Abstract
OBJECTIVE: To determine the influence of body mass index (BMI) on agreement between the American Diabetes Association (ADA) and the new World Health Organization diagnostic criteria for the diagnosis of diabetes mellitus and to investigate the metabolic profile of the resulting subcategories.
DESIGN: Cross-sectional study
SUBJECTS: A total of 3018 subjects with no previous history of diabetes and fasting glucose <7.8 mmol/l, with a wide range of BMIs.
MEASUREMENTS: (1) Prevalence of impaired glucose regulation (IGR) and diabetes (DM) according to ADA and WHO diagnostic criteria; (2) basal and post-load insulin sensitivity and secretion, calculated on the basis of data derived from an oral glucose tolerance test (OGTT).
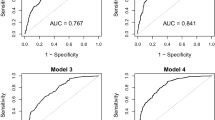
RESULTS: The diagnosis according to the two classifications was concordant in 2490 subjects, discordant in 528 (452 were identified as impaired glucose tolerance (IGT) and 76 as DM only by means of OGTT). The disagreement increased with increasing BMI, being as high as 25.3% in subjects with BMI ≥35 kg/m2. Subjects with isolated fasting hyperglycaemia were mainly characterised by reduced insulin sensitivity and secretion in the basal state, but normal first-phase insulin secretion and moderately reduced insulin sensitivity after glucose challenge. Subjects with isolated 2 h hyperglycaemia were mainly characterised by normal basal insulin secretion and by a marked insulin resistance associated with a blunted first-phase insulin secretion after the glucose load.
CONCLUSIONS: The disagreement between ADA and WHO classifications is particularly relevant in obesity, making OGTT mandatory in these subjects. Different pathogenic mechanisms are involved in isolated fasting or post-load hyperglycaemia, possibly related to a different site of insulin resistance (hepatic vs peripheral), and/or to a different disregulation of insulin secretion (basal vs post-load). A correct identification of the underlying mechanism(s) is the rationale for future studies to detect the effectiveness of different pharmacological or behavioural approaches.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Diabetes Care 1997 20: 1183–1197.
National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance Diabetes 1979 28: 1039–1057.
DECODE Study Group, on behalf of the European Diabetes Epidemiology Study Group. Will new diagnostic criteria for diabetes mellitus change phenotype of patients with diabetes? Reanalysis of European epidemiological data Br Med J 1998 317: 371–375.
Shaw JE, de Courten M, Boyko EJ, Zimmett PZ . Impact of new diagnostic criteria for diabetes on different populations Diabetes Care 1999 22: 762–766.
Lee ET, Howard BV, Go O, Savage PJ, Fabsitz RR, Robbins DC, Welty TK . Prevalence of undiagnosed diabetes in three America Indian populations Diabetes Care 2000 23: 181–186.
Alberti KGMM, Zimmet PZ for the WHO Consultation . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation Diabetes Med 1998 15: 539–553.
Shaw JE, Zimmet PZ, de Courten M, Dowse GK, Chitson P, Gareboo H, Hemraj F, Fareed D, Tuomilehto J, Alberti KGMM . Impaired fasting glucose or impaired glucose tolerance Diabetes Care 1999 22: 399–402.
Weyer C, Bogardus C, Pratley RE . Metabolic characteristics of individuals with impaired fasting glucose and/or impaired glucose tolerance Diabetes 1999 48: 2197–2203.
Davies MJ, Raymond NT, Day JL, Hales CN, Burden AC . Impaired glucose tolerance and fasting hyperglycaemia have different characteristics Diabetic Med 2000 17: 433–440.
Gimeno SGA, Ferreira SRG, Laercio JF, Iunes M, The Japanese Brazilian Diabetes Study Group. Comparison of glucose tolerance categories according to World Health Organization and American Diabetes Association diagnostic criteria in a population-based study in Brazil Diabetes Care 1998 21: 1889–1892.
The DECODE Study Group: glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria . Lancet 1999 354: 617–621.
Tripathy D, Carlsson M, Almgren P, Isomaa B, Taskinen M-R, Tuomi T, Groop LC . Insulin secretion and insulin sensitivity in relation to glucose tolerance. Lessons from the Botnia study Diabetes 2000 49: 975–980.
Stumvoli M, Mitakou A, Pimenta W, Jenseen T, Yki-Jarvinen H, Van Haeften T, Renn W, Gerich J . Use of oral glucose tolerance test to assess insulin release and insulin sensitivity Diabetes Care 2000 23: 295–301.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and β-cell function from plasma fasting glucose and insulin concentrations in man Diabetologia 1985 28: 412–419.
Matsuda M, de Fronzo RA . Insulin sensitivity indices obtained from oral glucose tolerance testing Diabetes Care 1999 22: 1462–1470.
Cederholm J, Wibell L . Insulin release and peripheral sensitivity at the oral glucose tolerance test Diabetes Res Clin Pract 1990 10: 167–175.
Bonora E, Targher G, Alberriche M, Bonadonna RCM, Saggiani F, Zenere MB, Monauni T, Muggeo M . Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity Diabetes Care 2000 23: 57–63.
de Fronzo R, Tobin JD, Andres R . Glucose clamp technique: a method for quantifying insulin secretion and resistance Am J Physiol 1979 237: 214–223.
de Fronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes . Diabetes Rev 1997 3: 177–269.
de Fronzo RA, Ferrannini E, Simonson DC . Fasting hyperglycemia in non-insulin dependent diabetes mellitus: contributions of excessive hepatic glucose production and impaired tissue glucose uptake Metabolism 1989 38: 387–395.
Katz LD, Glickman MG, Rapoport S, Ferrannini E, de Fronzo RA . Splanchnic and peripheral disposal of oral glucose in man Diabetes 1983 32: 675–679.
Duncan DB . Multiple range test for correlated and heteroscedastic means Biometrics 1957 13: 164–204.
Mannucci E, Bardini G, Ognibene A, Rotella CM . Comparison of ADA and WHO screening methods for diabetes mellitus in obese patients Diabetic Med 1999 16: 579–585.
Levitt NS, Unwin NC, Bradshaw D, Kitange HM, Mbanya J-CN, Mollentze WF, Omar MAK, Motala AA, Joubert G, Masuki G, Machibya H . Application of the new ADA criteria for the diagnosis of diabetes to populations studies in sub-Saharan Africa Diabetic Med 2000 17: 381–385.
Dinneen SF, Maldonado D III, Leibson CL, Klee GG, Li H, Melton LJ III, Rizza RA . Effects of changing diagnostic criteria on the risk of developing diabetes Diabetes Care 1998 21: 1408–1413.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Melchionda, N., Forlani, G., Marchesini, G. et al. WHO and ADA criteria for the diagnosis of diabetes mellitus in relation to body mass index. Insulin sensitivity and secretion in resulting subcategories of glucose tolerance. Int J Obes 26, 90–96 (2002). https://doi.org/10.1038/sj.ijo.0801847
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801847
Keywords
This article is cited by
-
The Effect of a Silybin-Vitamin E-Phospholipid Complex on Nonalcoholic Fatty Liver Disease: A Pilot Study
Digestive Diseases and Sciences (2007)
-
Pleiotropic Effects of Genes for Insulin Resistance on Adiposity in Baboons
Obesity Research (2004)