Abstract
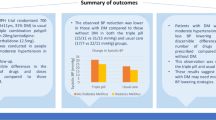
Suboptimal management of hypertension is often a result of poor patient compliance in the form of missed doses of their antihypertensive medication. This multicentre, randomised, double-blind, parallel-group trial was designed to compare the persistence of the antihypertensive efficacy of the amlodipine and nifedipine gastrointestinal therapeutic system (GITS) after two ‘missed doses’, and also to compare the drugs' overall efficacy and safety in Asian patients with mild-to-moderate essential hypertension. Following a 2-week placebo run-in period, 222 patients were randomised to receive either amlodipine (5 mg daily, increased after 6 weeks if necessary to 10 mg daily, n=109) or nifedipine GITS (30 mg daily, increased after 6 weeks if necessary to 60 mg daily; n=113) for 12 weeks. A placebo was then substituted for further 2 days with continuous ambulatory blood pressure (BP) monitoring. The increases in the last 9 h of mean ambulatory BP on day 2 after treatment withdrawal were significantly less with amlodipine than with nifedipine GITS: 4.4±7.0 vs 11.2±11.3 mmHg for systolic BP (P⩽0.0001) and 2.4±6.3 vs 6.0±6.0 mmHg for diastolic BP (P⩽0.0002). Significant differences between the two drugs in mean 24-h ambulatory BP levels were already evident on day 1 after withdrawal, even though there were no significant differences on the final day of treatment. No differences in safety parameters were observed, and neither drug caused any serious or severe treatment-related adverse events. In conclusion, amlodipine provides greater protection than nifedipine GITS against loss of BP control following missed doses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. The Sixth Report of the US Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure Arch Intern Med 1997 157: 2413–2446
World Health Organization (WHO)–International Society of Hypertension (ISH). 1999 World Health Organization–International society of Hypertension Guidelines for the management of Hypertension J Hypertens 1999 17: 151–183
Ramsay L et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society J Hum Hypertens 1999 13: 569–592
Meredith PA . The importance of sustained blood pressure control J Cardiovasc Pharmacol 2000 35: (Suppl 3) S7–S11
Mancia G et al. for the SAMPLE Study Group. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy Circulation 1997 95: 1464–1470
McInnes GT . Integrated approaches to management of hypertension: promoting treatment acceptance Am Heart J 1999 138: (part 2) 252–255
Burnier M . Long-term compliance with antihypertensive therapy: another facet of chornotherapeutics in hypertension Blood Press Monit 2000 5: (Suppl 1) S31–S34
Trilling JS, Froom J . The urgent need to improve hypertension care Arch Fam Med 2000 9: 794–801
Williams GH . Assessing patient wellness: new perspectives on quality of life and compliance Am J Hypertens 1998 11: (Part 2) 186S–191S
Rudd P . Compliance with antihypertensive therapy: raising the bar of expectations Am J Manag Care 1998 4: 957–966
Mallion JM et al. Compliance, electronic monitoring and antihypertensive drug J Hypertens 1998 16: (Suppl 1) S75-S79
Payne KA, Esmonde-White S . Observational studies of antihypertensive medication use and compliance: is drug choice a factor in treatment adherence? Curr Hypertens Rep 2002 2: 515–524
Haria M, Wagstaff AJ . Amlodipine: a reappraisal of its pharmacological properties and therapeutic use in cardiovascular disease Drugs 1995 50: 560–586
Brogden RN, McTavish D . Nifedipine gastrointestinal therapeutic system (GITS). A review of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy in hypertension and angina pectoris Drugs 1995 50: 495–512
Mancia G et al. Relation between blood pressure variability and carotid artery damage in hyper-tension: baseline data from the European Lacidipine Study on Atherosclerosis J Hypertens 2001 19: 1981–1989
Ueda S et al. A comparative assessment of the duration of action of amlodipine and nifedipine GITS in normotensive subjects Br J Clin Pharmacol 1993 36: 561–566
Zanchetti A et al. Antihypertensive effects of nifedipine gastrointestinal therapeutic system on clinic and ambulatory blood pressure in essential hypertensives J Hypertens 1993 11: (Suppl 5) s334–s335
Zanchetti A et al. Antihypertensive effects of nifedipine GITS on clinic and ambulatory blood pressure in essential hypertensives High Blood Press 1994 3: 45–56
Ferruci et al. 24-blood pressure profiles in patients with hypertension treated with amlodipine or nifedipine GITS Clin Drug Invest 1997 13: (Suppl 1) 67–72
Elliott HL . Persistence of antihypertensive efficacy after missed doses: comparison of amlodipine and nifedipine GITS [abstract] J Hypertens 1997 15: (Suppl 4) 8B7
Nussinovitch N, Rosenberg G, Peleg E, Rosenthal T . A comparative crossover evaluation of amlodipine and nifedipine GITS before and after a missed dose: 48-h blood pressure profiles Am J Hypertens 2002 15: 580–582
Motero J et al. Long acting calcium channel blockers in hypertension. Amlodipine vs nifedipine GITS comparative study [abstract] Am J Hypertens 1998 11: 69A
Hernandez-Hernandez R et al. The effects of a miss-ing dose of enalapril versus amlodipine on ambula-tory blood pressure Blood Press Monit 1996 1: 121–126
Leenen FH, Fourney A, Notman G, Tanner J . Persistence of anti-hypertensive effect after ‘missed doses’ of calcium antagonist with long (amlodipine) vs short (diltiazem) elimination half-life Br J Clin Pharmacol 1996 41: 83–88
Acknowledgements
This study was supported by Pfizer, Inc.
Author information
Authors and Affiliations
Appendix
Appendix
Members of the study group who conducted this trial were:
China: Principal investigators: Hu Dayi, Beijing Chaoyang Hospital, Beijing; Zhuo-Ren Lu, Xian Medical University First Affiliated Hospital, Xian. Co-investigators: Zhao Xiuli, Xu Zhimin, Liu Xiaohui, Cui Liang, Beijing Chaoyang Hospital, Beijing; Xue Xiaolin, Yuan Zuyi, Wang Dongqi, Qu Yi, Xian Medical University First Affiliated Hospital, Xian. Study coordinators: Yin Rongxiu, Beijing Chaoyang Hospital, Beijing; Guo Ning, Min Hui-e, Xian Medical University First Affiliated Hospital, Xian.
Hong Kong: Principal investigator: John Sanderson, The Chinese University of Hong Kong, Hong Kong. Co-investigator: Brian Tomlinson, The Chinese University of Hong Kong, Hong Kong. Study Coordinator: Wong Sau Ying, The Chinese University of Hong Kong, Hong Kong.
Indonesia: Principal investigators: Pudji Rahardjo, Rumah Sakit Cipto Mangunkusumo, Jakarta; Arieska Ann Soenarta, Rumah Sakit Harapan Kita, Jakarta. Co-investigators: Lucky Azizah Bawazier, Rumah Sakit Cipto Mangunkusomo, Jakarta; Santoso Karo-karo, Ismoyo Sunu, Rumah Sakit Harapan Kita, Jakarta. Study coordinators: Nanit Rahardjo, Rumah Sakit Cipto Mangunkusomo, Jakarta; Lasmaria Sitorus, Rumah Sakit Harapan Kita, Jakarta.
Malaysia: Principal investigators: Dato Robaayah Zambahari, Institute Jantung Negara, Kuala Lumpur; Christina Tan, University Hospital, Kuala Lumpur. Co-investigators: Na Boon Seng, Lam Kai Huat, Institute Jantung Negara, Kuala Lumpur; Chia Yook Chin, Chua Chin Teong, Lang Chim Choy, University Hospital, Kuala Lumpur. Study coordinators: Chia See Moi, Fong Chew Khew, Institute Jantung Negara, Kuala Lumpur; Tan Chan Soo Looi, University Hospital, Kuala Lumpur.
Philippines: Principal investigators: Dante Morales, Manila Doctors Hospital, Manila; Isabelo Ongtengco, St Luke's Medical Center, Quezon City. Co-investigators: Rody Sy, Rafael Castillo, Dennis Donor, Philip Chua, Manila Doctor's Hospital, Manila; Abondino Yunque, Michael Mercier Enriquez, St Luke's Medical Center, Quezon City. Study coordinators: Dannette Marbella, Manila Doctor's Hospital, Manila; Beverly Anne Callejo, St. Luke's Medical Center, Quezon City.
Singapore: Principal investigator: Tan Kok Soon, Changi General Hospital. Co-investigator: Woon Voon Ching, Changi General Hospital. Study Coordinator: Yew Lay Hwa, Changi General Hospital, Singapore.
Taiwan: Principal investigators: Chung-Yin Chen, Kuang-Tien General Hospital, Taichung; Der-Jinn Wu, Chung-Shan Medical and Dental College, Taichung. Co-investigators: Shih-Chung Huang, Mau-Rem Lin, Kuang Tien General Hospital, Taichung; Kwo-Chang Ueng, Chung-Shan Medical and Dental College, Taichung. Study coordinators: Chiao-Ling Chang, Kuang-Tien General Hospital, Taichung; Miao-Chi Chiu, Chung-Shan Medical and Dental College, Taichung.
Thailand: Principal investigators: Supachai Tanomsup, Ramathibodi Hospital, Mahidol University, Bangkok; Peera Buranakitjaroen, Siriraj Hospital, Mahidol University, Bangkok. Co-investigators: Suchet Takdhada, Ramathibodi Hospital, Mahidol University, Bangkok; Meta Phoojaroenchanachai, Siriraj Hospital, Mahidol University, Bangkok. Study coordinators: Nongluck Intarayota, Ramathibodi Hospital, Mahidol University, Bangkok; Surachai Saravich, Siriraj Hospital, Mahidol University, Bangkok.
Rights and permissions
About this article
Cite this article
Ongtengco, I., Morales, D., Sanderson, J. et al. Persistence of the antihypertensive efficacy of amlodipine and nifedipine GITS after two ‘missed doses’: a randomised, double-blind comparative trial in Asian patients. J Hum Hypertens 16, 805–813 (2002). https://doi.org/10.1038/sj.jhh.1001485
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001485