, 1998; Qu et al, 2003; Sokoloff, 1999).
The frontal cortex and hippocampus have been implicated as sites of action of antidepressant drugs (Duman et al, 1997; Jacobson and Sapolsky, 1991). In this study (Table 2), incorporation coefficients k* for [3H]arachidonate were increased by fluoxetine in these regions, suggesting that to signaling via PLA2 at these sites contributes to fluoxetine's antidepressant action. In major depression, serotonergic neurotransmission may be disturbed and processes of cellular immunity may be activated, suggesting a relation between the two processes. Indeed, there appears to be a constant ‘crosstalk’ between the immune endocrine, central, and peripheral nervous systems which can involve serotonin and arachidonic acid metabolites (eg prostaglandins) (Leonard, 2001; Maier and Watkins, 1998).
In conclusion, we have demonstrated in unanesthetized rats that acute fluoxetine activates PLA2 signaling and increases labeled arachidonate incorporation from plasma into brain regions having high serotonin reuptake transporter densities, with some exceptions. Increased tracer incorporation likely arises because fluoxetine indirectly increases binding of 5-HT to PLA2-coupled 5-HT2A/2C receptors. Identifying the exact mechanisms of fluoxetine's acute action will entail using specific receptor antagonists with it (Hayakawa et al, 2001; Mazzola-Pomietto et al, 1997; Rabiner et al, 2002), or studying 5-HT2A or 5-HT2C knockout mice (Lira et al, 2001).
References
Appel NM, Mitchell WM, Gasrlick RK, Glennon RA, Teitler M, De Souza EB (1990). Autoradiographic characterization of (+−)-1-(2,5-dimethoxy-4-[125I]iodophenyl)-2-aminopropane ([125I]DOI) binding to 5-HT2 and 5-HT1C receptors in rat brain. J Pharmacol Exp Ther 255: 843–857.
Ashby Jr CR, Jiang LH, Kasser RJ, Wang RY (1990). Electro-physiological characterization of 5-hydroxytryptamine2 receptors in the rat medial prefrontal cortex. J Pharmacol Exp Ther 252: 171–178.
Axelrod J (1990). Receptor-mediated activation of phospholipase A2 and arachidonic acid release in signal transduction. Biochem Soc Trans 18: 503–507.
Bayon Y, Hernandez M, Alonso A, Nunez L, Garcia-Sancho J, Leslie C, Sanchez Crespo M, Nieto ML (1997). Cytosolic phospholipase A2 is coupled to muscarinic receptors in the human astrocytoma cell line 1321N1: characterization of the transducing mechanism. Biochem J 323: 281–287.
Bell JD, Burnside M, Owen JA, Royall ML, Baker ML (1996). Relationships between bilayer structure and phospholipase A2 activity: interactions among temperature, diacylglycerol, lysolecithin, palmitic acid, and dipalmitoylphosphatidylcholine. Biochemistry 35: 4945–4955.
Berg KA, Maayani S, Goldfarb J, Scaramellini C, Leff P, Clark WP (1998). Effector pathway-dependant relative efficacy at serotonin type 2A and 2C receptors: Evidence for agonist-directed trafficking of receptor stimulus. Mol Pharmacol 54: 94–104.
Bergqvist PB, Bouchard C, Blier P (1999). Effect of long-term administration of antidepressant treatments on serotonin release in brain regions involved in obsessive–compulsive disorder. Biol Psychiatry 45: 164–174.
Blier P, De Montigny C (1983). Electrophysiological investigations on the effect of repeated zimelidine administration on serotonergic neurotransmission in the rat. J Neurosci 3: 1270–1278.
Brown P, Molliver ME (2000). Dual serotonin (5-HT) projections to the nucleus accumbens core and shell: relation of the 5-HT transporter to amphetamine-induced neurotoxicity. J Neurosci 20: 1952–1963.
Cerrito F, Raiteri M (1980). Presynaptic autoreceptors control serotonin release from central nerve endings. Pharmacol Res Commun 12: 593–597.
Chang MCJ, Arai T, Freed LM, Wakabayashi S, Channing MA, Dunn BB, Der MG, Bell JM, Sasaki T, Herscovitch P, Eckelman WC, Rapoport SI (1997). Brain incorporation of [1-11C]-arachidonate in normocapnic and hypercapnic monkeys, measured with positron emission tomography. Brain Res 755: 74–83.
Choi SR, Hou C, Oya S, Mu M, Kung MP, Siciliano M, Acton PD, Kung HF (2000). Selective in vitro and in vivo binding of [(125)I]ADAM to serotonin transporters in rat brain. Synapse 38: 403–412.
Cook Jr EH, Metz J, Leventhal BL, Lebovitz M, Nathan M, Semerdjian SA, Brown T, Cooper MD (1994). Fluoxetine effects on cerebral glucose metabolism. Neuroreport 5: 1745–1748.
Cooper JR, Bloom FE, Roth RH (1996). The Biochemical Basis of Neuropharmacology, 7th edn. Oxford University Press: Oxford.
Czachura JF, Rasmussen K (2000). Effects of acute and chronic administration of fluoxetine on the activity of serotonergic neurons in the dorsal raphe nucleus of the rat. Naunyn Schmiedebergs Arch Pharmacol 362: 266–275.
Dailey JW, Yan QS, Mishra PK, Burger RL, Jobe PC (1992). Effects of fluoxetine on convulsions and on brain serotonin as detected by microdialysis in genetically epilepsy-prone rats. J Pharmacol Exp Ther 260: 533–540.
DeGeorge JJ, Nariai T, Yamazaki S, Williams WM, Rapoport SI (1991). Arecoline-stimulated brain incorporation of intravenously administered fatty acids in unanesthetized rats. J Neurochem 56: 352–355.
De Souza EB, Kuyatt BL (1987). Autoradiographic localization of 3H-paroxetine-labeled serotonin uptake sites in rat brain. Synapse 1: 488–496.
Dinan TG (1996). Serotonin: current understanding and the way forward. Int Clin Psychopharmacol 11(Suppl 1): 19–21.
Duman RS, Heninger GR, Nestler EJ (1997). A molecular and cellular theory of depression. Arch Gen Psychiatry 54: 597–606.
Felder CC, Kanterman RY, Ma AL, Axelrod J (1990). Serotonin stimulates phospholipase A2 and the release of arachidonic acid in hippocampal neurons by a type 2 serotonin receptor that is independent of inositol phospholipid hydrolysis. Proc Natl Acad Sci USA 87: 2187–2191.
Fitzpatrick F, Soberman R (2001). Regulated formation of eicosanoids. J Clin Invest 107: 1347–1351.
Folch J, Lees M, Sloane Stanley GH (1957). A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem 226: 497–509.
Freo U, Ori C, Dam M, Merico A, Pizzolato G (2000). Effects of acute and chronic treatment with fluoxetine on regional glucose cerebral metabolism in rats: implications for clinical therapies. Brain Res 854: 35–41.
Freo U, Soncrant TT, Holloway HW, Rapoport SI (1991). Dose- and time-dependent effects of 1-(2,5-dimethoxy-4-iodophenyl)-2-aminopropane (DOI), a serotonergic 5-HT2 receptor agonist, on local cerebral glucose metabolism. Brain Res 541: 63–69.
Fryer JD, Lukas RJ (1999). Antidepressants noncompetitively inhibit nicotinic acetylcholine receptor function. J Neurochem 72: 1117–1124.
Fuller RW (1995). Serotonin uptake inhibitors: uses in clinical therapy and in laboratory research. Prog Drug Res 45: 167–204.
Fuller RW, Wong DT (1977). Inhibition of serotonin reuptake. Fed Proc 36: 2154–2158.
Griebel G, Blanchard DC, Agnes RS, Blanchard RJ (1995). Differential modulation of antipredator defensive behavior in Swiss-Webster mice following acute or chronic administration of imipramine and fluoxetine. Psychopharmacology (Berl) 120: 57–66.
Guan XM, McBride WJ (1988). Fluoxetine increases the extracellular levels of serotonin in the nucleus accumbens. Brain Res Bull 21: 43–46.
Hayakawa T, Chang MC, Rapoport SI, Appel NM (2001). Selective dopamine receptor stimulation differentially affects [3H]arachidonic acid incorporation, a surrogate marker for phospholipase A2-mediated neurotransmitter signal transduction, in a rodent model of Parkinson's disease. J Pharmacol Exp Ther 296: 1074–1084.
Hervas I, Queiroz CM, Adell A, Artigas F (2000). Role of uptake inhibition and autoreceptor activation in the control of 5-HT release in frontal cortex and dorsal hippocampus of the rat. Br J Pharmacol 130: 160–166.
Jacobson L, Sapolsky R (1991). The role of the hippocampus in feedback regulation of the hypothalamic–pituitary–adrenocortical axis. Endocr Rev 12: 118–134.
Jones CR, Arai T, Bell JM, Rapoport SI (1996). Preferential in vivo incorporation of [3H]arachidonic acid from blood into rat brain synaptosomal fractions before and after cholinergic stimulation. J Neurochem 67: 822–829.
Kaufman MJ, Hartig PR, Hoffman BJ (1995). Serotonin 5-HT2C receptor stimulates cyclic GMP formation in choroid plexus. J Neurochem 64: 199–205.
Kim HY, Edsall L, Garcia M, Zhang H (1999). The release of polyunsaturated fatty acids and their lipoxygenation in the brain. Adv Exp Med Biol 447: 75–85.
Kurt M, Arik AC, Celik S (2000). The effects of sertraline and fluoxetine on anxiety in the elevated plus-maze test in mice. J Basic Clin Physiol Pharmacol 11: 173–180.
Leonard BE (2001). Stress, norepinephrine and depression. J Psychiatry Neurosci 26(Suppl): S11–S16.
Li Q, Levy AD, Cabrera TM, Brownfield MS, Battaglia G, Van de Kar LD (1993). Long-term fluoxetine, but not desipramine, inhibits the ACTH and oxytocin responses to the 5-HT1A agonist, 8-OH-DPAT, in male rats. Brain Res 630: 148–156.
Li Q, Ma L, William K, Murphy DL (2001). 5-HT2A and 5-HT2C receptors are differently regulated in 5-HT transporter mice: studies on the density and gene expression of the receptors. Soc Neurosci Abstr 26: 380.5.
Lin MT, Tsay HJ, Su WH, Chueh FY (1998). Changes in extracellular serotonin in rat hypothalamus affect thermoregulatory function. Am J Physiol 274: R1260–R1267.
Lira A, Bradley-Moore M, Zhou M, Fairhurst S, Menzaghi F, Brunner D, Gingrich JA (2001). Cognitive performance in 5-HT2A receptor knockout mice. Soc Neurosci Abstr 27: 380.4.
Maier SF, Watkins LR (1998). Cytokines for psychologists: implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychol Rev 105: 83–107.
Martin LL, Sanders-Bush E (1982). Comparison of the pharmacological characteristics of 5 HT1 and 5 HT2 binding sites with those of serotonin autoreceptors which modulate serotonin release. Naunyn Schmiedebergs Arch Pharmacol 321: 165–170.
Mazzola-Pomietto P, Aulakh CS, Tolliver T, Murphy DL (1997). Functional subsensitivity of 5-HT2A and 5-HT2C receptors mediating hyperthermia following acute and chronic treatment with 5-HT2A/2C receptor antagonists. Psychopharmacology (Berl) 130: 144–151.
McReynolds AM, Meyer JS (1998). Effects of prenatal cocaine exposure on serotonin and norepinephrine transporter density in the rat brain. Ann NY Acad Sci 846: 412–414.
Mickley GA, Cobb BL, Farrell ST (1997). Brain hyperthermia alters local cerebral glucose utilization: a comparison of hyperthermic agents. Int J Hyperthermia 13: 99–114.
Moll GH, Mehnert C, Wicker M, Bock N, Rothenberger A, Ruther E, Huether G (2000). Age-associated changes in the densities of presynaptic monoamine transporters in different regions of the rat brain from early juvenile life to late adulthood. Brain Res Dev Brain Res 119: 251–257.
Murphy EJ, Rosenberger TA, Patrick CB, Rapoport SI (2000). Intravenously injected [1-14C]arachidonic acid targets phospholipids, and [1-14C]palmitic acid targets neutral lipids in hearts of awake rats. Lipids 35: 891–898.
Noronha JG, Bell JM, Rapoport SI (1990). Quantitative brain autoradiography of [9,10-3H]palmitic acid incorporation into brain lipids. J Neurosci Res 26: 196–208.
Noronha JG, Larson DM, Rapoport SI (1989). Regional cerebral incorporation of plasma [14-C]palmitate, and cerebral glucose utilization in water-deprived Long-Evans and Brattleboro rats. Exp Neurol 103: 267–276.
Owens MJ, Morgan WN, Plott SJ, Nemeroff CB (1997). Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites. J Pharmacol Exp Ther 283: 1305–1322.
Palvimaki EP, Roth BL, Majasuo H, Laakso A, Kuoppamaki M, Syvalahti E, Hietala J (1996). Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor. Psychopharmacology (Berl) 126: 234–240.
Paxinos G, Watson C (1987). The Rat Brain in Stereotaxic Coordinates, 3rd edn. Academic Press: New York.
Pazos A, Palacios JM (1985). Quantitative autoradiographic mapping of serotonin receptor in the rat brain. I. Serotonin-1 receptors. Brain Res 346: 205–230.
Perry KW, Fuller RW (1993). Extracellular 5-hydroxytryptamine concentration in rat hypothalamus after administration of fluoxetine plus L-5-hydroxytryptophan. J Pharmacol 45: 759–761.
Purdon AD, Rapoport SI (1998). Energy requirements for two aspects of phospholipid metabolism in mammalian brain. Biochem J 335: 313–318.
Qu Y, Chang L, Klaff J, Balbo A, Rapoport SI (2001a). Imaging phospholipase A2 mediated signal transduction in response to a 5-HT2 agonist in brain of awake rats. J Neurochem 78(Suppl 1): 144.
Qu Y, Chang L, Klaff J, Balbo A, Rapoport SI (2001b). In vivo neuroimaging of serotonin-mediated phospholipase A2 signal transduction in awake rats: effect of methiothepin. J Neurochem (Abstr) 78(Suppl 1): 152.
Qu Y, Chang L, Klaff J, Balbo A, Rapoport SI (2003). Imaging brain phospholipase A2 activation in awake rat in response to 5-HT2A/2C agonist, (+-)-2,5-dimethoxy-4-iodophenyl-2-aminopropane (DOI). Neuropsychopharmacology 28: 244–252.
Rabiner EA, Wilkins MR, Turkheimer F, Gunn RN, De Haes JU, De Vries M, Grasby PM (2002). 5-Hydroxytryptamine (1A) receptor occupancy by novel full antagonist 2-[4-[4-(7-chloro-2,3-dihydro-1,4-benzdioxyn-5-yl)-1-piperazinyl]butyl]-1, 2-benzisothiazol-3-(2H)-one-1,1-dioxide: A [(11)C][O-methyl-3H]-N-(2-(4-(2-methoxyphenyl)-1-piperazinyl)ethyl)-N-(2-p yridinyl)cyclohexanecarboxamide trihydrochloride (WAY-100635) positron emission tomography study in humans. J Pharmacol Exp Ther 301: 1144–1150.
Rapoport SI (1976). Blood–Brain Barrier in Physiology and Medicine. Raven Press: New York.
Rapoport SI (2001). In vivo fatty acid incorporation into brain phospholipids in relation to plasma availability, signal transduction and membrane remodeling. J Mol Neurosci 16: 243–261.
Rapoport SI, Purdon D, Shetty HU, Grange E, Smith Q, Jones C, Chang MCJ (1997). In vivo imaging of fatty acid incorporation into brain to examine signal transduction and neuroplasticity involving phospholipids. Ann NY Acad Sci 820: 56–74.
Ricchieri GL, Soncrant TT, Holloway HW, Rapoport SI (1987). Methiothepin reduces glucose utilization in forebrain regions of awake rats. Psychopharmacology (Berl) 93: 449–456.
Robinson PJ, Noronha J, DeGeorge JJ, Freed LM, Nariai T, Rapoport SI (1992). A quantitative method for measuring regional in vivo fatty-acid incorporation into and turnover within brain phospholipids: review and critical analysis. Brain Res Rev 17: 187–214.
Rutter JJ, Auerbach SB (1993). Acute uptake inhibition increases extracellular serotonin in the rat forebrain. J Pharmacol Exp Ther 265: 1319–1324.
Sills TL, Greenshaw AJ, Baker GB, Fletcher PJ (1999). Acute fluoxetine treatment potentiates amphetamine hyperactivity and amphetamine-induced nucleus accumbens dopamine release: possible pharmacokinetic interaction. Psychopharmacology (Berl) 141: 421–427.
Sokoloff L (1999). Energetics of functional activation in neural tissues. Neurochem Res 24: 321–329.
Stanford JA, Currier TD, Gerhardt GA (2002). Acute locomotor effects of fluoxetine, sertraline, and nomifensine in young versus aged Fischer 344 rats. Pharmacol Biochem Behav 71: 325–332.
To CT, Anheuer ZE, Bagdy G (1999). Effects of acute and chronic fluoxetine treatment of CRH-induced anxiety. Neuroreport 10: 553–555.
Torres G, Horowitz JM, Laflamme N, Rivest S (1998). Fluoxetine induces the transcription of genes encoding c-fos, corticotropin-releasing factor and its type 1 receptor in rat brain. Neuroscience 87: 463–477.
Vial D, Piomelli D (1995). Dopamine D2 receptors potentiate arachidonate release via activation of cytosolic, arachidonic-specific phospholipase A2. J Neurochem 64: 2765–2772.
Wong DT, Bymaster FP, Engleman EA (1995). Prozac (fluoxetine, Lilly 110140), the first selective serotonin uptake inhibitor and an antidepressant drug: twenty years since its first publication. Life Sci 57: 411–441.
Wong DT, Threlkeld PG, Robertson DW (1991). Affinities of fluoxetine, its enantiomers, and other inhibitors of serotonin uptake for subtypes of serotonin receptors. Neuropsychopharmacology 5: 43–47.
Yoshino T, Nisijima K, Katoh S, Yui K, Nakamura M (2002). Tandospirone potentiates the fluoxetine-induced increases in extracellular dopamine via 5-HT(1A) receptors in the rat medial frontal cortex. Neurochem Int 40: 355–360.
Zhou FC, Tao-Cheng JH, Segu L, Patel T, Wang Y (1998). Serotonin transporters are located on the axons beyond the synaptic junctions: anatomical and functional evidence. Brain Res 805: 241–254.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qu, Y., Chang, L., Klaff, J. et al. Imaging Brain Phospholipase A2-Mediated Signal Transduction in Response to Acute Fluoxetine Administration in Unanesthetized Rats. Neuropsychopharmacol 28, 1219–1226 (2003). https://doi.org/10.1038/sj.npp.1300177
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300177
Keywords
This article is cited by
-
A high coverage pseudotargeted lipidomics method based on three-phase liquid extraction and segment data-dependent acquisition using UHPLC-MS/MS with application to a study of depression rats
Analytical and Bioanalytical Chemistry (2021)
-
Brain Arachidonic Acid Incorporation and Turnover are not Altered in the Flinders Sensitive Line Rat Model of Human Depression
Neurochemical Research (2015)
-
Chronic treatment of astrocytes with therapeutically relevant fluoxetine concentrations enhances cPLA2 expression secondary to 5-HT2B-induced, transactivation-mediated ERK1/2 phosphorylation
Psychopharmacology (2009)
-
Diverse antidepressants increase CDP-diacylglycerol production and phosphatidylinositide resynthesis in depression-relevant regions of the rat brain
BMC Neuroscience (2008)
-
RETRACTED ARTICLE: Chronic fluoxetine increases cytosolic phospholipase A2 activity and arachidonic acid turnover in brain phospholipids of the unanesthetized rat
Psychopharmacology (2007)