Abstract
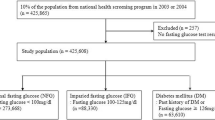
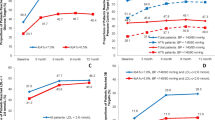
Abnormal glucose metabolism (AGM) is common but underestimated in patients with coronary heart disease (CHD). Here, we reported 898 in-hospital patients with primary hypertension (PH) at the university hospitals in developed regions of China. Oral glucose tolerance test (OGTT) was performed in those without known type-2 diabetes mellitus (2-DM). A total of 158 patients had known 2-DM and 32 were newly diagnosed as 2-DM by fasting blood glucose (FBG). OGTT revealed that 83 had 2-DM and 296 had impaired glucose tolerance (IGT). The proportion of 2-DM and AGM increased from 21.2 to 30.4% and from 57.5 to 68.7% upon OGTT. Prevalence of AGM and 2-DM increased with the increase of age, and incidence of AGM and 2-DM was significant higher in patients with risk factors (including CHD, overweight, hyperlipidaemia, proteinuria) than those without risk factors mentioned above. Glucose was not sufficiently controlled in 55.1% of the patients with 2-DM upon treatment, well controlled in 35.4% and not controlled in 9.5%. So AGM is also prevalent in PH patients especially the elders and those with risk factors, which was underestimated in most cases. Moreover, much lower awareness, treatment and control of 2-DM occurred in some regions of China, thus strengthening health education for patients and heightening consciousness of doctor are very important and eminent. Except for FBG, more attention should be paid to postprandial blood glucose ignored before, and OGTT should be a routine procedure in PH patients, especially in older patients and those with the factors mentioned above.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Donahoe SM, Stewart GC, McCabe CH, Mohanavelu S, Murphy SA, Cannon CP et al. Diabetes and mortality following acute coronary syndromes. JAMA 2007; 298: 765–775.
Mak KH, Ma S, Heng D, Tan CE, Tai ES, Topol EJ et al. Impact of sex, metabolic syndrome, and diabetes mellitus on cardiovascular events. Am J Cardiol 2007; 100: 227–233.
Takahashi K, Bokura H, Kobayashi S, Iijima K, Nagai A, Yamaguchi S . Metabolic syndrome increases the risk of ischemic stroke in women. Intern Med 2007; 46: 643–648.
Jeerakathil T, Johnson JA, Simpson SH, Majumdar SR . Short-term risk for stroke is doubled in persons with newly treated type 2 diabetes compared with persons without diabetes: a population-based cohort study. Stroke 2007; 38: 1739–1743.
European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2007 guidelines for the management of arterial hypertension. J Hypertens 2007; 25: 1105–1187.
Weitzman D, Goldbourt U . The significance of various blood pressure indices for long-term stroke, coronary heart disease, and all-cause mortality in men: the Israeli Ischemic Heart Disease study. Stroke 2006; 37: 358–363.
Multiple Risk Factor Intervention Trial Research Group. Design considerations in the NHLBI Multiple Risk Factor Intervention Trial (MRFIT). Control Clin Trial 1987; 8: 41S–53S.
The Treatment of Mild Hypertension Research Group. The Treatment of Mild Hypertension Study (TOMHS): final results. JAMA 1993; 270: 713–724.
Franklin SS, Khan SA, Wong ND, Larson MG, Levy D . Is pulse pressure useful in predicting the risk for coronary heart disease? The Framingham Heart Study. Circulation 1999; 100: 354–360.
Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation 2001; 103: 1245–1249.
Hypertension in Diabetes Study IV. Therapeutic requirements to maintain tight blood pressure control. Diabetologia 1996; 39: 1554–1561.
UK Prospective Diabetes Study Group. Tight blood pressure and risk of macrovascular and microvascular complications in type-2 diabetes (UKPDS 38). BMJ 1998; 317: 703–713.
Donnelly R, Emslie-Smith AM, Gardner ID, Morris AD . ABC of arterial and venous disease: vascular complications of diabetes. BMJ 2000; 320: 1062–1066.
Mariosa LS, Ribeiro-Filho FF, Ribeiro AB, Zanella MT . Diagnosing abnormal glucose tolerance in hypertensive women: are we making the best choice? J Cardiometab Syndr 2007; 2: 98–103.
Essien OE, Peters EJ, Udoh AE, Ekott JU, Odigwe CO . Prevalence and pattern of abnormal glucose tolerance in adult Nigerians with primary hypertension. Niger J Med 2007; 16: 50–56.
Garcia-Puig J, Ruilope LM, Luque M, Fernandez J, Ortega R, Dal-Re R, AVANT Study Group Investigators. Glucose metabolism in patients with essential hypertension. Am J Med 2006; 119: 318–326.
Guideline Enactment Committee of Prevention and Treatment of Dyslipidemia. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Chin J Cardiol 2007; 35: 390–409.
Genuth S . Lowering the criterion for impaired fasting glucose is in order. Diabetes Care 2003; 26: 3331–3332.
International Diabetes Federation. Diabetes atlas. http://www.eatlas.idf.org(8 August 2006).
Diabetes Study Group of Science-Technology Project of the National ‘Ninth Five-Year-Plan’ of China. Epidemiologic study of diabetes mellitus and impaired glucose tolerance in middle and old aged people of China. Chin J Epidemiol 2003; 24: 410–412.
Bartnik M, Ryden L, Ferrari R, Malmberg K, Pyorala K, Simoons M et al. The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. The Euro Heart Survey on Diabetes and the Heart. Eur Heart J 2004; 25: 1880–1890.
Hu DY, Pan CY, Yu JM, China Heart Survey Group. The relationship between coronary artery disease and abnormal glucose regulation in China: the China Heart Survey. Eur Heart J 2006; 27: 2573–2579.
Wu YF, Xie GQ, Li Y, Zhao LC, Zhou BF . The current status on the prevalence, awareness, treatment and control of diabetes mellitus in several Chinese subpopulations. Chin J Epidemiol 2005; 26: 564–568.
Acknowledgements
We are indebted to our nurses, in particular Ms QiaoHui Xie for her help to us and all the dedicated assistance to patients. We thank professor ErWei Song from Sun Yat-sen Memorial Hospital for editing the paper. We also thank our colleagues, in particular, Dr YingSheng Xue, Dr Chang Fang, Dr NianSang Luo and Dr ZhiBin Huang.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, YX., Wang, XQ., Wang, JF. et al. Glucometabolic state of in-hospital patients with primary hypertension in sub-population of partial regions in China. J Hum Hypertens 22, 346–351 (2008). https://doi.org/10.1038/sj.jhh.1002327
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1002327