Abstract
A major difficulty in the treatment of cancers is the poor response of many tumors to pharmacological regimens. This situation can be accounted for by the existence of a variety of complex mechanisms of chemoresistance (MOCs), leading to reduced intracellular concentrations of active agents, changes in the molecular targets of the drugs, enhanced repair of drug-induced modifications in macromolecules, stimulation of anti-apoptotic mechanisms, and inhibition of pro-apoptotic mechanisms. The present review focuses on alterations in the expression and appearance of the genetic variants that affect the genes involved in reducing the amount of active agents inside tumor cells. These alterations can occur through two mechanisms: either by lowering uptake or enhancing efflux (so-called MOC-1a and MOC-1b, respectively), or by decreasing the activation of prodrugs or enhancing inactivation of active agents through their biotransformation (MOC-2). The development of chemosensitizers that are useful in implementing the pharmacological manipulation of these processes constitutes a challenge to modern pharmacology. Nevertheless, the important physiological roles of the most relevant genes involved in MOC-1a, MOC-1b, and MOC-2 make it difficult to prevent the side effects of chemosensitizers. A more attainable goal in this area of pharmacological enquiry is the identification of proteomic profiles that will permit oncologists to accurately predict a lack of response to a given regimen, which would be useful for adapting treatment to the personal situation of each patient.
Similar content being viewed by others
Introduction
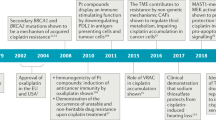
One of the main problems in the treatment of cancer is the poor response of many tumors to the pharmacological regimen imposed. This situation can be explained by the existence of a variety of complex mechanisms of chemoresistance (MOCs), which lead to reduced intracellular concentrations of active agents, changes in the molecular targets of the drugs, and enhanced repair of drug-induced modifications in macromolecules; additionally, anti-apoptotic mechanisms are stimulated, whereas pro-apoptotic mechanisms are inhibited. Here, we review the MOCs that involve changes in the expression level and appearance of the genetic variants that affect the genes involved in i) drug uptake or efflux (so-called MOC-1a and MOC-1b, respectively)1 of the genes encoding the proteins that belong to the “transportome”, which is a group of expressed transporters that govern the traffic across the plasma membrane of tumor cells, and ii) activation of prodrugs or inactivation of already active agents through their biotransformation (MOC-2)1 (Figure 1). Together, these events form an important group of MOCs, as the mechanism of action of many anticancer agents occurs inside cells, either by inhibiting the key processes required for tumor cell survival or interacting in non-tumor cells with the signaling pathways involved in cancer development, such as those responsible for angiogenesis.
Schematic representation of the genes involved in chemoresistance due to a reduction in the intracellular concentrations of anticancer drugs via reduced uptake or enhanced efflux and by a lower activation of prodrugs and enhanced inactivation of anticancer agents.
MOC-1a
Reduced expression of genes involved in drug uptake
The uptake of most anticancer agents occurs via plasma membrane transporters belonging to the Solute Carrier Family (SLC)2. The natural substrates of these transporters include a large variety of endogenous or xenobiotic compounds. Many drugs use these transporters to enter cells because they have structural characteristics that are similar to those of the endogenous substrates3. Down-regulation or the expression of less functional variants of SLC proteins in tumor cells may impair drug uptake, reduce the intracellular concentration of the active agent, and, as a consequence, hinder the efficacy of chemotherapy (Table 1).
Organic anion-transporting polypeptides (OATPs) are plasma membrane transporters encoded by SLCO genes and are able to transport a large variety of endogenous compounds and drugs4. OATP1B1 and OATP1B3, encoded by the SLCO1B1 and SLCO1B3 genes, respectively, are able to transport such anticancer drugs as flavopiridol, methotrexate, paclitaxel, irinotecan, tyrosine kinase inhibitors5, and cisplatin-conjugated bile acid derivatives6. A reduction in OATP1B1 and OATP1B3 expression or their functionality appears to result in a lower accumulation of antitumor drugs in liver cancer7. Indeed, a decrease in the expression of these proteins in hepatocellular carcinoma (HCC) and cholangiocarcinoma (CGC) has been described8. The expression of another member of the OATP family, OATP1A2 (SLCO1A2), is markedly reduced in both polyps of the large intestine and colon cancer compared to a healthy colon9. Furthermore, alterations in the expression level or functionality of OATP1A2 have been associated with the development of resistance to methotrexate10 and imatinib11.
The human SLC22A family includes organic cation transporters (OCTs), Na+-zwitterion/cation cotransporters (OCTNs), and a heterogeneous group of transporters that can transport organic anions (OATs)12. The organic cation transporter-1 (OCT1, the SLC22A1 gene) is one of the transporters involved in the uptake of tyrosine kinase inhibitors, such as sorafenib13, and other important cationic antitumor drugs, such as platinum derivatives and anthracyclines14. Thus, tumor response to these drugs depends in part on OCT1 expression. We have recently described that primary liver cancer, ie, HCC, CGC, and hepatoblastoma, share decreased expression of OCT1 as a common feature8; OCT1 expression is also reduced in colon cancer9. In HCC15 and CGC patients16, low OCT1 expression has been associated with advanced tumor stages and poorer overall survival rates, and hypermethylation of the SLC22A1 promoter has been proposed as a mechanism for the down-regulation of OCT1 in HCC15. Moreover, imatinib uptake in chronic myeloid leukemia (CML) primary cells and cell lines has been shown to be dependent on OCT1 expression17, and the degree of OCT1 expression has been suggested to be a useful biomarker for predicting the success of imatinib-based therapy in leukemia patients18.
The SLC28 and SLC29 families include high-affinity concentrative nucleoside transporters (CNTs) and low-affinity equilibrative nucleoside transporters (ENTs), which are involved in the uptake of nucleoside-derived anticancer drugs, such as gemcitabine, floxuridine, and cytarabine19. Changes in the expression of these transporters account for the differential uptake of nucleoside derivatives by tumors, and this may significantly modulate intracellular drug bioavailability and hence responsiveness to therapy19,20.
Copper is an essential micronutrient, and uptake by human cells is mainly performed by the high-affinity copper transporter CTR1, which is encoded by the SLC31A1 gene. The expression of this transporter is regulated by the transcription factor Sp1, which acts as a copper sensor21. Recent research has revealed that CTR1 can also transport platinum drugs, underscoring the important role of CTR1 in platinum-drug sensitivity in cancer chemotherapy. Elevated CTR1 expression has consistently been associated with favorable treatment outcomes in cisplatin-based cancer chemotherapy, although down-regulation of CTR1 has been observed when tumor cells are exposed to this agent22. Because CTR1 expression can be induced through the depletion of cellular copper levels, which results in enhanced cisplatin uptake, a phase I clinical trial using a combination of trientine (a copper chelator) and carboplatin has been conducted, with encouraging results (for a review, see21).
Less functional variants of proteins involved in drug uptake
In addition to differences in the expression pattern of SLC proteins in tumors, the presence of of SLC protein variants is responsible for the considerable inter-individual variation in the efficiency of antitumor drugs23 and also contributes to MOC-1a24. This section offers an overview of the transporter variants that are clinically relevant in the pharmacological treatment of cancer.
The reduced folate carrier (RFC, SLC19A1), which is ubiquitously expressed in human tissues, is involved in the uptake of endogenous folate and antifolate drugs, such as methotrexate and pemetrexed. SLC19A1 genetic variants have been associated with a variable response to methotrexate in several types of cancer25, and the common missense variant His27Arg (c.80A>G) has been investigated for its effect on methotrexate response and toxicity. In children with acute lymphoblastic leukemia (ALL) treated with methotrexate, the presence of the wild-type variant was associated with a 50% better chance of staying in remission than the GG or GA variant25. Polymorphisms in the SLC1A91 gene can also be predictive of survival differences in advanced non-small cell lung carcinoma (NSCLC) patients treated with pemetrexed-based chemotherapy26.
Resistance is a major cause of imatinib treatment failure in CML patients. Because imatinib uptake is mainly performed by OCT1, the SLC22A1 genotype of CML patients can be used to predict the outcome of imatinib treatment. Thus, patients harboring the wild-type GG genotype of the common variant Leu160Phe (c.480G>C) have a higher rate of treatment failure to imatinib therapy than patients with the mutation27. Moreover, the Met420del variant (c.1258_1260delATG) may alter imatinib pharmacodynamics, resulting in a reduction in drug efficacy in the targeted leukemia cells28.
Similar results have been found for sorafenib in the treatment of liver cancer. The results of a recent study performed by our group suggest that liver carcinogenesis is accompanied by the appearance of aberrant variants of OCT1 that may dramatically affect the ability of HCC and CGC to take up and hence respond to sorafenib13. In addition, the existence of inactivating SNPs in the SLC22A1 gene in HCC and CGC may affect the response of these tumors to treatment with sorafenib13. The expression of non-functional truncated OCT1 isoforms originating through alternative splicing mechanisms, such as exon skipping and intron retention, has also been found in tumor cells13,29.
MOC-1b
Increased expression of genes involved in drug efflux
Most genes involved in MOC-1b encode export pumps belonging to the ABC (ATP-binding cassette) superfamily. The over-expression of some members of this superfamily in tumor cells, particularly those of the ABCB, ABCC, and ABCG families, is one of the major problems in chemotherapy resistance because of their role in the so-called multidrug resistance (MDR) phenotype6. These membrane transporters use energy derived directly from the hydrolysis of ATP to export a large variety of compounds, including antitumor drugs, from inside the cell, thereby reducing their intracellular concentrations. The expression of ABC proteins can be increased as part of the cellular response to the chemical stress induced by compounds that are structurally very different. Even compounds that are not substrates of these transporters have been found to increase the levels of some ABC proteins in tumor cells30.
The ABCB family includes the prototype of MDR proteins, ie, MDR1 (gene symbol ABCB1), also known as P-glycoprotein. This pump is broadly expressed in epithelia and is able to transport a large variety of anticancer drugs30. MDR1 is also involved in conferring the MDR phenotype to many types of cancer cells that have developed resistance to anticancer drugs. For example, high ABCB1 expression has been associated with a poor response of HCC31 and hepatoblastoma32 to pharmacological treatments.
Several members of the ABCC family involved in chemoresistance are typically designated multidrug resistance-associated proteins (MRPs). Among them, the most important with regard to drug refractoriness and the development of chemoresistance in human tumors are MRP1 (ABCC1), MRP2 (ABCC2), MRP3 (ABCC3), and MRP4 (ABCC4)6. Indeed, a clear relationship between MRP1 and the resistance to many antineoplastic agents, such as doxorubicin and vincristine, has been established based on studies using tumor cell lines33. MRP2 plays an important role in the resistance to platinum derivatives, presumably because this protein is able to efficiently export glutathione conjugates of cisplatin, and a markedly increased expression of MRP2 has been found in colon cancer cells after exposure to cisplatin34. MRP2 is mainly detected in the membrane of HCC tumor cells, and this localization has been associated with the refractoriness of HCC to chemotherapy that is due to reduced drug accumulation in these cells6. Over-expression of MRP2 is considered to be one of the most important mechanisms accounting for the failure of cisplatin treatment in colon cancer35, whereas MRP3 expression in CGC has been suggested to contribute to the intrinsic MDR phenotype characteristic of this type of cancer36. MRP4 expression has been found to be increased by more than 10-fold when cisplatin resistance was induced in cell lines derived from HCC37.
The ABCG gene family includes an important transporter that is responsible for the failure of chemotherapy in many tumors: ABCG2, which is also known as breast cancer resistance protein (BCRP). ABCG2 expression may be a selective marker for the efficacy of chemotherapeutic regimens in treating some types of cancer, such as colorectal carcinoma38, and esophageal squamous carcinoma39. ABCG2 over-expression in response to anticancer drug exposure has also been observed. ABCG2 was found to be markedly upregulated in a study in which the expression of a broad panel of both ABC and SLC transporters were measured in an ovarian cancer cell line compared to MDR sublines40. Similarly, increased ABCG2 expression has been found in colon cancer cells after exposure to cisplatin34. IMP3, a member of a family of insulin-like growth factor II (IGF-II) mRNA-binding proteins (IMPs), is preferentially expressed in triple-negative breast cancers, which are resistant to many chemotherapeutics. The IMP3 protein has also been reported to promote chemoresistance in breast cancer cells by regulating ABCG2 expression41. Owing to the clinical relevance of ABCG2 in the multidrug resistance phenomenon, ABCG2 constitutes an appealing therapeutic target to increase drug distribution. The development of ABCG2 inhibitors, which can be used in combination with anticancer drugs to block drug efflux from cancer cells, has recently emerged42.
Non-ABC transporters are also involved in drug efflux and have therefore been included in MOC-1b. Thus, the ATP7A and ATP7B genes that encode the copper-transporting P-type ATPases Menkes and Wilson proteins, respectively, are involved in regulating the copper status of the body43. However, in cancer cells, these primary active transporters also account for a reduction in the intracellular concentrations of several antitumor agents, such as cisplatin. Accordingly, ATP7B has been found to be over-expressed in tumors with marked resistance to platinum-based chemotherapy44.
Lung resistance-related protein (LRP) or major vault protein (MVP) is not a pump but plays a similar role in chemoresistance because it forms cytoplasmic nano-organelles, the vaults, which are able to encapsulate anticancer drugs and hence reduce their active intracellular concentrations. In tumors, an inverse relationship between MVP expression and the degree of response to anticancer agents has been reported45,46.
Genetic variants in genes involved in drug efflux
Most SNPs described in ABC genes do not contribute to MOC-1b because many of them affect the mRNA stability of the variant transcript, resulting in lower protein levels, or alter residues that are important for the structure of the protein, thereby impairing transport activity. Nevertheless, the presence of certain SNPs in the 5′ flanking region of ABC genes can increase their expression in tumor cells, accounting for enhanced resistance to antitumor drugs. Moreover, genetic variants in MOC-1b genes might result in an increased transport ability of the proteins and hence a reduced intracellular active drug concentration24.
To date, more than 50 SNPs have been identified in ABCB1, and changes in protein (MDR1) structure and function that are due to altered protein folding have been suggested as a possible consequence of these mutations47. Some SNPs have been reported to affect either the substrate specificity of MDR1 and/or increase its transport activity, which in turn enhances drug refractoriness in tumor cells expressing these variants. The identification of SNPs in ABCB1 has been proposed as a valuable marker for the outcome of the chemotherapeutic treatment of several types of tumors48,49,50. The MDR1 variant Ser400Asn (c.1199G>A) in patients with ovarian cancer has been associated with a higher likelihood of failure of treatment with paclitaxel plus carboplatin51. Although c.1236C>T in ABCB1 is a synonymous SNP (p.Gly412Gly), it may result in higher MDR1 expression levels, and its presence in CML patients has been associated with a higher resistance to imatinib52. Other ABCB1 genetic variants involved in the drug refractoriness of tumor cells are c.2677G>T/A (p.Ala893Ser/Thr) and c.3435C>T (p.Ile1145Ile). The presence of these variants has been related to increased resistance to irinotecan53 and platinum-derived compounds54 in advanced NSCLC, to imatinib in CML52, and to 5-fluorouracil plus leucovorin in colorectal cancer55. Additionally, the 1236T/2677G/3435C haplotype has been found more frequently in patients with resistance to imatinib56.
High MRP1 expression in cancer is characteristic of the MDR phenotype57. The c.-1666G>A SNP in ABCC1 impairs promoter activity, and HCC patients bearing the wild-type -1666GG genotype have a poor outcome and survival rate58.
The most frequent SNPs in ABCC2 are c.-24C>T, c.1249G>A (p.Val417Ile), and c.3972C>T (p.Ile1324Ile). The presence of c.-24C>T has been related to an increased platinum-based chemotherapy response in NSCLC59; furthermore, this SNP has also been related to higher methotrexate plasma concentrations in childhood ALL due to a lower MRP2 activity60. An association between the c.3972C>T variant and the risk of CGC has also been found61. Moreover, the haplotype consisting of both c.-24C>T and c.3972C>T SNPs has been related to an enhanced sensitivity to irinotecan therapy in advanced NSCLC53.
Enhanced MRP3 expression has been associated with a lower remission rate and decreased survival in leukemias62,63. Because the c.-211C>T SNP in the ABCC3 gene reduces MRP3 expression levels64, the wild-type CC genotype has been associated with a poor prognosis in daunorubicin-treated ALL patients65. However, in this respect, controversial results have been found because the presence of the c.-211T mutant allele has been associated with significantly reduced progression-free survival in lung cancer patients treated with etoposide66. The c.-189A>T SNP has also been proposed as a marker of clinical outcome in childhood ALL patients, whereas it has been reported that methotrexate-treated patients bearing the wild-type AA allele, which results in enhanced ABCC3 promoter activity, have reduced survival outcomes62.
The prognostic usefulness of ABCC4 SNPs in childhood ALL has also been reported. Because the c.-1393T>C SNP results in higher ABCC4 promoter activity, the methotrexate and 6-mercaptopurine plasma levels in ALL patients are lower than in those bearing the wild-type genotype67.
More than 80 ABCG2 genetic variants have been described. Among them, Gln141Lys (c.421C>A) is one of the most extensively studied and results in reduced protein expression and increased sensitivity to many anticancer drugs68. For example, the presence of this polymorphism confers higher sensitivity to tyrosine kinase inhibitors69 and camptothecins70. In contrast, this ABCG2 variant has recently been associated with a poor prognosis in acute myeloid leukemia (AML) patients treated with idarubicin71.
The Arg482Gly (c.1444A>G) and Arg482Thr (c.1445G>C) variants result in higher sensitivity to topotecan but enhanced resistance to anthracyclines and rhodamine-123. These variants have been found during the course of drug-induced selection and have been shown to be responsible for differential drug efflux and sensitivity72.
MOC-2
Reduced intracellular activation of prodrugs
The detoxification processes occurring in both tumor and healthy cells include oxidation/reduction reactions by phase I enzymes, such as cytochrome P450 (CYP)-related enzymes, and conjugation with polyatomic groups by phase II enzymes, such as those involved in glucuronic acid, sulfate, and glutathione conjugation. Changes in the expression or function of these enzymes that are due to the appearance of variants in the genes involved in drug biotransformation in cancer cells may dramatically affect the final success of pharmacological treatment73. Thus, on the one hand, the enhanced activity of phase I and phase II enzymes may result in the inactivation of drugs and enhanced chemoresistance; on the other hand, several anticancer agents are administered as inactive prodrugs and hence require metabolic activation by phase I proteins. Accordingly, reduced sensitivity to these drugs may be due to the reduced expression or function of the enzymes. In summary, alterations in drug metabolism that are due either to an enhanced production of inactive metabolites or a reduced activation of prodrugs (MOC-2) may decrease the intracellular concentrations of the active agent, reducing the efficacy of chemotherapy6.
For instance, 5-fluorouracil activation involves three enzymatic activities: thymidine phosphorylase (TYMP), uridine phosphorylase (UPP), and orotate phosphoribosyl transferase (OPRT). The reduced expression or impaired activity of these enzymes in tumors has been associated with a lower sensitivity to 5-fluorouracil74. Similarly, irinotecan must be converted by carboxylesterases (CESs) into SN-38, which is an active inhibitor of topoisomerase I. The mRNA levels of these enzymes are consistently reduced in irinotecan-resistant colorectal carcinomas75. One of the mechanisms accounting for the resistance to methotrexate derivatives is a reduction in folylpolyglutamate synthase (FPGS) activity, the role of which is to enhance the affinity of the drug for its molecular target76.
CYP belongs to a large group of more than 60 enzymes that are responsible for the activation or inactivation of most clinically important drugs, including those used against cancer. The human CYP genes are highly polymorphic, yet to date only certain genetic variants have been demonstrated to be clinically relevant.
CYP2A6 activates tegafur to generate 5-fluorouracil, and one study reported that the poor response to tegafur by a patient with gastric cancer was caused by a poor metabolic phenotype due to mutations in the CYP2A6 gene. The presence of the Ser224Pro variant (c.670T>C, CYP2A6*11), which has a very low metabolizing capacity, along with the deletion of one of the alleles of the CYP2A6 gene (also known as the CYP2A6*4C allele) were found in this patient77.
CYP2C19 is involved in thalidomide and cyclophosphamide activation. Two variants resulting in the synthesis of non-functional truncated proteins, Ile215_Pro227del fs*20 or CYP2C19*2 (c.681G>A, which results in an aberrant splicing of exon 5) and Trp212X or CYP2C19*3 (c.636G>A), have been associated with a lack of response to thalidomide in patients with multiple myeloma78,79. The CYP2C19*2 variant has also been associated with lower drug efficacy in cyclophosphamide-treated patients as a result of inefficient activation of the prodrug80.
CYP2D6 metabolizes tamoxifen to produce active 4-hydroxytamoxifen and endoxifen. More than 80 genetic variants encoding non-functional CYP2D6 or an enzyme with reduced activity have been described, and tamoxifen-treated breast cancer patients harboring these variants are at a greater risk of cancer relapse81. The most common variants in the Caucasian population are CYP2D6*3 (c.2549delA in exon 5), CYP2D6*4 (1846G>A in intron 3), CYP2D6*5 (deleted gene), and CYP2D6*6 (c.1707delT in exon 3)82.
Enhanced drug inactivation
Dihydropyrimidine dehydrogenase (DPYD) inactivates fluoropyrimidines, such as 5-fluorouracil; therefore, changes in DPYD activity affect the overall exposure of tumor cells to these drugs. Among the 39 genetic variants identified in the human DPYD gene, the most frequent is an intronic mutation that leads to exon-14 skipping (c.IVS14+1G>A). This alteration is associated with decreased DPYD activity and hence an increased risk of developing severe or fatal side effects during treatment with 5-fluorouracil or its prodrugs capecitabine and tegafur83.
NAD(P)H quinone oxidoreductase 1 (NQO1) catalyzes the reduction of quinines and nitro derivatives using NADP or NADPH as a cofactor. A lower survival of women with breast carcinoma harboring the Pro187Ser variant (c.558C>T; NQO1*2) after treatment with anthracycline-based adjuvant chemotherapy with epirubicin has been reported84.
Glutathione S-transferases (GSTs) form a superfamily of enzymes that play an important role in the detoxification of a broad variety of hydrophobic and electrophilic compounds through conjugation with reduced glutathione, a modification that inactivates the drugs and/or increases their water solubility, thus favoring their elimination from the body85. Accordingly, an enhanced conjugating activity due to GST can determine the degree of resistance to platinum compounds86, and the cellular content of glutathione is a key factor in this mechanism of resistance. Indeed, the amount of intracellular glutathione and the expression of the enzymes responsible for the synthesis of glutathione determine sensitivity to cisplatin87,88.
Functionally different glutathione S-transferase pi (GSTP1) variant proteins are encoded by a polymorphic gene. These enzymes are able to recognize several anticancer drugs as substrates, such as etoposide, doxorubicin, thioTEPA, cisplatin, oxaliplatin, and carboplatin. The Ile105Val variant, or GSTP1*B, is a non-synonymous SNP (c.313A>G) of special pharmacogenetic relevance and has been associated with anticancer drug responses and toxicity. Indeed, an increase in overall survival was observed in patients with metastatic colorectal cancer bearing the GSTP1*B polymorphism who had been treated with 5-fluorouracil plus oxaliplatin89. It was also reported that children with ALL treated with etoposide displayed different drug clearances, depending on their genotype90.
Uridine disphosphate glucuronosyl transferases (UGTs) catalyze the glucuronidation of xenobiotics and endogenous compounds to form more water-soluble molecules that can be more readily excreted. UGT1A1 is involved in the metabolism of bilirubin and other endogenous compounds. UGT1A1 also mediates the glucuronidation of SN-38, which is secreted into bile91, and also participates in the metabolism of other drugs, such as etoposide, epirubicine, and tyrosine kinase inhibitors. In addition, an increase in UGT1A1 activity may contribute to chemoresistance to irinotecan in colon cancer91.
A TA insertion in the (TA)6TAA promoter region (UGT1A1*28) is the most common genetic variant in the Caucasian population, whereas the Gly71Arg variant, or UGT1A1*6 (c.211G>A), and Pro229Gln, or UGT1A1*27 (c.686C>A), are more frequent in Asian populations. All of these variants are associated with enhanced exposure to SN-38 and higher drug-induced toxicity due to a reduction in SN-38 glucuronidation92,93.
Sulfotransferase 1A1 (SULT1A1) catalyzes the sulfation of the active metabolite of tamoxifen. The most common variant is Arg213His, or SULT1A1*2 (c.638G>A), which has been associated with reduced activity and a three-fold enhanced risk of death in patients with breast cancer treated with tamoxifen94.
The clinical relevance of genetic variants in other drug-metabolizing enzymes, such as carboxylesterase, epoxide hydrolase, cytidine deaminase, deoxycytidine kinase, N-acetyltranferase, thiopurine methyltransferase, and metallothionein, to chemoresistance is considered minor24.
Conclusions and future perspectives
To produce a higher likelihood of success, a better understanding of the molecular bases of MOC is required to tackle one of the major hurdles in the treatment of cancer, ie, the lack of response to available drugs. Indeed, the development of chemosensitizers that are useful for the pharmacological manipulation of MOC is a challenge to modern pharmacology. Nevertheless, the important physiological role of many of the most relevant genes involved in MOC-1a, MOC-1b, and MOC-2, creates difficulty in avoiding the side effects of chemosensitizers. Another goal in this area of pharmacological research that has a higher chance of success in the near future is the identification of proteomic profiles. Such data may allow oncologists to accurately predict the lack of response to a given pharmacological regimen, which would be useful for adapting treatments to the personal situation of each patient.
Financial support
Supported in part by the Junta de Castilla y Leon (grants SA023A11-2, SA070A11-2 and Biomedicina-2011), Spain, the Ministerio de Ciencia e Innovación (grant SAF2010-15517), Spain, and the Instituto de Salud Carlos III, FIS (grant PI11/0337). The group is a member of the Network for Cooperative Research on Membrane Transport Proteins (REIT), co-funded by the Ministerio de Educación y Ciencia, Spain, and the European Regional Development Fund (ERDF) (grant BFU2007-30688-E/BFI), and belongs to the CIBERehd (Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas), Instituto de Salud Carlos III, Spain.
Abbreviations
AML, acute myeloid leukemia; ALL, acute lymphoblastic leukemia; ABC, ATP-binding cassette; BCRP, breast cancer resistance protein; CES, carboxylesterase; CML, chronic myeloid leukemia; HCC, hepatocellular carcinoma; CGC, cholangiocarcinoma; CYP, cytochrome P-450; DPD, dihydropyrimidine dehydrogenase; GST, glutathione S-transferase; LRP/MVP, lung resistance-related protein or major vault protein; MDR, multidrug resistance; MOC, mechanism of chemoresistance; MRP, multidrug resistance-associated protein; NSCLC, non-small cell lung carcinoma; OATP, organic anion-transporting polypeptide; OCT, organic cation transporter; OPRT, orotate phosphoribosyl transferase; SLC, solute carrier; SNP, single-nucleotide polymorphism; TYMP, thymidine phosphorylase; UGT, uridine disphosphate glucuronosyl transferase; UMPS, uridine monophosphate synthetase; UPP, uridine phosphorylase.
References
Marin JJ, Castano B, Blazquez AG, Rosales R, Efferth T, Monte MJ . Strategies for overcoming chemotherapy resistance in enterohepatic tumours. Curr Mol Med 2010; 10: 467–85.
Hediger MA, Clemencon B, Burrier RE, Bruford EA . The ABCs of membrane transporters in health and disease (SLC series): introduction. Mol Aspects Med 2013; 34: 95–107.
Huang Y, Sadee W . Membrane transporters and channels in chemoresistance and -sensitivity of tumor cells. Cancer Lett 2006; 239: 168–82.
Hagenbuch B, Meier PJ . Organic anion transporting polypeptides of the OATP/SLC21 family: phylogenetic classification as OATP/ SLCO superfamily, new nomenclature and molecular/functional properties. Pflugers Arch 2004; 447: 653–65.
Buxhofer-Ausch V, Secky L, Wlcek K, Svoboda M, Kounnis V, Briasoulis E, et al. Tumor-specific expression of organic anion-transporting polypeptides: transporters as novel targets for cancer therapy. J Drug Deliv 2013; 2013: 863539.
Marin JJ, Romero MR, Briz O . Molecular bases of liver cancer refractoriness to pharmacological treatment. Curr Med Chem 2010; 17: 709–40.
Zollner G, Wagner M, Fickert P, Silbert D, Fuchsbichler A, Zatloukal K, et al. Hepatobiliary transporter expression in human hepatocellular carcinoma. Liver Int 2005; 25: 367–79.
Martinez-Becerra P, Vaquero J, Romero MR, Lozano E, Anadon C, Macias RI, et al. No correlation between the expression of FXR and genes involved in multidrug resistance phenotype of primary liver tumors. Mol Pharm 2012; 9: 1693–704.
Ballestero MR, Monte MJ, Briz O, Jimenez F, Gonzalez-San Martin F, Marin JJ . Expression of transporters potentially involved in the targeting of cytostatic bile acid derivatives to colon cancer and polyps. Biochem Pharmacol 2006; 72: 729–38.
Badagnani I, Castro RA, Taylor TR, Brett CM, Huang CC, Stryke D, et al. Interaction of methotrexate with organic-anion transporting polypeptide 1A2 and its genetic variants. J Pharmacol Exp Ther 2006; 318: 521–9.
Yamakawa Y, Hamada A, Shuto T, Yuki M, Uchida T, Kai H, et al. Pharmacokinetic impact of SLCO1A2 polymorphisms on imatinib disposition in patients with chronic myeloid leukemia. Clin Pharmacol Ther 2011; 90: 157–63.
Koepsell H, Endou H . The SLC22 drug transporter family. Pflugers Arch 2004; 447: 666–76.
Herraez E, Lozano E, Macias RI, Vaquero J, Bujanda L, Banales JM, et al. The expression of SLC22A1 variants may affect the response of hepatocellular carcinoma and cholangiocarcinoma to sorafenib. Hepatology 2013; 58: 1065–73.
Koepsell H, Lips K, Volk C . Polyspecific organic cation transporters: structure, function, physiological roles, and biopharmaceutical implications. Pharm Res 2007; 24: 1227–51.
Schaeffeler E, Hellerbrand C, Nies AT, Winter S, Kruck S, Hofmann U, et al. DNA methylation is associated with downregulation of the organic cation transporter OCT1 (SLC22A1) in human hepatocellular carcinoma. Genome Med 2011; 3: 82.
Lautem A, Heise M, Grasel A, Hoppe-Lotichius M, Weiler N, Foltys D, et al. Downregulation of organic cation transporter 1 (SLC22A1) is associated with tumor progression and reduced patient survival in human cholangiocellular carcinoma. Int J Oncol 2013; 42: 1297–304.
Thomas J, Wang L, Clark RE, Pirmohamed M . Active transport of imatinib into and out of cells: implications for drug resistance. Blood 2004; 104: 3739–45.
Wang L, Giannoudis A, Lane S, Williamson P, Pirmohamed M, Clark RE . Expression of the uptake drug transporter hOCT1 is an important clinical determinant of the response to imatinib in chronic myeloid leukemia. Clin Pharmacol Ther 2008; 83: 258–64.
Pastor-Anglada M, Molina–Arcas M, Casado FJ, Bellosillo B, Colomer D, Gil J . Nucleoside transporters in chronic lymphocytic leukaemia. Leukemia 2004; 18: 385–93.
Hung SW, Mody HR, Govindarajan R . Overcoming nucleoside analog chemoresistance of pancreatic cancer: a therapeutic challenge. Cancer Lett 2012; 320: 138–49.
Kuo MT, Fu S, Savaraj N, Chen HH . Role of the human high-affinity copper transporter in copper homeostasis regulation and cisplatin sensitivity in cancer chemotherapy. Cancer Res 2012; 72: 4616–21.
Holzer AK, Katano K, Klomp LW, Howell SB . Cisplatin rapidly down-regulates its own influx transporter hCTR1 in cultured human ovarian carcinoma cells. Clin Cancer Res 2004; 10: 6744–9.
Leabman MK, Huang CC, DeYoung J, Carlson EJ, Taylor TR, de la Cruz M, et al. Natural variation in human membrane transporter genes reveals evolutionary and functional constraints. Proc Natl Acad Sci U S A 2003; 100: 5896–901.
Marin JJ, Briz O, Monte MJ, Blazquez AG, Macias RI . Genetic variants in genes involved in mechanisms of chemoresistance to anticancer drugs. Curr Cancer Drug Targets 2012; 12: 402–38.
Gregers J, Christensen IJ, Dalhoff K, Lausen B, Schroeder H, Rosthoej S, et al. The association of reduced folate carrier 80G>A polymorphism to outcome in childhood acute lymphoblastic leukemia interacts with chromosome 21 copy number. Blood 2010; 115: 4671–7.
Li WJ, Jiang H, Fang XJ, Ye HL, Liu MH, Liu YW, et al. Polymorphisms in thymidylate synthase and reduced folate carrier (SLC19A1) genes predict survival outcome in advanced non-small cell lung cancer patients treated with pemetrexed-based chemotherapy. Oncol Lett 2013; 5: 1165–70.
Kim DH, Sriharsha L, Xu W, Kamel-Reid S, Liu X, Siminovitch K, et al. Clinical relevance of a pharmacogenetic approach using multiple candidate genes to predict response and resistance to imatinib therapy in chronic myeloid leukemia. Clin Cancer Res 2009; 15: 4750–8.
Giannoudis A, Wang L, Jorgensen AL, Xinarianos G, Davies A, Pushpakom S, et al. The hOCT1 SNPs M420del and M408V alter imatinib uptake and M420del modifies clinical outcome in imatinib-treated chronic myeloid leukemia. Blood 2013; 121: 628–37.
Hayer M, Bonisch H, Bruss M . Molecular cloning, functional characterization and genomic organization of four alternatively spliced isoforms of the human organic cation transporter 1 (hOCT1/SLC22A1). Ann Hum Genet 1999; 63: 473–82.
Marin JJ, Briz O, Perez MJ, Romero MR, Monte MJ . Hepatobiliary transporters in the pharmacology and toxicology of anticancer drugs. Front Biosci (Landmark Ed) 2009; 14: 4257–80.
Ng IO, Liu CL, Fan ST, Ng M . Expression of P-glycoprotein in hepatocellular carcinoma. A determinant of chemotherapy response. Am J Clin Pathol 2000; 113: 355–63.
Minemura M, Tanimura H, Tabor E . Overexpression of multidrug resistance genes MDR1 and cMOAT in human hepatocellular carcinoma and hepatoblastoma cell lines. Int J Oncol 1999; 15: 559–63.
Grant CE, Valdimarsson G, Hipfner DR, Almquist KC, Cole SP, Deeley RG . Overexpression of multidrug resistance-associated protein (MRP) increases resistance to natural product drugs. Cancer Res 1994; 54: 357–61.
Herraez E, Gonzalez-Sanchez E, Vaquero J, Romero MR, Serrano MA, Marin JJ, et al. Cisplatin-induced chemoresistance in colon cancer cells involves FXR–dependent and FXR-independent up–regulation of ABC proteins. Mol Pharm 2012; 9: 2565–76.
Hinoshita E, Uchiumi T, Taguchi K, Kinukawa N, Tsuneyoshi M, Maehara Y, et al. Increased expression of an ATP-binding cassette superfamily transporter, multidrug resistance protein 2, in human colorectal carcinomas. Clin Cancer Res 2000; 6: 2401–7.
Rau S, Autschbach F, Riedel HD, Konig J, Kulaksiz H, Stiehl A, et al. Expression of the multidrug resistance proteins MRP2 and MRP3 in human cholangiocellular carcinomas. Eur J Clin Invest 2008; 38: 134–42.
Wakamatsu T, Nakahashi Y, Hachimine D, Seki T, Okazaki K . The combination of glycyrrhizin and lamivudine can reverse the cisplatin resistance in hepatocellular carcinoma cells through inhibition of multidrug resistance-associated proteins. Int J Oncol 2007; 31: 1465–72.
Lin PC, Lin HH, Lin JK, Lin CC, Yang SH, Li AF, et al. Expression of ABCG2 associated with tumor response in metastatic colorectal cancer patients receiving first-line FOLFOX therapy-preliminary evidence. Int J Biol Markers 2013; 28: 182–6.
Tsunoda S, Okumura T, Ito T, Kondo K, Ortiz C, Tanaka E, et al. ABCG2 expression is an independent unfavorable prognostic factor in esophageal squamous cell carcinoma. Oncology 2006; 71: 251–8.
Januchowski R, Zawierucha P, Andrzejewska M, Rucinski M, Zabel M . Microarray-based detection and expression analysis of ABC and SLC transporters in drug-resistant ovarian cancer cell lines. Biomed Pharmacother 2013; 67: 240–5.
Samanta S, Pursell B, Mercurio AM . IMP3 protein promotes chemoresistance in breast cancer cells by regulating breast cancer resistance protein (ABCG2) expression. J Biol Chem 2013; 288: 12569–73.
Lecerf-Schmidt F, Peres B, Valdameri G, Gauthier C, Winter E, Payen L, et al. ABCG2: recent discovery of potent and highly selective inhibitors. Future Med Chem 2013; 5: 1037–45.
La Fontaine S, Ackland ML, Mercer JF . Mammalian copper-transporting P-type ATPases, ATP7A and ATP7B: emerging roles. Int J Biochem Cell Biol 2010; 42: 206–9.
Nakayama K, Kanzaki A, Terada K, Mutoh M, Ogawa K, Sugiyama T, et al. Prognostic value of the Cu-transporting ATPase in ovarian carcinoma patients receiving cisplatin-based chemotherapy. Clin Cancer Res 2004; 10: 2804–11.
Steiner E, Holzmann K, Elbling L, Micksche M, Berger W . Cellular functions of vaults and their involvement in multidrug resistance. Curr Drug Targets 2006; 7: 923–34.
Losert A, Lotsch D, Lackner A, Koppensteiner H, Peter-Vorosmarty B, Steiner E, et al. The major vault protein mediates resistance to epidermal growth factor receptor inhibition in human hepatoma cells. Cancer Lett 2012; 319: 164–72.
Fung KL, Gottesman MM . A synonymous polymorphism in a common MDR1 (ABCB1) haplotype shapes protein function. Biochim Biophys Acta 2009; 1794: 860–71.
Buda G, Ricci D, Huang CC, Favis R, Cohen N, Zhuang SH, et al. Polymorphisms in the multiple drug resistance protein 1 and in P-glycoprotein 1 are associated with time to event outcomes in patients with advanced multiple myeloma treated with bortezomib and pegylated liposomal doxorubicin. Ann Hematol 2010; 89: 1133–40.
Balcerczak E, Panczyk M, Piaskowski S, Pasz-Walczak G, Salagacka A, Mirowski M . ABCB1/MDR1 gene polymorphisms as a prognostic factor in colorectal cancer. Int J Colorectal Dis 2010; 25: 1167–76.
Campa D, Muller P, Edler L, Knoefel L, Barale R, Heussel CP, et al. A comprehensive study of polymorphisms in ABCB1, ABCC2 and ABCG2 and lung cancer chemotherapy response and prognosis. Int J Cancer 2012; 131: 2920–8.
Green H, Soderkvist P, Rosenberg P, Horvath G, Peterson C . ABCB1 G1199A polymorphism and ovarian cancer response to paclitaxel. J Pharm Sci 2008; 97: 2045–8.
Ni LN, Li JY, Miao KR, Qiao C, Zhang SJ, Qiu HR, et al. Multidrug resistance gene (MDR1) polymorphisms correlate with imatinib response in chronic myeloid leukemia. Med Oncol 2011; 28: 265–9.
Han JY, Lim HS, Yoo YK, Shin ES, Park YH, Lee SY, et al. Associations of ABCB1, ABCC2, and ABCG2 polymorphisms with irinotecan-pharmacokinetics and clinical outcome in patients with advanced non-small cell lung cancer. Cancer 2007; 110: 138–47.
Yin JY, Huang Q, Zhao YC, Zhou HH, Liu ZQ . Meta-analysis on pharmacogenetics of platinum-based chemotherapy in non small cell lung cancer (NSCLC) patients. PloS One 2012; 7: e38150.
Panczyk M, Balcerczak E, Piaskowski S, Jamroziak K, Pasz-Walczak G, Mirowski M . ABCB1 gene polymorphisms and haplotype analysis in colorectal cancer. Int J Colorectal Dis 2009; 24: 895–905.
Maffioli M, Camos M, Gaya A, Hernandez-Boluda JC, Alvarez-Larran A, Domingo A, et al. Correlation between genetic polymorphisms of the hOCT1 and MDR1 genes and the response to imatinib in patients newly diagnosed with chronic-phase chronic myeloid leukemia. Leuk Res 2011; 35: 1014–9.
Mahjoubi F, Golalipour M, Ghavamzadeh A, Alimoghaddam K . Expression of MRP1 gene in acute leukemia. Sao Paulo Med J 2008; 126: 172–9.
Zhao J, Yu BY, Wang DY, Yang JE . Promoter polymorphism of MRP1 associated with reduced survival in hepatocellular carcinoma. World J Gastroenterol 2010; 16: 6104–10.
Sun N, Sun X, Chen B, Cheng H, Feng J, Cheng L, et al. MRP2 and GSTP1 polymorphisms and chemotherapy response in advanced non-small cell lung cancer. Cancer Chemother Pharmacol 2010; 65: 437–46.
Rau T, Erney B, Gores R, Eschenhagen T, Beck J, Langer T . High-dose methotrexate in pediatric acute lymphoblastic leukemia: impact of ABCC2 polymorphisms on plasma concentrations. Clin Pharmacol Ther 2006; 80: 468–76.
Hoblinger A, Grunhage F, Sauerbruch T, Lammert F . Association of the c.3972C>T variant of the multidrug resistance-associated protein 2 gene (MRP2/ABCC2) with susceptibility to bile duct cancer. Digestion 2009; 80: 36–9.
Ansari M, Sauty G, Labuda M, Gagne V, Rousseau J, Moghrabi A, et al. Polymorphism in multidrug resistance-associated protein gene 3 is associated with outcomes in childhood acute lymphoblastic leukemia. Pharmacogenomics J 2012; 12: 386–94.
Benderra Z, Faussat AM, Sayada L, Perrot JY, Tang R, Chaoui D, et al. MRP3, BCRP, and P-glycoprotein activities are prognostic factors in adult acute myeloid leukemia. Clin Cancer Res 2005; 11: 7764–72.
Lang T, Hitzl M, Burk O, Mornhinweg E, Keil A, Kerb R, et al. Genetic polymorphisms in the multidrug resistance-associated protein 3 (ABCC3, MRP3) gene and relationship to its mRNA and protein expression in human liver. Pharmacogenetics 2004; 14: 155–64.
Muller P, Asher N, Heled M, Cohen SB, Risch A, Rund D . Polymorphisms in transporter and phase II metabolism genes as potential modifiers of the predisposition to and treatment outcome of de novo acute myeloid leukemia in Israeli ethnic groups. Leuk Res 2008; 32: 919–29.
Muller PJ, Dally H, Klappenecker CN, Edler L, Jager B, Gerst M, et al. Polymorphisms in ABCG2, ABCC3 and CNT1 genes and their possible impact on chemotherapy outcome of lung cancer patients. Int J Cancer 2009; 124: 1669–74.
Ansari M, Sauty G, Labuda M, Gagne V, Laverdiere C, Moghrabi A, et al. Polymorphisms in multidrug resistance-associated protein gene 4 is associated with outcome in childhood acute lymphoblastic leukemia. Blood 2009; 114: 1383–6.
Imai Y, Nakane M, Kage K, Tsukahara S, Ishikawa E, Tsuruo T, et al. C421A polymorphism in the human breast cancer resistance protein gene is associated with low expression of Q141K protein and low-level drug resistance. Mol Cancer Ther 2002; 1: 611–6.
Mizuno T, Terada T, Kamba T, Fukudo M, Katsura T, Nakamura E, et al. ABCG2 421C>A polymorphism and high exposure of sunitinib in a patient with renal cell carcinoma. Ann Oncol 2010; 21: 1382–3.
Sparreboom A, Loos WJ, Burger H, Sissung TM, Verweij J, Figg WD, et al. Effect of ABCG2 genotype on the oral bioavailability of topotecan. Cancer Biol Ther 2005; 4: 650–8.
Tiribelli M, Fabbro D, Franzoni A, Fanin R, Damante G, Damiani D . Q141K polymorphism of ABCG2 protein is associated with poor prognosis in adult acute myeloid leukemia treated with idarubicin-based chemotherapy. Haematologica 2013; 98: e28–9.
Honjo Y, Hrycyna CA, Yan QW, Medina-Perez WY, Robey RW, van de Laar A, et al. Acquired mutations in the MXR/BCRP/ABCP gene alter substrate specificity in MXR/BCRP/ABCP-overexpressing cells. Cancer Res 2001; 61: 6635–9.
Yu KD, Huang AJ, Fan L, Li WF, Shao ZM . Genetic variants in oxidative stress-related genes predict chemoresistance in primary breast cancer: a prospective observational study and validation. Cancer Res 2012; 72: 408–19.
Evrard A, Cuq P, Ciccolini J, Vian L, Cano JP . Increased cytotoxicity and bystander effect of 5-fluorouracil and 5-deoxy-5-fluorouridine in human colorectal cancer cells transfected with thymidine phosphorylase. Br J Cancer 1999; 80: 1726–33.
Kojima A, Hackett NR, Crystal RG . Reversal of CPT-11 resistance of lung cancer cells by adenovirus-mediated gene transfer of the human carboxylesterase cDNA. Cancer Res 1998; 58: 4368–74.
Barnes MJ, Estlin EJ, Taylor GA, Aherne GW, Hardcastle A, McGuire JJ, et al. Impact of polyglutamation on sensitivity to raltitrexed and methotrexate in relation to drug-induced inhibition of de novo thymidylate and purine biosynthesis in CCRF-CEM cell lines. Clin Cancer Res 1999; 5: 2548–58.
Daigo S, Takahashi Y, Fujieda M, Ariyoshi N, Yamazaki H, Koizumi W, et al. A novel mutant allele of the CYP2A6 gene (CYP2A6*11) found in a cancer patient who showed poor metabolic phenotype towards tegafur. Pharmacogenetics 2002; 12: 299–306.
Li Y, Hou J, Jiang H, Wang D, Fu W, Yuan Z, et al. Polymorphisms of CYP2C19 gene are associated with the efficacy of thalidomide based regimens in multiple myeloma. Haematologica 2007; 92: 1246–9.
Matsuzawa N, Nakamura K, Matsuda M, Ishida F, Ohmori S . Influence of cytochrome P450 2C19 gene variations on pharmacokinetic parameters of thalidomide in Japanese patients. Biol Pharm Bull 2012; 35: 317–20.
Timm R, Kaiser R, Lotsch J, Heider U, Sezer O, Weisz K, et al. Association of cyclophosphamide pharmacokinetics to polymorphic cytochrome P450 2C19. Pharmacogenomics J 2005; 5: 365–73.
Rodriguez-Antona C, Gomez A, Karlgren M, Sim SC, Ingelman-Sundberg M . Molecular genetics and epigenetics of the cytochrome P450 gene family and its relevance for cancer risk and treatment. Hum Genet 2010; 127: 1–17.
Jin Y, Desta Z, Stearns V, Ward B, Ho H, Lee KH, et al. CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 2005; 97: 30–9.
van Kuilenburg AB, Muller EW, Haasjes J, Meinsma R, Zoetekouw L, Waterham HR, et al. Lethal outcome of a patient with a complete dihydropyrimidine dehydrogenase (DPD) deficiency after administration of 5-fluorouracil: frequency of the common IVS14+1G>A mutation causing DPD deficiency. Clin Cancer Res 2001; 7: 1149–53.
Fagerholm R, Hofstetter B, Tommiska J, Aaltonen K, Vrtel R, Syrjakoski K, et al. NAD(P)H:quinone oxidoreductase 1 NQO1*2 genotype (P187S) is a strong prognostic and predictive factor in breast cancer. Nat Genet 2008; 40: 844–53.
Beckett GJ, Hayes JD . Glutathione S-transferases: biomedical applications. Adv Clin Chem 1993; 30: 281–380.
Meijer C, Mulder NH, Timmer-Bosscha H, Sluiter WJ, Meersma GJ, de Vries EG . Relationship of cellular glutathione to the cytotoxicity and resistance of seven platinum compounds. Cancer Res 1992; 52: 6885–9.
Wang H, Li X, Chen T, Wang W, Liu Q, Li H, et al. Mechanisms of verapamil-enhanced chemosensitivity of gallbladder cancer cells to platinum drugs: glutathione reduction and MRP1 downregulation. Oncol Rep 2013; 29: 676–84.
Siddik ZH . Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene 2003; 22: 7265–79.
Stoehlmacher J, Park DJ, Zhang W, Groshen S, Tsao-Wei DD, Yu MC, et al. Association between glutathione S-transferase P1, T1, and M1 genetic polymorphism and survival of patients with metastatic colorectal cancer. J Natl Cancer Inst 2002; 94: 936–42.
Kishi S, Yang W, Boureau B, Morand S, Das S, Chen P, et al. Effects of prednisone and genetic polymorphisms on etoposide disposition in children with acute lymphoblastic leukemia. Blood 2004; 103: 67–72.
Mathijssen RH, van Alphen RJ, Verweij J, Loos WJ, Nooter K, Stoter G, et al. Clinical pharmacokinetics and metabolism of irinotecan (CPT-11). Clin Cancer Res 2001; 7: 2182–94.
Ando Y, Ueoka H, Sugiyama T, Ichiki M, Shimokata K, Hasegawa Y . Polymorphisms of UDP-glucuronosyltransferase and pharmacokinetics of irinotecan. Ther Drug Monit 2002; 24: 111–6.
Ando Y, Fujita K, Sasaki Y, Hasegawa Y . UGT1AI*6 and UGT1A1*27 for individualized irinotecan chemotherapy. Curr Opin Mol Ther 2007; 9: 258–62.
Nowell S, Sweeney C, Winters M, Stone A, Lang NP, Hutchins LF, et al. Association between sulfotransferase 1A1 genotype and survival of breast cancer patients receiving tamoxifen therapy. J Natl Cancer Inst 2002; 94: 1635–40.
Acknowledgements
The revision of the English spelling, grammar, and style of the manuscript by N SKINNER is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Marin, J., Monte, M., Blazquez, A. et al. The role of reduced intracellular concentrations of active drugs in the lack of response to anticancer chemotherapy. Acta Pharmacol Sin 35, 1–10 (2014). https://doi.org/10.1038/aps.2013.131
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2013.131
Keywords
This article is cited by
-
Drug resistance in cancer: mechanisms and tackling strategies
Pharmacological Reports (2020)
-
Oncolytic virus efficiency inhibited growth of tumour cells with multiple drug resistant phenotype in vivo and in vitro
Journal of Translational Medicine (2016)
-
Classification and characteristics of tight oil plays
Petroleum Science (2016)
-
Modulation of the pentose phosphate pathway alters phase I metabolism of testosterone and dextromethorphan in HepG2 cells
Acta Pharmacologica Sinica (2015)