Abstract
The harm associated with high-risk injected opiate use and the threat of the HIV epidemic among injecting drug users has become a worldwide problem. Twenty years ago, in the face of a rapid increase in mortality rates among injecting drug users and the upcoming threat of HIV, the first harm-reduction programs were implemented in the Western world. This paper is a literature review describing four forms of harm reduction currently in use in Europe, North America, and Australia. Each represents a reasonable counterapproach to the threat of increased prevalence of HIV among injecting drug users in transitional and developing countries. The paper attempts to explain the concepts behind the most commonly used types of harm reduction and provides a brief overview of the advantages and disadvantages of each and the reasons for their implementation. The main focus of the review is on the definition and the practical aspects of harm reduction; it includes a brief introduction of Chinese harm-reduction efforts and their implications.
Similar content being viewed by others
Drug abuse and HIV/AIDS epidemiology worldwide
According to 2007 UNAIDS AIDS epidemic data, an estimated 33.2 million people live with HIV/AIDS worldwide; 2.5 million newly infected cases and about 2.1 million deaths from HIV/AIDS were reported in 20071. Injected drug use is a significant factor in the epidemiology of HIV infection. As one example, in Nairobi, 53% of injecting drug users (IDUs; mostly heroin users) test positive for HIV.
The number of IDUs worldwide is estimated to be 13.2 million1; 8.8 million of these live in Eastern Europe or Central, South, or South-East Asia, 1.4 million in North America, and 1 million in Latin America2. Once HIV infection penetrates a given community, it can spread rapidly3. Globally, 10% of the 36.1 million people living with HIV are IDUs. However, only 5% of IDUs have access to HIV-prevention efforts2.
In Eastern Europe and Central Asia, more than 80% of all HIV cases are caused by injected drug use, mainly resulting from the sharing of injection equipment2. Worldwide, the proportion of human papillomavirus infections caused by injecting drug use ranges from 30% to 90%2. The prevalence of IDUs and HIV within a given country can vary considerably. In Western countries, drug use is more common in urban areas, while in countries such as China, it is more common in rural areas. The availability of substances of abuse appears to determine the locations where the drugs are used. In Western countries illegal drugs are much easier to obtain in metropolitan areas, while in some developing countries illegal drug abuse is more common in border areas where illegal drugs are produced and where they can more easily be sold.
Drug-related harm reduction
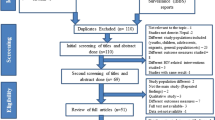
Abstinence and drug-free treatment are extremely desirable goals, but are difficult to attain in the case of opioid dependence, which is considered a chronic relapsing disease. The development of harm reduction is an ongoing process designed to face the problems and harms associated with illegal drug use5. Newcombe defined harm reduction as a public health philosophy that defines policies, programs, services, and actions that work to reduce the health, social, and economic harm to individuals, communities, and society associated with the use of drugs6. Such a definition recognizes the harm associated with substance abuse and attempts to minimize its impact. Effective treatments can result in stabilization and reduction of harm to increase life expectancy or, more pragmatically, to save lives, increase the quality of life of drug abusers2, and reduce social and economic burdens, including public disturbances, loss of productivity due to unemployment, and crime. As a result of the urgent need to prevent HIV transmission among IDUs, essential prevention programs were developed and implemented in most Western European countries in the late 1980s (Figure 1)4.
In practice, harm reduction provides access to sterile needles/syringes and drug equipment, safe disposal, substitution maintenance treatment, outreach and peer support, as well as education and information on safer drug use, safer lifestyles, sex education, condom distribution, and HIV testing7. Below we discuss four forms of harm reduction already implemented and used for many years in different countries in Europe, Canada, and Australia.
Drug consumption rooms
One form of harm reduction currently in place in many countries in Europe is drug consumption in supervised settings, specifically drug consumption rooms (DCRs). DCRs are mostly funded by local or regional budgets or voluntary organizations8; they provide a supervised facility where drug users can bring street heroin and inject it in a safe and sterile environment under advice and instruction from trained staff. This promotes safer injection techniques and prevents the spread of infections and the occurrence of abscesses. Staff personnel, mostly social workers, physicians, nurses, and others trained in emergency aid10, are not permitted to help users inject the drug9, 10. Drug dealing is strictly prohibited, and other rules prohibiting antisocial behavior are commonly enforced in such drug consumption facilities10. Ideally, professional DCR staff educate users about disease and threats to their health resulting from drug use and help them find suitable treatment, especially for diseases such as HIV or hepatitis C. Additionally, DCR staff provide emergency aid in cases of overdose, likely the main cause of death among IDUs.
When heroin abuse in Europe began to expand appreciably, public health authorities were faced with increasing morbidity and mortality rates among IDUs. IDUs are one of the most at-risk groups for HIV and AIDS, and the real threat exists that HIV may be transmitted from IDUs to the normal population. Moreover, the public nuisance caused by IDUs injecting in public can be a large problem in cities with many drug users and drug user communities. Some IDUs dispose of their needles and other injection equipment in streets, school yards, or other public places where other people could be harmed. Because of these concerns and concerns about IDUs, especially high-risk and difficult-to-reach users, who are often in bad health and usually do not seek health services because of a fear of punishment or imprisonment, many countries in Europe have implemented DCRs. The first DCR was opened in Berne, Switzerland, in 1986. By 2004, 72 DCRs existed in 39 cities in Germany, Switzerland, Spain, and the Netherlands10.
To ensure that occasional drug users are not provided with opportunities to increase their drug use, DCRs employ certain admission criteria. These may include a minimum age (currently 18 years in most DCRs) and the exclusion of occasional or first-time users, with only regular and dependent users allowed9, 10.
Some DCRs offer additional services in order to reach special-needs and high-risk groups. These services include opening times for women only, temporary accommodations for users who are homeless, off-site recreational activities, parenting skills training, postal contact with prison inmates, and soft drinks, fruits and hot dishes10. DCRs can be viewed as a link to healthcare and can be considered as a first step to drug addiction treatment9.
The concept of DCRs is controversial, and overcoming the barriers to establish such facilities is often difficult, especially if police do not accept the concept. Agreements must be reached between the operator of the DCR and the police, and acceptance by local residents is also important. The German government, for example, had to make drastic changes to their existing narcotics laws to make DCRs possible11. In German cities that provide DCRs for IDUs, special agreements often prohibit the police from stepping inside the rooms for drug law enforcement purposes; in return, the facilities strive to allay the nuisance of IDUs and their negative impact on public order.
Although DCRs are perhaps not the ideal treatment, evidence indicates that they help to some extent; they decrease mortality among drug users and provide the opportunity to reach users who are not otherwise motivated to seek treatment. DCRs are a practical means of enabling drug users to survive, with the hope that at a later stage they will be able to cease drug use9.
Needle exchange and needle distribution
Sharing of injection equipment is very common among IDUs. One essential innovation of facing the HIV threat was the implementation of needle exchange programs. Its concept is the distribution of sterile needles and the safe disposal of used and contaminated needles in order to prevent the transmission of blood-borne viruses such as HIV4.
In 1993, Des Jarlais, Friedman, and Ward described needle exchange programs as “... the prototypical harm-reduction method for preventing HIV infection among IDUs”5. Needle exchange programs should always include an exchange of needles and not simply provide sterile needles. This concept is extremely important in order to avoid inappropriate disposal, which could result in transmission of infections not only to other IDUs, but also to the normal population5.
Because most needle exchanges occur face-to-face between the IDU and the distributor (eg, street worker, pharmacist), education about safer drug use, safer lifestyles, and the risks of HIV and other infections can easily be accomplished. Moreover, staff working in a needle exchange program can promote other forms of drug abuse treatment and can motivate users to initiate comprehensive healthcare5. Accordingly, needle exchange programs have a positive effect not only on the reduction of HIV but also the recruitment of IDUs into primary healthcare to begin drug abuse treatment5.
Another aspect of needle exchange programs is the use of vending machines, which provide a discreet way to obtain sterile needles for IDUs who wish to remain anonymous. Vending machines also help to create access to sterile injecting equipment in special geographical areas and during times of the day when other access is not available.
Needle exchange alone is not sufficient to prevent HIV infection; it should be regarded as a necessary, but only supplemental service fundamental to more comprehensive treatment12. Another problem is the accessibility and quality of the needles themselves. For example, some users may find it inconvenient to obtain sterile needles before using drugs. In addition, some users are not satisfied with the quality of the injection equipment (eg, too much drug is retained in the equipment and other reasons)13. Despite these disadvantages, however, needle exchange programs are necessary to achieve adequate harm reduction.
Substitution maintenance treatment
Substitution maintenance treatment is a form of drug abuse treatment in which a substitute for the main drug of abuse is offered to drug addicts6. Substitution drugs may be provided by general practitioners or by community-based outpatient clinics or pharmacies supervised by a physician or nurse6. Substances which are currently common for substitution maintenance treatment for opiate dependence include methadone, buprenorphine, dihydrocodeine, slow-release methadone, and pure heroin14.
Substitution maintenance treatment differs from substitution treatment used to reduce withdrawal after detoxification. Substitution detoxification treatment is a stepwise reduction of the drug quantity to zero6, whereas maintenance treatment prescribes the substitution drug (eg, methadone) as long as necessary to stabilize the patient's health status and achieve abstinence from the primary illegal drug. Such maintenance treatments may last 6 months or longer7.
Methadone, which blocks the euphoric effects of heroin, should be prescribed as a treatment for long-term heroin-dependent individuals as long as necessary to avoid relapse to illegal drug use1, 16. Methadone maintenance involves prescribed doses of liquid or pill-form methadone for treating opiate addiction, mostly in outpatient settings15. Methadone is taken orally once per day to stop or reduce the craving for opiates. Evidence shows that the retention rate of patients in methadone maintenance treatment is much higher than that of patients who obtain short-term methadone treatment after detoxification (76% retention with methadone maintenance vs 27% with methadone detoxification)17.
The doses of methadone administered during methadone maintenance treatment should be high enough to reduce risky and harmful behavior. While no agreed-upon standard exists for a minimum dose, tests have shown that a dosage above 50 mg is effective, whereas doses of 20 mg are ineffective1. Higher dosages are more effective at retaining patients than lower dosages1. In most countries, methadone is prescribed in dosages of 60–80 mg per day6.
Much evidence supports the effectiveness of methadone maintenance11. Most currently used substitutes are taken orally7. Methadone maintenance has been shown to reduce the risk of HIV/AIDS, hepatitis C, and other infectious diseases among IDUs15, 18. Methadone maintenance also can support the early diagnosis of health problems such as HIV/AIDS, because HIV testing can be provided. Moreover, methadone maintenance can reduce criminal activity among IDUs who are at a higher risk of being involved in crimes because of their extreme craving for heroin. Evidence indicates that substituted patients are less likely to be involved in crimes (3% involvement in crimes vs 12% among drug users without treatment)17. Furthermore, in a German study, 10% of patients who were in substitution maintenance programs became drug-free from both the primary and substitute drug19.
Maintenance treatment should include complementary psychological care to increase retention rates and achieve better long-term outcomes. Maintenance treatment combined with counseling is also more cost-effective than maintenance treatment alone19. Supplementary social services, such as assistance in returning to employment, are also recommended and are essential for ameliorating the harm associated with injected drug use.
Despite the demonstrated successes in some areas described above with respect to maintenance treatment, challenges remain regarding the accessibility of substitution maintenance treatment, especially in rural and other areas with an inadequate healthcare infrastructure. A second challenge is the provision of substitution maintenance treatment at a cost that healthcare systems, the community, and/or individuals are able to afford. Compliance may also be difficult due to the inconvenience for some patients of daily dosing. For this reason, drugs such as buprenorphine are sometimes considered better solutions than methadone, because they do not need to be taken daily20.
Peer support/self-help groups
In terms of heroin abuse harm reduction, peer support and peer education can be an effective supplement to other treatment11. Peer support can take many different forms, including peer education and self-help groups. Such groups can be anonymous drug user communities or autonomous drug user organizations. They may be initiated not only by professionals, but also by current users, ex-users, users under substitution maintenance treatment, family members, and others associated with the drug user. The theory behind peer support and education is that many drug users within a drug community may join together to imitate, encourage or criticize each other in a peer group21, an interaction that can be described as having a snowball effect21. The concept of peer support takes advantage of this peer effect to spread perspectives of safer drug use and to educate about the risks associated with drug use within a peer community.
Peer support can also educate about the risk of HIV and improve the health and social and mental condition of the drug user, while promoting safer drug use, safer sexual behavior, and, in some cases, abstinence. One important aspect of peer support is assisting drug users to find suitable treatment or providing support for drug users who are motivated to become abstinent. In this form of harm reduction, abstinence from or reduction of drug use is not the primary goal. Self-help groups are meant to be a non-judgmental platform where people can be honest about their drug use without stereotyping or criminalizing the behavior11, 15. Most self-help organizations dedicate themselves to promoting the same rights for drug users as for every human being and being more tolerant and accepting of policies focused on drug addiction. Their credo is that drug addiction should no longer be viewed merely as a crime, but as what it is already widely acknowledged to be — a severe, chronically relapsing disease. Self-help groups are often initiated by relatives of drug users who are afraid of, or lack knowledge about, the drug abuse of their loved one or who simply want to share their experiences with other parents or relatives. They emphasize the importance of reconstructing relationships with friends, family, and employers11, 15. Efforts are concentrated on the promotion of other social networks that do not support drug use11.
The advantages of peer support and self-help include the great efforts that are made to contact difficult-to-reach users, one special risk group that often has a higher risk of blood-borne viruses and infections and is often in bad health. Efforts should be made to make these people feel appreciated and comfortable in order to create a base from which to initiate treatment and to encourage their participation in short-term or long-term abstinence-oriented programs11. Providing drug user communities with peer outreach workers who are former or current drug users can provide extra benefit to these communities resulting from greater knowledge of the risks of HIV and safer injecting techniques (eg, how to clean needles, how to gain access to sterile needles, how to increase condom use, and how to decrease drug use).
One problem that may occur which could hinder the public's acceptance of self-help is the risk of policy makers being accused of promoting drug use. Self-help organizations are sometimes overly rigorous in claiming rights and changes in policy, such as promoting the legalization of drugs of abuse. As mentioned above, peer support is not always only abstinence oriented, and this often results in difficulties concerning acceptance of this kind of treatment. Therefore, self-help organizations should be mindful of their philosophies and aims and should be extremely sensitive when promoting them to the (mostly critical) public.
Peer support is designed to reach drug users who are difficult to persuade to seek drug abuse treatment and who are, in addition, often highly vulnerable because of their life situations (eg, homelessness or being a sex worker). Drug users who are not aware of drug abuse treatment because they are either afraid or simply not interested in receiving help can receive advice about how to take the first step into treatment. Peer support and especially self-help should be given greater consideration in terms of effective, comprehensive harm-reduction treatments 11.
Drug abuse and harm reduction in China
Drug abuse and HIV epidemiology in China
The establishment of the People's Republic of China in 1949 resulted in a drug-free society and the absolute disappearance of illicit drug abuse that lasted for decades22. However, with the establishment of China's open-door policy in the late 1980s, the drug problem reappeared. At that time, most drug abusers were young, poor farmers from the southwest and rural areas in the northwest23. However, in the early 1990s, drug abuse in China quickly spread to epidemic proportions. With the frequent drug trafficking in the Golden Triangle region, heroin abuse gradually became the most potent issue with regard to illicit drugs24.
In China, 1.16 million drug abusers were registered at the end of 2006; however, the actual number of drug-dependent individuals is estimated to be 3.5 million20, 25, 26. Approximately 700 000 heroin-dependent individuals account for 78.3% of total drug abusers27. In some provinces, such as Yunnan, Sichuan, Guangxi, and Guangdong, the prevalence of heroin addiction is even higher. The most frequent route of drug administration is intravenous injection (50% to 70%). Although snorting (55%) and smoking (8%) heroin are common, most users eventually migrate to intravenous as the preferred route of administration in order to achieve the same effect at lower doses22, 28, 29, 30.
Since the late 1990s, the abuse of new types of drugs in China, mainly amphetamine-type stimulants and other chemically related synthetic drugs, including amphetamine, methamphetamine, and 3,4-methylenedioxymethamphetamine (MDMA; ecstasy)31, has increased. Recent years have seen a rapid increase in the popularity of amphetamine-type stimulants and MDMA in nightclubs in southeastern cities and business-centered cities23. However, heroin remains the primary abused drug which causes the most severe health and social problems.
Drug abuse leads to a high prevalence of HIV/AIDS because HIV can be transmitted quickly among IDUs (Figure 2). The first AIDS case was reported in China in 1985, and the first drug-related HIV infection was reported in Yunnan Province as early as 198932. Approximately 650 000 people in China were living with HIV in 2005, and IDUs account for almost half (44%) of the people living with HIV33. In November 2007, China reportedly had 223 501 HIV-infected individuals, including 62 838 AIDS cases, 22 205 of whom died. Injecting drugs and sharing needles account for transmission of 42% of HIV/AIDS in China34.
Because 85% of all drug users prefer heroin over other kinds of drugs and injection is the most common route of administration35, comprehensive treatment is needed to prevent or reduce the harm that occurs as a result of high-risk behaviors such as needle sharing 32.
Methadone maintenance treatment in China
Methadone has been used for short-term detoxification in China since 199336. Because regular abstinence-oriented treatments such as compulsory rehabilitation centers or reeducation-through-labor camps have very high relapse rates and appear to be ineffective in keeping patients drug-free37, harm reduction may be an inevitable approach in the fight against HIV and other harm associated with injected drug use. Long-term methadone therapy began in 2002 for research purposes in high-prevalence provinces and large cities such as Beijing; the first eight methadone maintenance clinics were established in early 200436. Methadone maintenance in China was implemented mainly to control and prevent the transmission of HIV. One study showed that the percentages of patients infected with HIV (3.9%) or hepatitis C (46%) did not increase with methadone maintenance treatment18, and evidence indicated that methadone maintenance could reduce the protracted symptoms of heroin abstinence18. Today, the emphasis of treatment is moving more toward reducing illegal drug use in general. An estimated 47 427 cases were being treated in August 2007, and the number of clinics will likely reach 500 by the end of 200737. Currently, a rapid scale-up of methadone maintenance clinics is occurring in China, and the central government plans to serve 200 000 patients by 201038. Moreover, harm-reduction efforts are being concentrated on methadone maintenance treatment in urban areas in order to better control crime and reduce other harm associated with drug use18, 38.
In China, methadone is being administered as a green liquid solution39 as a symbol of hope for patients. The price for a daily dose of methadone is RMB1037, regardless of how high the individual dose for the patient might be. Participants in methadone maintenance programs in Beijing, for example, pay RMB300 in advance for an entire month of treatment. Doses range from 30 to 40 mg in the initial phase and are adjusted individually without a maximum limit due to the level of opiate dependence after a few weeks. In one of Beijing's methadone maintenance facilities, the highest daily dose was 135 mg, indicating no clear differences in dosages compared with other countries. Normally, patients must sign a form before obtaining their individually adjusted dose of methadone and can easily enter the clinic without undergoing a lengthy procedure.
Admission requirements can differ slightly from site to site, but for most clinics the patient has to meet four criteria37: be a local resident, have already gone through forced detoxification, be a minimum age of 18 or 20 years, and have a good civil character. People living with HIV/AIDS are usually admitted after meeting only one or two of the criteria, and if they cannot otherwise afford treatment, they are qualified to have their treatment paid from government funds. Additionally, the requirements for entrance into methadone maintenance programs have relaxed to encourage greater access. For example, patients are sometimes not required to be local residents or to have completed internment in a detoxification center32. Urine testing for HIV, sexually transmitted diseases, hepatitis, and current use of illegal drugs are undertaken before the patients enter the program and are conducted randomly during treatment. Three drug-positive samples generally lead to exclusion from the program.
In order to increase the quality of methadone maintenance programs, some critical points need to be addressed. First, although studies indicate that methadone maintenance combined with psychosocial services is more effective in retaining patients, decreasing relapse rates, and reducing costs11, 24 than maintenance treatment alone, no standardized comprehensive psychotherapeutic service or counseling is available for patients. Fortunately, some methadone maintenance clinics in Beijing have begun offering voluntary counseling for patients twice per week. Most clinics in Beijing now regularly organize occasional outdoor activities, group meetings, and discussions based on the DAYTOP model, in which problems and fears can be discussed through peer support. Another critical point is that patients entering methadone maintenance programs need to be registered; the collection of individual data from each patient by the staff may be a deterrent for some drug abusers who are afraid of punishment. Moreover, the strict criteria for entering the program might themselves be a deterrent for some patients. In Beijing, some clinics have begun admitting patients who are under 20 years of age, and some clinics are not obligated to report patients to the police who are drug-positive for a third time. Methadone maintenance clinics operated by the local Centers for Disease Control (CDC) try to retain patients after the third positive urine sample, while warning them that they might be eliminated from the program if they do not stop taking drugs. Clinics operated by law enforcement are likely to be stricter and less able to deviate from official guidelines than facilities that are operated by the CDC.
China's response to HIV among IDUs is rapidly developing, and policy is becoming more liberal and pragmatic. However, coverage of drug abusers in China by methadone maintenance clinics remains low, and plans for the future are based on miscalculated prevalence rates40.
Needle exchange in China
Sharing injection equipment is very common among drug users in China and accounts for more than half of the HIV cases in China35. Needle exchange programs in China are not developing as quickly as methadone maintenance programs because many drug abuse authorities have the common opinion that providing needles encourages drug use32, 37. As a result, needle exchange programs are not officially endorsed by the Ministry for Public Security. Because of this, conflicts between outreach workers and police sometimes occur38. Therefore, the government used the term “needle social marketing” in its initial phase, which in fact means increasing the commercial accessibility of needles, whereas in some parts of China sterile needles are provided for free32. Needle distribution is conducted mainly through outreach workers who are former drug users. The government plans to open 1,400 needle exchange programs to serve 70 000 drug users by the end of 200837. By 2010, coverage of IDUs should reach 50%32, 37. Law enforcement and participants in needle exchange promotion, education, and distribution should increase their communication and cooperate to avoid conflicts and enhance the effectiveness of these programs.
Non-governmental organizations (NGOs) in China
NGOs in China play an important role by filling the gaps in reaching high-risk populations in the fight against HIV41. In particular, those segments of the population that are afraid of interacting with governmental organizations can receive help from national and international NGOs37, 42.
The work of NGOs varies from prevention to education to research. For example, NGOs print and distribute educational material about health issues, organize outreach work for drug communities, organize public awareness events, cooperate with other NGOs in China, and fight for the rights of people living with HIV/AIDS41. NGOs have played a key role in initiating needle exchange programs in China. Of the current programs, 50% have been supported by funds from international organizations37.
Due to China's legal framework, NGOs are slightly different from those in other countries because they remain connected to the government (eg, for their funding). As a result, the Chinese NGO model can be described as a semi-NGO or government-organized nongovernmental organization. However, terminology can vary from nonprofit organization to foundation to social organization32, 37.
In late 2007, the financially strong Bill and Melinda Gates Foundation entered China with a budget of US$50 million and plans to work together with the government and NGOs to expand HIV-prevention efforts. One of their main goals was to reach vulnerable high-risk populations, including IDUs, sex workers, and homosexuals43.
NGOs and peer-outreach programs should be given greater consideration in terms of comprehensive treatment and are a key strategy for reaching drug abusers who are marginalized or stigmatized37.
HIV testing in China
Widespread HIV testing to make people who are infected with HIV aware of their serostatus is very important in the fight against HIV, especially in China, where knowledge about HIV/AIDS is very poor37. HIV awareness is important for two main reasons. First, it is a gateway to gain access to treatment. Second, it helps to prevent transmission to other people42. Hindering effective HIV awareness is the widespread opinion in China that individuals who are infected with HIV come from lower classes or are involved in criminal activity42. This stigma can result in major barriers to voluntary testing36.
In China, institutional settings for HIV testing, such as Compulsory Rehabilitation Centres (CRCs) and prisons, are part of a routine procedure, and refusal is not possible42. More than 3000 voluntary HIV testing centers are being opened in high-prevalence provinces with help from the government37. At the end of 2005, the free anti-retroviral treatment (ART) program served 20 453 AIDS patients, including approximately 17 000 former plasma donors, 600 drug users, and 100 homosexuals42.
In conclusion, the most important challenge facing us today is to make comprehensive harm-reduction programs more widely accessible to a greater percentage of drug abusers in order to achieve the aims of harm reduction.
Implications of harm reduction in China
With the Chinese government paying more attention to the burden and threat of HIV/AIDS in recent years, the implementation of harm-reduction programs has increased. Positive developments in harm reduction in China are efforts being made by the central government, such as outlawing discrimination against HIV-infected individuals11 and media campaigns to increase awareness of HIV risks and promote HIV testing. Yet some limitations remain.
Only a few forms of harm-reduction program exist for drug abusers in China. Because of the relatively recent recognition of the concept of harm reduction, approaches such as maintenance with buprenorphine or supervised DCRs have not been established. Facing the significant reemergence of drug use in the past two decades and the alarming threat of HIV, the Chinese government needs to continually reassess its current forms of drug abuse treatment. Under pressures from international experts who call for more practical treatment, and with predictions of increasing numbers of HIV patients in China in the upcoming years, a rush is occurring to implement harm-reduction programs for drug abusers. Rather than precipitously rushing development, however, more research should be conducted to improve the quality of treatment; otherwise, the effectiveness of such programs might suffer. Moreover, China needs to change the widespread opinion that drug abusers are delinquent persons who need correction rather than patients suffering from a severe chronic mental disorder44. Efforts should be concentrated on promoting HIV testing and promoting the more liberal handling of drug abuse issues. Problems also occur in the coordination of and cooperation between different participants in drug abuse policy and treatment. For example, law enforcement should increasingly cooperate with health authorities and outreach workers to avoid conflict.
Controversies about harm reduction and prevention exist worldwide. The significant threat of HIV and other harm among IDUs needs to be faced without necessarily criminalizing drug addiction, but such efforts have been accused of promoting drug use, thus making harm-reduction implementation difficult. Harm reduction as a public health issue must include many different aspects, activities, and people, including primary prevention, outreach workers, family members, and the drug users themselves.
For over 20 years harm-reduction programs have been used in Europe and other parts of the world and are becoming more popular and important in developing countries. Harm reduction continues to be an ongoing process, which still needs improvement. Its ultimate goal is to help drug users survive not only to achieve their next step in treatment, but also to attain long-term abstinence.
References
Simoens S, Matheson C, Bond C, Inkster K, Ludbrook A . The effectiveness of community maintenance with methadone or buprenorphine for treating opiate dependence. Br J Gen Pract 2005; 55: 139–46.
Joint United Nations Programme on HIV/AIDS. 2006 Report on the global AIDS epidemic. Geneva: UNAIDS; 2006.
Ball AL . HIV, injecting drug use and harm reduction: a public health response. Addiction 2007; 102: 684–90.
Vlahov D, Des Jarlais DC, Goosby E, Hollinger PC, Lurie PG, Shriver MD, et al. Needle exchange programs for the prevention of human immunodeficiency virus infection: epidemiology and policy. Am J Epidemiol 2001; 154 (12 suppl): S70–7.
Des Jarlais DC, Friedman SR, Ward TP . Harm reduction: a public health response to the AIDS epidemic among injecting drug users. Annu Rev Public Health 1993; 14: 413–50.
European Monitoring Centre for Drugs and Drug Addiction. Drugs in focus: key role of substitution in drug treatment. Luxembourg: Office for Official Publications of the European Communities; 2002.
World Health Organization, United Nations Office on Drugs and Crime. Joint United Nations Programme on HIV/AIDS. Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention. Geneva: World Health Organization; 2004.
Kimber J, Dolan K, Wodak A . Survey of drug consumption rooms: service delivery and perceived public health and amenity impact. Drug Alcohol Rev 2005; 24: 21–4.
Cruz MF, Patra J, Fischer B, Rehm J, Kalousek K . Public opinion towards supervised injection facilities and heroin-assisted treatment in Ontario, Canada. Int J Drug Policy 2007; 18: 54–61.
Hedrich D . European report on drug consumption rooms. Luxembourg: Office for Official Publications of the European Communities; 2004.
Michels II, Stover H, Gerlach R . Substitution treatment for opioid addicts in Germany. Harm Reduct J 2007; 4: 5.
Aceijas C, Stimson GV, Hickman M, Rhodes T . Global overview of injecting drug use and HIV infection among injecting drug users. AIDS 2004; 18: 2295–303.
Morissette C, Cox J, De P, Tremblay C, Roy E, Allard R, et al. Minimal uptake of sterile drug preparation equipment in a predominantly cocaine injecting population: implications for HIV and hepatitis C prevention. Int J Drug Policy 2007; 18: 204–12.
O'Hare PA . The reduction of drug related harm. London: Routledge; 1992.
Wodak A, Cooney A . Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. Geneva: World Health Organization; 2004.
Ward J, Hall W, Mattick RP . Role of maintenance treatment in opioid dependence. Lancet 1999; 353: 221–6.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP . An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abuse Treat 2005; 28: 321–9.
Shi J, Zhao L, Epstein D, Zhao C, Shuai Y, Yan B, et al. The effect of methadone maintenance on HIV and HCV infection, health status, employment, and criminal activity among heroin abusers during six months of treatment in China. J Addict Med 2007; 1: 186–90.
Kraft MK, Rothbard AB, Hadley TR, McLellan AT, Asch DA . Are supplementary services provided during methadone maintenance really cost-effective? Am J Psychiatry 1997; 154: 1214–9.
Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE . A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. N Engl J Med 2000; 343: 1290–7.
Trautmann F, Barendregt C . The European peer support manual: peer support as a method for AIDS prevention in injecting drug user communities. Utrecht: NIAD; 1994.
Fang YX, Wang YB, Shi J, Liu ZM, Lu L . Recent trends in drug abuse in China. Acta Pharmacol Sin 2006; 27: 140–4.
Michels I, Zhao M, Lu L . Drug abuse and its treatment in China. German J Addict 2007; 53: 228–37.
Lu L, Fang Y, Wang X . Drug abuse in China: past, present and future. Cell Mol Neurobiol 2008; 28: 479–90.
UNAIDS Asia Pacific Intercountry Team, United Nations International Drug Control Programme, Regional Centre for East Asia and the Pacific. Drug use and HIV vulnerability: policy research study in Asia. Bangkok: Joint United Nations Programme on HIV/AIDS; 2000.
Li XJ, Kusagawa S, Xia X, Yang C, Wang Q, Yokota Y, et al. Molecular epidemiology of the heterosexual HIV-1 transmission in Kunming, Yunnan Province of China suggests origin from the local IDU epidemic. AIDS Res Hum Retroviruses 2005; 21: 977–80.
Fengrui Y . Annual Report on Drug Control in China. Beijing: National Narcotics Control Commission; 2006.
Li X, Zhou Y, Stanton B . Illicit drug initiation among institutionalized drug users in China. Addiction 2002; 97: 575–82.
State Council AIDS Working Committee Office, UN Theme Group on HIV/AIDS in China. A joint assessment of HIV/AIDS prevention, treatment and care in China (2004). Beijing: State Council AIDS Working Committee Office, UN Theme Group on AIDS in China; 2004.
Ministry of Health of China, National Center for AIDS Prevention and Control, Collaboration Group for National HIV Sentinel Surveillance Program. Set up of national sentinel surveillance of HIV infection in China and its report in 1995. Zhongguo Xing Bing Ai Zi Bing Fang Zhi 1996; 2: 193–7.
Kulsudjarit K . Drug problem in southeast and southwest Asia. Ann N Y Acad Sci 2004; 1025: 446–57.
Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R . Evolution of China's response to HIV/AIDS. Lancet 2007; 369: 679–90.
Ministry of Health, Joint United Nations Programme on HIV/AIDS, World Health Organization. 2005 update on the HIV/AIDS epidemic and response in China. Beijing: National Center for AIDS/STD Prevention and Control, China CDC; 2006.
Lu L, Wang X . Drug addiction in China. Ann N Y Acad Sci 2008; 1141: 304–17.
Qian HZ, Vermund SH, Wang N . Risk of HIV/AIDS in China: subpopulations of special importance. Sex Transm Infect 2005; 81: 442–7.
Tang YL, Zhao D, Zhao C, Cubells JF . Opiate addiction in China: current situation and treatments. Addiction 2006; 101: 657–65.
Sullivan SG, Wu Z . Rapid scale up of harm reduction in China. Int J Drug Policy 2007; 18: 118–28.
Open Society Institute, International Harm Reduction Association. Harm reduction developments 2005: countries with injection-driven HIV epidemics. New York: Open Society Institute; 2006.
Humeniuk R, Ali R . The first methadone clinic in Beijing. Drug Alcohol Rev 2005; 24: 285–7.
Kosten TR, Gardner TJ . China's new march forward in addiction treatment: methadone for the masses: 2. Issues in formulating DSM V. Am J Drug Alcohol Abuse 2008; 34: 123–6.
Chen HT, Liao Q . A pilot study of the NGO-based relational intervention model for HIV prevention among drug users in China. AIDS Educ Prev 2005; 17: 503–14.
Wu Z, Sun X, Sullivan SG, Detels R . Public health: HIV testing in China. Science 2006; 312: 1475–6.
Walker R . Gates Foundation commits to expansion of HIV prevention in China. AIDS Portal [http://www.aidsportal.org/News_Details.aspx?ID=6337; accessed December 24, 2008].
Tang YL, Wiste A, Mao PX, Hou YZ . Attitudes, knowledge, and perceptions of Chinese doctors toward drug abuse. J Subst Abuse Treat 2005; 29: 215–20.
Acknowledgements
This work was supported in part by the 11th 5-year program of the Chinese Ministry of Science and Technology (No 2008zx10102), National Basic Research Program of China (No 2003CB 515400) and the China-Canada Joint Health Research Program (No 30611120528).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meise, M., Wang, X., Sauter, ML. et al. Harm reduction for injecting opiate users: an update and implications in China. Acta Pharmacol Sin 30, 513–521 (2009). https://doi.org/10.1038/aps.2009.30
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.30
Keywords
This article is cited by
-
Referring heroin users from compulsory detoxification centers to community methadone maintenance treatment: a comparison of three models
BMC Public Health (2013)
-
Hydrocarbon accumulation mechanism and structure of large-scale volcanic weathering crust of the Carboniferous in northern Xinjiang, China
Science China Earth Sciences (2012)